Translate this page into:
Re-tensioning of the medial collateral ligament
*Corresponding author: Márcio Balbinotti Ferrari, Department of Orthopaedics, Hospital de Clinicas de Porto Alere, Porto Alegre, Brazil. mb.ferrari@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ellera Gomes J, Vicioli C, Vieira de Castro J, Ferrari MB. Re-tensioning of the medial collateral ligament. J Musculoskelet Surg Res. doi: 10.25259/JMSR_85_2025
Abstract
Medial collateral ligament (MCL) injuries, especially in young active patients, can be particularly limiting, resulting in valgus laxity and overall instability of the knee in some cases. Although conservative management of this injury has demonstrated positive outcomes and the return to the pre-injury level of sport, surgery may be performed in cases of chronic and symptomatic MCL injuries that do not respond to non-operative management. In this technical note, we describe our preferred method for treating chronic MCL laxity associated with symptomatic valgus abnormality and re-tensioning the ligament through trephination of the tibia.
Keywords
Knee joint
Ligaments
Medial collateral ligament
Sports injuries
Valgus instability
INTRODUCTION
The principal ligaments on the medial aspect of the knee are composed of the superficial medial collateral ligament (sMCL), the deep medial collateral ligament (MCL), and the posterior oblique ligament (POL).[1,2] sMCL injury is the most common of all knee ligamentous structures.[2] Often, these injuries occur during participation in a contact sport and are more commonly seen in young and active male patients.[1,2]
The sMCL is the largest ligament found on the medial side of the knee and is composed of one femoral origin and two tibial attachments.[3] Cavaignac et al.[4] performed a cadaveric study to evaluate the deep MCL and found that the isolated sectioning of this portion of the MCL was associated with an increase in knee internal and external rotation, with the greatest amount of rotation found at 30° of flexion and extension. Furthermore, Robinson et al.[5] reported that the deep MCL is a secondary restraint to valgus. However, as long as the sMCL remains intact, no significant changes in valgus laxity are seen, regardless of the deep MCL.
Most patients with MCL injuries can be successfully treated through conservative measures and return to pre-injury activity without sequelae.[1] Nevertheless, surgery may be necessary in cases of high-grade MCL tears, as well as an MCL tear combined with a multi-ligament knee injury.[1] In cases with chronic laxity and symptomatic valgus abnormality, which occurs as a result of MCL injury, surgical treatment may be indicated.[1] This technical note aimed to describe our preferred method to address MCL laxity through re-tensioning of the ligament by way of trephination of the neighboring aspect of the tibia.
SURGICAL TECHNIQUE
Pre-operative setup
The patient is placed supine, and a thorough knee physical examination under anesthesia is routinely performed, evaluating the varus/valgus laxity as well as rotatory instability, particularly through the anteromedial drawer. The valgus and varus stress tests are performed at 30º of knee flexion as well as at full extension in order to evaluate the extent of the injury to the medial side. We suggest performing the physical exam on both knees, with the contralateral, uninjured knee serving as the reference for normal laxity values. Once the tests are performed, a tourniquet is secured on the proximal aspect of the surgical limb. The knee is then prepared and draped in a standard sterile fashion, and the tourniquet is inflated to 250–350 mm Hg to begin the procedure.
Approach and incision
To ensure the correct position of the incision, we use a variety of bony landmarks, including the patellar inferior pole, the medial femoral condyle, the medial tibial plateau rim, and the tibial tuberosity. Using these landmarks as our guide and according to the surgeon’s preference, a surgical pen may be used to outline any relevant bony landmarks for easier identification throughout the procedure. An 8 cm curved incision is performed on the medial side of the proximal tibia, beginning at 1 cm distal to the inferior pole of the patella. Following this, the subcutaneous tissue is carefully dissected using Metzenbaum scissors, taking care to avoid damage to the saphenous vein and nerve. Once adequately exposed, the hamstring and semimembranosus tendons are identified, and a longitudinal 5 cm incision is performed on the superficial layer of the MCL. Following this, a subperiosteal detachment is performed, specifically on the posteromedial aspect of the ligament [Figure 1].
