Translate this page into:
Reference radiologic measurements for the assessment of tibial pilon fractures
*Corresponding author: Daniele Gianoli, Clinic of Orthopedics and Traumatology, Canton’s Hospital St. Gallen, Switzerland. danielegianoli@gmx.ch
-
Received: ,
Accepted: ,
How to cite this article: Gianoli D, Joeris A, Sommer C. Reference radiologic measurements for the assessment of tibial pilon fractures. J Musculoskelet Surg Res 2022;6:19-24.
Abstract
Objectives:
The management of pilon fractures is a challenge and the outcome depends on multiple factors, one of which is the quality of reduction. In the literature, there is no assessment of anatomical reduction in pilon fractures. We also lack standard radiological parameters in large patient groups to measure the reduction. The main aim of this analysis was to define normal standard radiological values and identify potential specific types of ankle joint morphology (morphotypes) that might deserve special attention intraoperatively.
Methods:
We analyzed data of 103 healthy contralateral ankles collected within an observational and prospective multicenter study about tibial pilon fractures. We divided the patients according to their height into two groups, measured 11 radiological parameters, and compared them with each other and the literature. In addition, using cluster analysis, we could identify three morphotypes.
Results:
There is a statistically significant difference between the two groups in the lengths of three parameters: Mortise width, medial clear space, and length of the lateral malleolus, but not in the angles. The three morphotypes differ only in body mass index and the length of the lateral malleolus.
Conclusion:
Reference values from the literature are insufficient to assess a reduction after open reduction and internal fixation of tibial pilon fractures because they depend on the height. This does not apply to angles because they are independent of height. For clinical practice, a radiological control of the contralateral healthy ankle gives the best information about the reduction quality and should always be done, especially in normal weight males.
Keywords
Ankle fracture
Pilon
Reduction
Tibial fracture
X-ray
INTRODUCTION
Tibial pilon fractures (Types B3 and C according to the AO/OTA fracture and dislocation classification) are predominantly the result of high-energy trauma and are often associated with comminuted joint surface, displacement, and often associated with extensive soft-tissue damage or open fractures.[1-3] Pilon fractures are very rare, with an incidence of 1%,[4,5] a bimodal age distribution with a peak frequency at 25–50 years, and seen predominantly in males (57–65%).[6] Pilon fractures include the articular surface and require metaphysis reconstruction and treatment of the soft tissues.[6] Due to these factors, the management of tibial pilon fractures remains a complex and challenging issue.[5]
Multiple treatment strategies of tibial pilon fractures have been described, but no method has been superior compared to the others.[7] However, two-stage treatment, first closed reduction and external fixation followed by open reduction and internal fixation (ORIF), is generally recommended.[8] External fixation without ORIF compared to ORIF shows the same rate of additional procedures or intravenous antibiotics, but more bone healing complications.[9] Studies showed that the outcome after tibial pilon fractures depends on the severity of the trauma, comorbidities, soft-tissue condition, and the reduction quality.[7,10] The anatomic reduction of the joint is considered the most important factor after articular fractures.[11-13]
Even though studies describing the anatomy of the distal tibia have been published,[10,14,15] there are no standard radiological parameters to assess the quality of reduction after tibial pilon fractures. Furthermore, although there are some publications on standardizing how radiological measures are done, radiological measurements still show low interobserver agreement and reproducibility.[16-18]
Sommer et al. analyzed different radiological parameters and found that only the length of the lateral malleolus was a predictor of clinical outcome.[16] Using radiological images of the healthy opposite side from that study,[16] the main aim of this in-depth analysis was to define standard radiological values and identify potential specific types of ankle joint morphology (morphotypes) that might deserve special attention intraoperatively.
MATERIALS AND METHODS
Study design
This is a secondary in-depth analysis of images from the healthy contralateral ankle collected within an observational and prospective multicenter study about tibial pilon fractures.[16] The Ethical Committee approved the original study of the lead center, and every patient provided informed consent before inclusion. The study was registered on ClinicalTrials.gov with the identifier NCT01316289.
Patients
In total, 117 patients in Switzerland, the USA, Austria, and Brazil were enrolled from 2012 to 2014. The patients were 18 years or older with unilateral and intra-articular distal tibia pilon fractures (AO/OTA type 43-B or 43-C). We defined some exclusion criteria: Pathological fractures, contralateral fractures, polytrauma with injury severity score more than 28, severe vascular diseases existing before the trauma, inability to walk without aids before the injury, drug or alcohol abuse, the American Society of Anesthesiologists (ASA) classifications V or VI, pregnant women (urine pregnancy test), and neurological or psychiatric disorders. Of the 117 originally enrolled patients, 14 had no radiographs of the healthy contralateral ankle and were excluded from this study. Of the 103 remaining patients, a lateral radiograph was missing in one patient, resulting in 102 images available to assess all below-described parameters.
Outcome measures
Radiographic measurements
One rater (DG) performed the radiologic evaluation since the reliability of the planned radiographic measurements (including intraclass correlation coefficient for interobserver reliability) has already been published.[16] The measured parameters included both alignment factors (lateral distal tibial angle [LDTA] and anterior distal tibial angle [ADTA]) and articular factors (talar tilt [TT], mortise width [MW], lateral clear space [LCS], medial clear space [MCS], talocrural angle [TCA], length of lateral malleolus [LLM], and length of medial malleolus [LMM]).[19-24]
These variables were measured as described by Sommer et al.,[16] except that the medial and lateral talar shift was combined into a coronal talar shift (corTS). Furthermore, the anterior and posterior talar shift was combined into a sagittal talar shift (sagTS). Thus, the shift in one plane (coronal or sagittal) was assessed instead of the shift in one direction (medial or lateral and anterior or posterior).