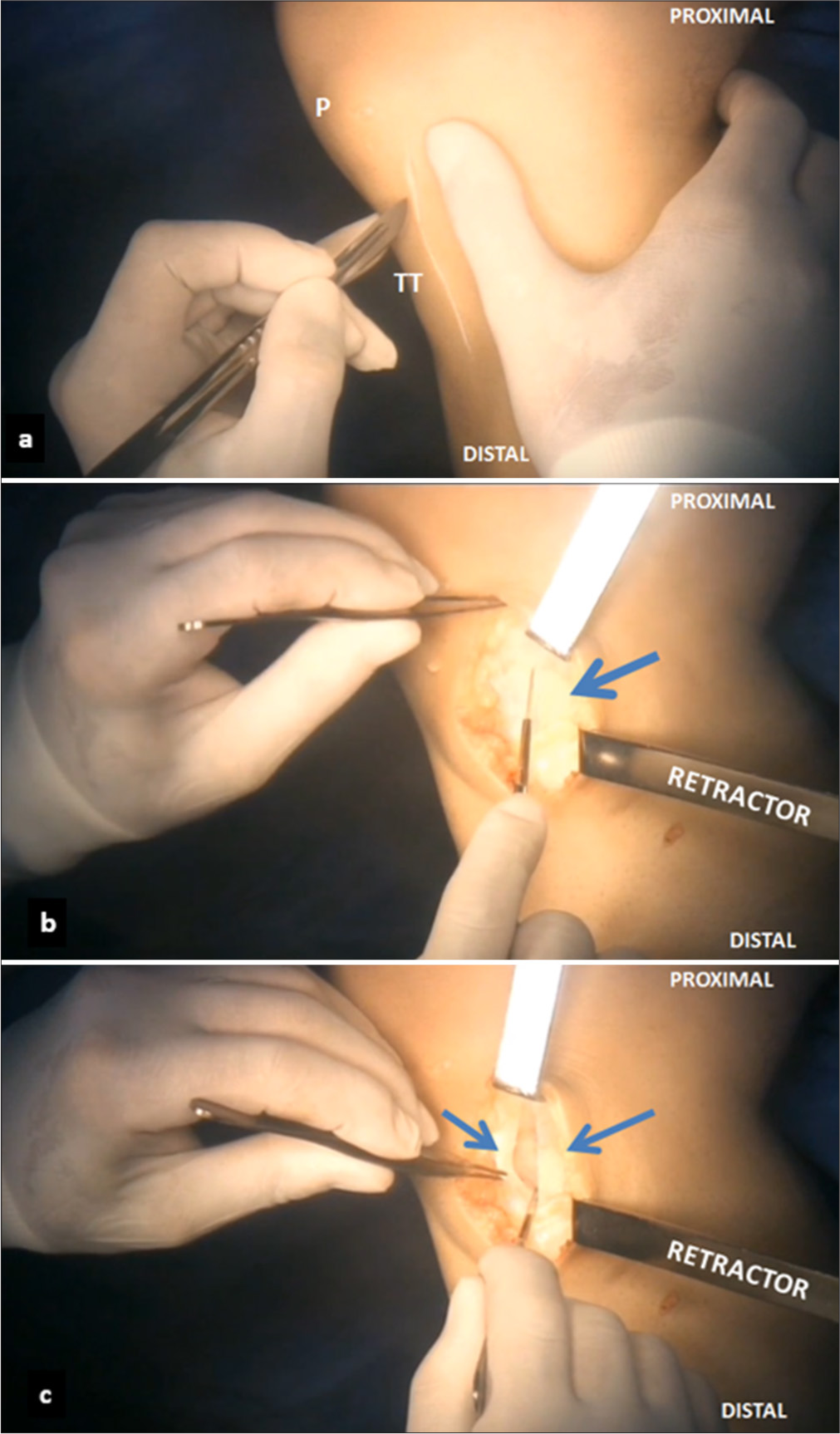
- (a) An 8 cm incision is made on the proximal medial tibia, starting 1 cm distal to the inferior pole of the P. (b) The medial collateral ligament (blue arrow) is exposed. (c) A 5 cm longitudinal incision is made along the superficial layer of the ligament (blue arrows). P: Patella, TT: Tibial tuberosity.
Trephination
A cannulated trephine made up of a cylinder with a small peg at one end and the actual trephine, which encloses the cylinder, designed by the senior author (JLEG), is used to remove a rounded plug of bone 1.2 cm wide from the medial condyle of the tibia [Figure 2]. The cylinder with the small peg is first hammered into the location directly between the semitendinosus and semimembranosus tendons, with the peg hitting against the tibia to create the indentation that will guide the trephination technique. At the site of this initial indentation, a 4.5 mm drill is used to perforate the tibial cortex directly perpendicular to the tibial axis, creating a unicortical hole. The peg of the cylinder is then inserted into the newly formed unicortical hole and will remain in this position during trephination. Once the cylinder is in place, the trephine, which encloses the cylinder, is situated at the trephination site. The trephine is then drilled down, as the cylinder helps maintain a steady position, to obtain the 1.2 cm wide bone plug to be used for re-tensioning of the MCL [Figure 3]. Once drilling is complete, the plug is removed using a 4.5 mm cortical screw (DePuy Synthes, Raynham, MA), which is inserted into the previously drilled 4.5 mm hole. Following this, the opposite cortex of the tibia is drilled with a 3.2 mm drill perpendicularly to the tibial axis. Once completed, the tunnel is measured, and then, a 4.5 mm trephine is used (DePuy Synthes, Raynham, MA). The correct size of the 4.5 mm cortical lag screw (DePuy Synthes, Raynham, MA) is then selected based on the previous measurement.
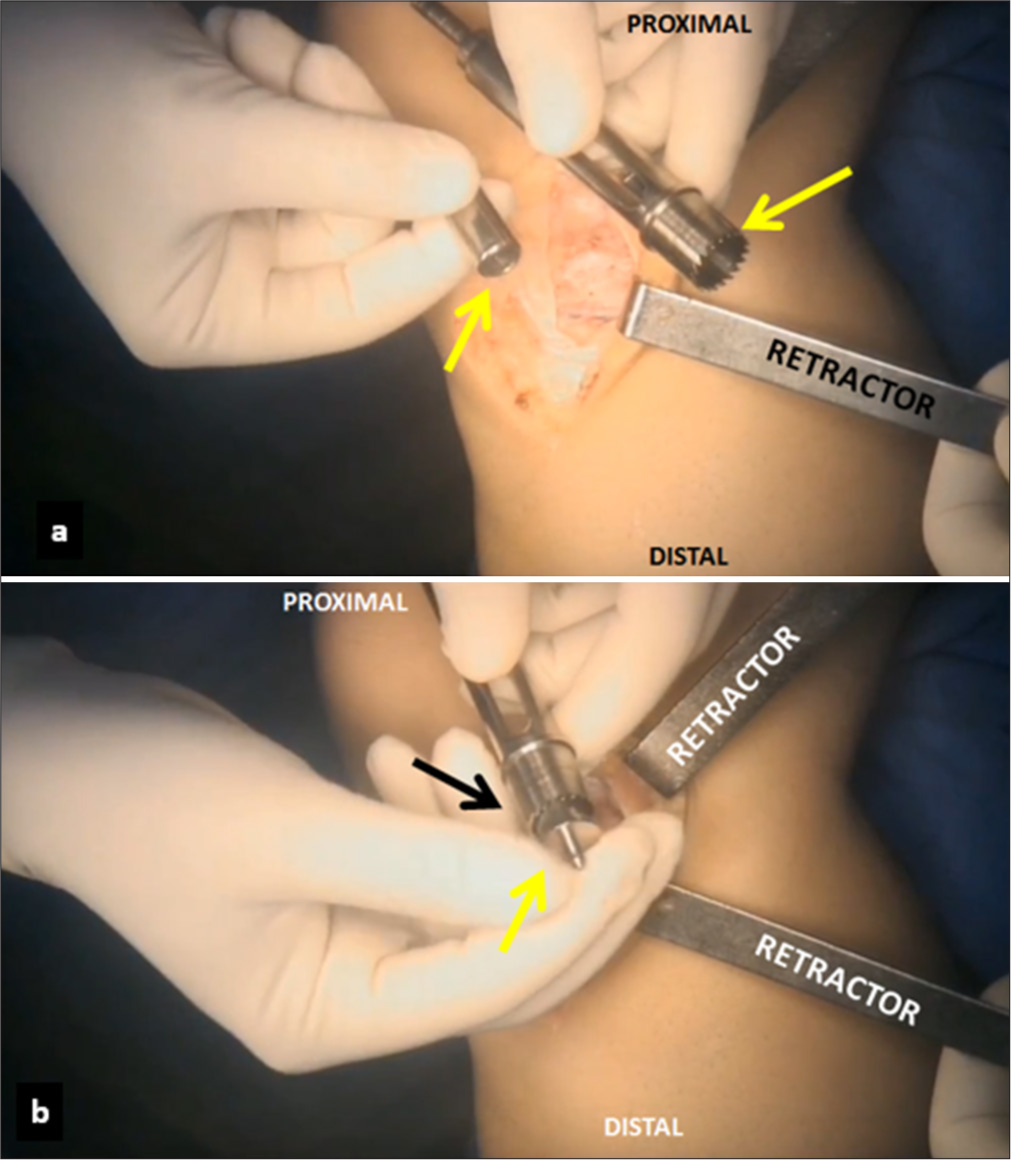
- (a) A specially designed cannulated trephine (yellow arrows) is used to remove a 1.2 cm wide bone plug from the right knee. (b) A cylinder with the small peg (yellow arrow) is inserted into the unicortical hole (black arrow). The trephine is placed underneath the medial collateral ligament, and the tibial cortex is perforated perpendicular to the tibial axis.
- The 1.2 cm wide bony plug (black arrow) is removed from the proximal tibia using a cortical screw (yellow arrow).
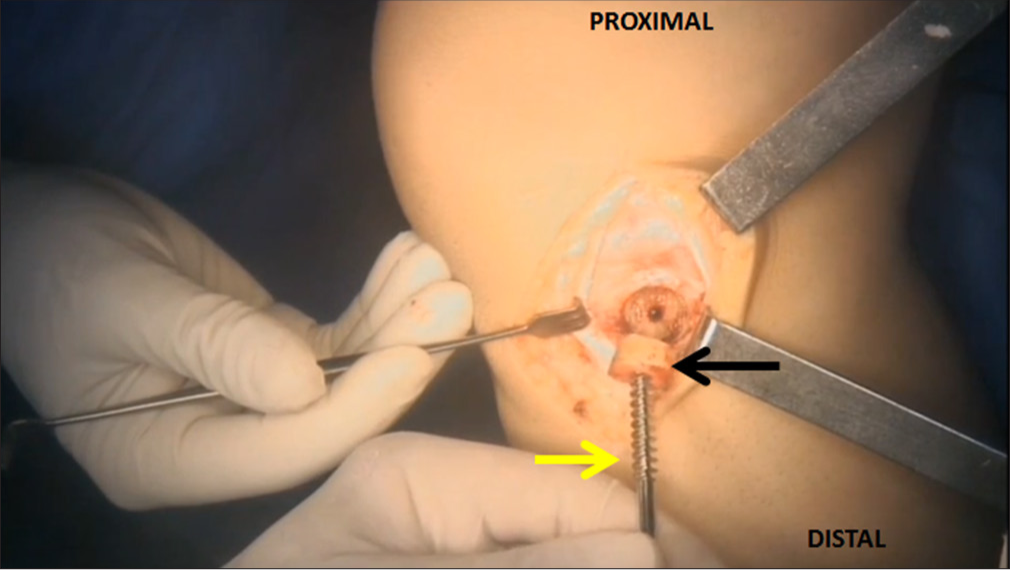
Re-tensioning of the sMCL
The knee is positioned at 45° of flexion, and the surgeon’s assistant applies a slight varus force. The posterior part of the sMCL is then tensioned anteriorly and distally to correct for prior laxity. Kocher clamps placed on the superior and inferior aspects of the ligament supply the tension needed during this portion of the technique. Then, an incision is made 1 cm medially from the initial incision on the MCL [Figure 4]. Following this, the cortical lag screw (DePuy Synthes, Raynham, MA) with a metal washer (DePuy Synthes, Raynham, MA) is drilled through the newly created incision and into the previously drilled hole with a standard screwdriver. It is crucial to completely introduce the bone plug into its native location while maintaining the MCL secure and appropriately tensioned. Once the bone plug has been driven all the way down with the MCL underneath, the knee is extended, and a valgus stress test is performed to verify the procedure’s effectiveness. Following this initial test, the knee is assessed for any signs of rotational instability.
- (a) After the removal of the bone plug, a small incision (white arrow) is made 1 cm medially from the initial incision (black arrow). (b) The medial collateral ligament is re-tensioned with Kocher clamps. A 4.5 mm cortical screw (black arrow) is inserted through the bone plug into the created defect (blue arrow). (c) The final view shows successfully implemented cortical screw and washer (black arrow). P: Patella.
Wound closure
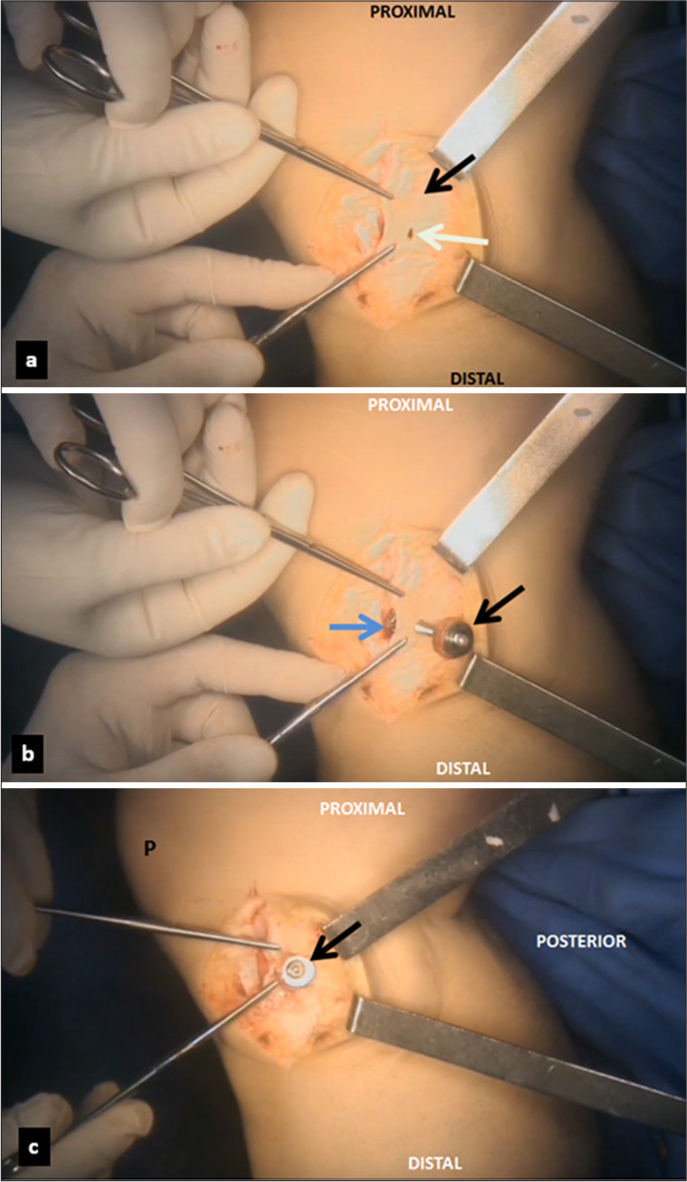
Once trephination and re-tensioning of the MCL are complete, a thorough irrigation with saline solution is performed. A combination of ropivacaine 7.5 mg/mL (20 mL) and epinephrine (2 mL) is also mixed into the irrigation solution to minimize post-operative bleeding. The tourniquet is released, and hemostasis is achieved using a coagulator. A non-absorbable #2 Ethibond 2–0 suture (Ethicon, Somerville, NJ) is then used to close the initial incision on the MCL [Figure 5]. Afterward, the subcutaneous tissue layer is closed using #2.0 Vycril sutures (Ethicon, Somerville, NJ) and the skin layer is closed in a standard fashion using # 4-0 Mononylon suture (Ethicon, Somerville, NJ). Post-operative knee radiographs are performed to verify the fixation [Figure 6].
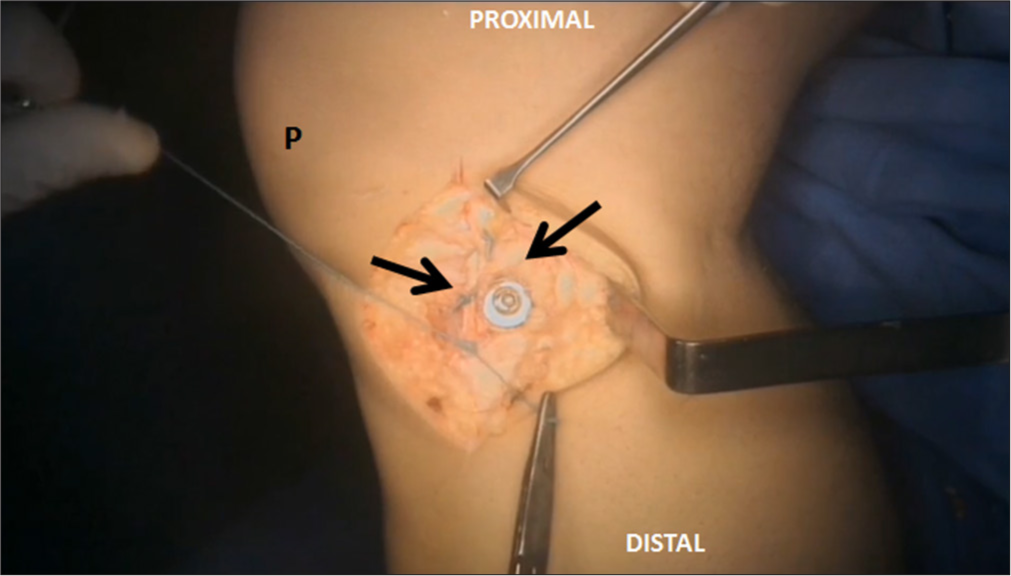
- Once the fixation of the medial collateral ligament (black arrows) is complete, the 5 cm incision is closed using absorbable sutures. P: Patella.
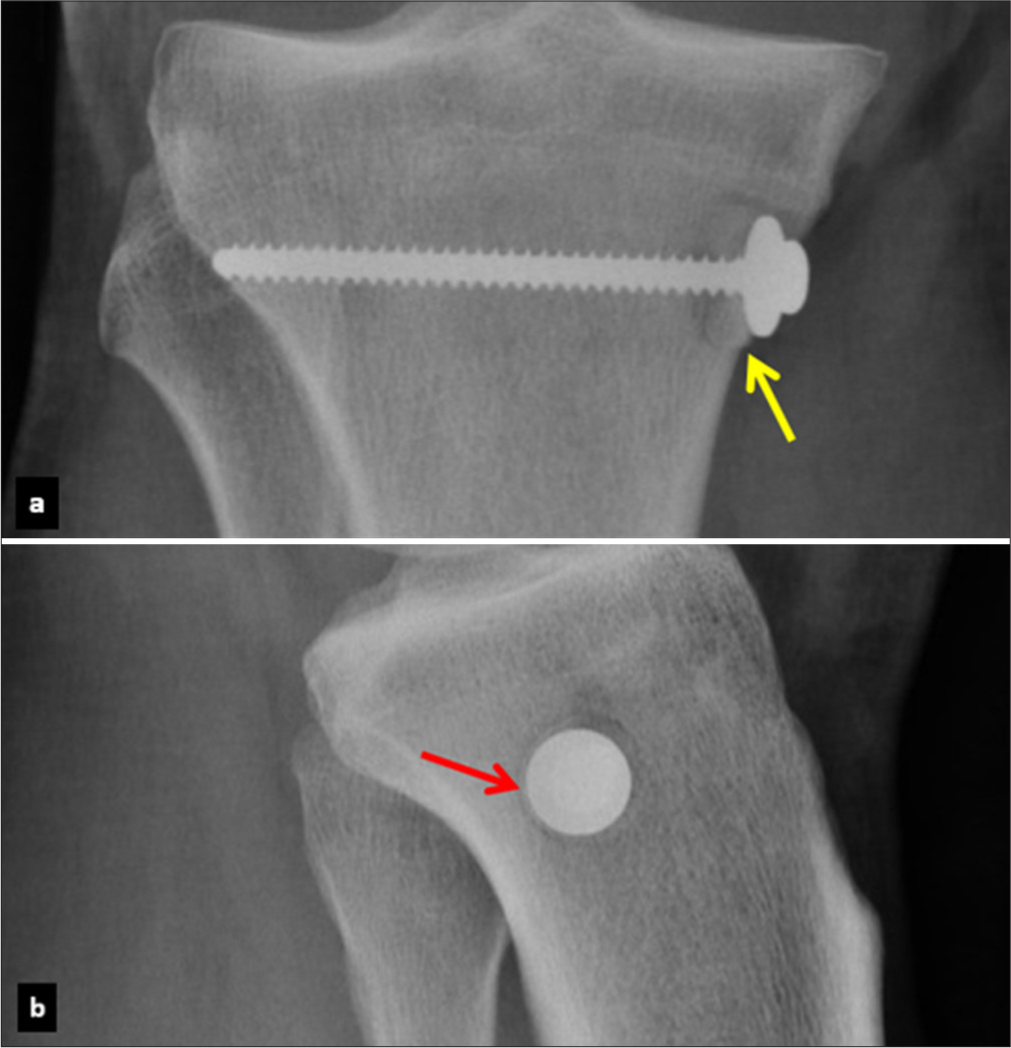
- Radiographic images in the (a) anteroposterior and (b) lateral views of the right knee, demonstrating successful fixation of the bone plug (yellow arrow). Note the perpendicular insertion of the screw (red arrow).
POST-OPERATIVE PROTOCOL
A long knee brace set at 15° of flexion is used for the 1st 7 days to protect the construct. Following this period, a full range of motion and weight bearing is encouraged at the patient’s discretion. However, we suggest using crutches for balance during this rehabilitation portion. Physical therapy begins after the first week and continues for the first three months. The progression of the physical therapy program is tailored for each patient based on their pain and knee swelling. Ultimately, we encourage an early range of motion, but resistance exercises should be avoided for at least 6–8 weeks. Follow-up appointments are recommended at 2, 4, 8, 12, and 16 weeks and 6 months postoperatively to verify improvement and progression toward full recovery. A timetable for a complete return to sport without restrictions is based on the patient’s progression during physical therapy and overall pain in the months following surgery. However, we recommend no participation in contact sports for the initial six post-operative months.
DISCUSSION
Ultimately, MCL injuries are common, especially in younger male patients who participate in contact sports. These injuries usually occur in response to a high amount of valgus stress, external rotation, or a combination of both.[6,7] If an MCL injury is suspected, a thorough physical examination and imaging workup are essential for an accurate and detailed evaluation of the lesion, which will guide decision-making for treatment. It has been previously reported that an isolated MCL tear may be best evaluated at 20–30° during physical examination while valgus stress force is applied. This same knee position should be used while taking valgus stress radiographs, where the medial femorotibial joint space is evaluated and compared with the non-injured knee.[2,8-11]
Conservative treatment of MCL injuries has been reported, in which early and controlled range of motion exercises are encouraged.[7,12,13] Ellsasser et al.[14] reported that conservative treatment for an MCL injury in professional athletes resulted in good outcomes, with a 98% success rate in those managed conservatively versus a 74% success rate in patients treated through surgery. However, this difference in outcomes between patients treated conservatively and those treated surgically may be due to the criteria patients had to fulfill to qualify for non-operative treatment. Indelicato et al.[12] reported positive outcomes following conservative treatment in collegiate football players and highlighted that the key to successful non-operative management of an MCL injury is thoroughly evaluating for other possible injuries, including a potential injury of the anterior cruciate ligament (ACL) or meniscus. Moreover, it has been reported that residual valgus laxity is identifiable in most players with an MCL injury following conservative treatment. However, this residual laxity did not influence their ability to return to sports successfully. Giannotti et al.[15] reported that when isolated, conservative treatment for all MCL injuries may result in good to excellent outcomes and a full return to pre-injury activities.
Although good outcomes are reported, failure of conservative treatment can exist, resulting in medial knee instability, dysfunction of the ACL, quadriceps weakness, and degenerative changes in the knee. For these cases, surgery is suggested, as well as in grade III injuries if an associated knee ligament injury is present.[16-19] Indications for surgery in an MCL injury include a substantial side-to-side difference in valgus laxity and evidence of considerable rotational instability.[20]
Several techniques have been described to address MCL injuries, including both repair and reconstruction methods.[21,22] Gupta et al.[23] described an anatomic reconstruction technique using a semitendinosus graft, keeping its tibial insertion. In their technique, the semitendinosus is anatomically placed into the tibia and femur and then secured into the tunnels using adjustable loop suspensory fixation, providing the advantage of controlling the tension of the graft. Ohliger et al.[24] also described a reconstruction technique using the autologous semitendinosus attached to the tibial site, which is fixed in the femoral tunnel using an interference screw and suture anchors at the tibial site. LaPrade and Wijdicks[25] described an anatomical technique using two separate grafts, reconstructing the sMCL and the POL.
CONCLUSION
We encourage the use of our procedure for the treatment of symptomatic and chronic MCL injuries unresponsive to conservative management. In greater detail, our surgery is suitable in the case of valgus laxity seen in stress radiographs and physical examination compared to the contralateral side. In our clinical experience, this simple and cost-effective technique successfully treats chronic valgus laxity and instability associated with external rotation following an MCL injury. We acknowledge the importance of performing this surgical technique only in symptomatic cases, given that most cases of residual instability following an MCL injury do not affect the patient’s quality of life and may be managed conservatively. Although we recommend our technique, future studies are needed to evaluate the efficacy of this technique through patient-reported outcome measures.
Authors’ contributions:
JLEG: Study conception and design, manuscript writing, and study supervision. CV, JVC, and MBF: Study conception, design, and manuscript writing. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
Ethical approval:
The Institutional Review Board approval is not required.
Declaration of patient’s consent:
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given consent for images and other clinical information to be reported in the journal. The patient understands that the patient’s name and initials will not be published, and due efforts will be made to conceal the patient’s identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI. Conflicts of interest: There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Medial collateral ligament injury of the knee: A review on current concept and management. Arch Bone Jt Surg. 2021;9:255-62.
- [Google Scholar]
- Simultaneous bilateral knee valgus stress radiographic technique. Arthrosc Tech. 2017;6:e2119-22.
- [CrossRef] [PubMed] [Google Scholar]
- From anatomy to complex reconstruction: A modern review on the medial collateral ligament of the knee. Arch Bone Jt Surg. 2022;10:818-26.
- [Google Scholar]
- The role of the deep medial collateral ligament in controlling rotational stability of the knee. Knee Surg Sports Traumatol Arthrosc. 2015;23:3101-7.
- [CrossRef] [PubMed] [Google Scholar]
- Structural properties of the medial collateral ligament complex of the human knee. J Biomech. 2005;38:1067-74.
- [CrossRef] [PubMed] [Google Scholar]
- Three main mechanisms characterize medial collateral ligament injuries in professional male soccer-blow to the knee, contact to the leg or foot, and sliding: Video analysis of 37 consecutive injuries. J Orthop Sports Phys Ther. 2021;51:611-8.
- [CrossRef] [PubMed] [Google Scholar]
- Shedding light on the non-operative treatment of the forgotten side of the knee: Rehabilitation of medial collateral ligament injuries-a systematic review. BMJ Open Sport Exerc Med. 2024;10:e001750.
- [CrossRef] [PubMed] [Google Scholar]
- Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am. 2010;92:1266-80.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of acute knee ligament injuries: The value of stress radiography compared with clinical examination, stability under anaesthesia and arthroscopic or operative findings. Ann Chir Gynaecol. 1986;75:37-43.
- [Google Scholar]
- Radiologic technique for measuring instability in the knee joint. Acta Radiol Diagn (Stockh). 1977;18:113-25.
- [CrossRef] [PubMed] [Google Scholar]
- Stress radiographical measurement of the anteroposterior, medial and lateral stability of the knee joint. Acta Orthop Scand. 1976;47:335-4.
- [CrossRef] [PubMed] [Google Scholar]
- Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop Relat Res. 1990;256:174-7.
- [CrossRef] [Google Scholar]
- Treatment of isolated medial collateral ligament injuries in athletes with early functional rehabilitation. A five-year follow-up study. Am J Sports Med. 1994;22:470-7.
- [CrossRef] [PubMed] [Google Scholar]
- The non-operative treatment of collateral ligament injuries of the knee in professional football players. An analysis of seventy-four injuries treated non-operatively and twenty-four injuries treated surgically. J Bone Joint Surg Am. 1974;56:1185-90.
- [CrossRef] [PubMed] [Google Scholar]
- The non-surgical management of isolated medial collateral ligament injuries of the knee. Sports Med Arthrosc Rev. 2006;14:74-7.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of acute grade III medial collateral ligament injury combined with anterior cruciate ligament injury: Anatomic ligament repair versus triangular ligament reconstruction. Arthroscopy. 2015;31:1108-16.
- [CrossRef] [PubMed] [Google Scholar]
- The management of injuries to the medial side of the knee. J Orthop Sports Phys Ther. 2012;42:221-33.
- [CrossRef] [PubMed] [Google Scholar]
- Superficial medial collateral ligament of the knee: Anatomic augmentation with semitendinosus and gracilis tendon autografts. Arthrosc Tech. 2016;5:e347-52.
- [CrossRef] [PubMed] [Google Scholar]
- Multiligament reconstruction of the knee in the setting of knee dislocation with a medial-sided injury. Arthrosc Tech. 2017;6:e341-50.
- [CrossRef] [PubMed] [Google Scholar]
- Nonoperative management, repair, or reconstruction of the medial collateral ligament in combined anterior cruciate and medial collateral ligament injuries-which is best? A systematic review and meta-analysis. Am J Sports Med. 2024;52:522-34.
- [CrossRef] [PubMed] [Google Scholar]
- Medial collateral ligament reconstruction and repair show similar improvement in outcome scores, but repair shows higher rates of knee stiffness and failure: A systematic review. Arthroscopy. 2023;39:2231-40.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction of superficial medial collateral ligament: Modified Danish technique with dual adjustable loop suspensory fixation. Arthrosc Tech. 2023;12:e2141-51.
- [CrossRef] [PubMed] [Google Scholar]
- Modified bosworth technique for medial collateral ligament reconstruction of the knee using semitendinosus tendon autograft. Arthrosc Tech. 2022;11:e1903-9.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical technique: Development of an anatomic medial knee reconstruction. Clin Orthop Relat Res. 2012;470:806-14.
- [CrossRef] [PubMed] [Google Scholar]