To evaluate the impact of body height on the measured parameters, the study population was divided into two groups based on height (Group A ≤175 cm and Group B >175 cm).
Statistical analysis
The statistical analyses were performed with R (R: A language and environment for statistical computing. Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org/). Means, standard deviations, ranges, coefficient of variation, and proportions are included for the descriptive statistics. Comparative statistics included t-tests. The level of significance was set at P < 0.05. Cluster analysis was performed applying the Ward method. The variables used for clustering were as follows: Gender, height, body mass index (BMI), MCS, LCS, TCA, LMM, and LLM. The number of clusters was defined using a dendrogram.
RESULTS
The study group consisted of 103 patients, the majority of whom (70.87%) were male. The mean age was 45.5 and the mean BMI was 28.5 kg/m2. Group A was composed of 53 patients (26 were male and 27 females) with a median height of 169 cm. Group B was composed of 50 patients (47 were male and three females) with a median height of 183 cm [Table 1]. The mean scores of the 11 parameters, in total and divided by group height, are shown in [Table 2].
| Total/Group A+B | Group A (≤175 cm) |
Group B (>175 cm) |
|
|---|---|---|---|
| Total, n | 103 | 53 | 50 |
| Gender, n (%) | |||
| Female | 30 (29.1) | 27 (50.9) | 3 (6) |
| Male | 73 (70.9) | 26 (49.1) | 47 (94) |
| Age (years) | |||
| Mean (SD) | 45.5 (13.4) | 48.2 (13.6) | 42.6 (12.8) |
| BMI (kg/m2) | |||
| Mean (SD) | 28.5 (7.3) | 28.9 (8) | 28.1 (6.6) |
| Height (cm) | |||
| Median | 175 | 169 | 183 |
BMI: Body mass index
There were statistically significant differences between Groups A and B in MW, MCS, and LLM (P = 0.023, 0.002, and 0.022, respectively). However, there was no significant difference in the angles between the two groups (LDTA, ADTA, TT, and TCA). The coefficient of variance (CV) for the three angles ADTA, LDTA, and TCA was smaller than 0.035 and for the five lengths, MW, MCS, LCS, LLM, and LMM between 0.13 and 0.30. Both the two shifts (corTS and sagTS) and TT show CV >0.827 [Table 2].
| Normal valuesa | Total | Group A (≤175 cm) | Group (>175 cm) | CV | P-value* | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Range | n | Mean (SD) | Range | n | Mean (SD) | Range | ||||
| LDTA (°, n=103) |
88.6±3.8 | 89.79±2.76 | 78.0; 96.0 | 53 | 90.00±3.04 | 78.0; 96.0 | 50 | 89.56±2.43 | 83.0; 95.0 | 0.031 | 0.418 |
| ADTA (°, n=102) |
79.8±1.6 | 84.71±3.00 | 77.0; 96.0 | 52 | 84.85±2.89 | 79.0; 91.0 | 50 | 84.56±3.12 | 77.0; 96.0 | 0.035 | 0.633 |
| TT (°, n=103) |
0 | −0.17±0.98 | −5.0; 4.0 | 53 | −0.21±0.82 | −3.0; 1.0 | 50 | −0.14±1.14 | −5.0; 4.0 | −5.633 | 0.732 |
| MW (mm, n=103) |
4±2 | 5.41±1.37 | 2.0; 9.0 | 53 | 5.11±1.44 | 2.0; 9.0 | 50 | 5.72±1.23 | 3.0; 8.0 | 0.253 | 0.023 |
| MCS (mm, n=103) |
<4 | 3.12±0.65 | 2.0; 5.0 | 53 | 2.92±0.58 | 2.0; 4.0 | 50 | 3.32±0.65 | 2.0; 5.0 | 0.207 | 0.002 |
| LCS (mm, n=103) |
<5 resp. <6 | 4.64±1.41 | 0.0; 9.0 | 53 | 4.42±1.32 | 2.0; 9.0 | 50 | 4.88±1.47 | 0.0; 9.0 | 0.303 | 0.095 |
| TCA (°, n=103) |
83±4 | 77.62±2.64 | 70.0; 84.0 | 53 | 77.26±2.33 | 74.0; 83.0 | 50 | 78.00±2.91 | 70.0; 84.0 | 0.034 | 0.161 |
| LMM (mm, n=103) |
16.79±2.27 | 11.0; 23.0 | 53 | 16.38±2.42 | 11.0; 22.0 | 50 | 17.22±2.04 | 12.0; 23.0 | 0.135 | 0.059 | |
| LLM (mm, n=103) |
28.64±3.61 | 20.0; 39.0 | 53 | 27.85±3.40 | 20.0; 39.0 | 50 | 29.48±3.67 | 21.0; 39.0 | 0.126 | 0.022 | |
| corTS (mm, n=103) |
0.27±1.72 | −6.0; 5.0 | 53 | 0.51±1.76 | −2.0; 5.0 | 50 | 0.02±1.66 | −6.0; 3.0 | 6.334 | 0.15 | |
| sagTS (mm, n=102) |
2.17±1.79 | −1.0; 7.0 | 52 | 2.46±1.72 | 0.0; 6.0 | 50 | 1.86±1.83 | −1.0; 7.0 | 0.827 | 0.091 | |
LDTA: Lateral distal tibial angle, ADTA: Anterior distal tibial angle, TT: Talar tilt, MW: Mortise width, MCS: Medial clear space, LCS: Lateral clear space, TCA: Talocrural angle, LMM: Length of medial malleolus, LLM: Length of lateral malleolus, corTS: Coronal talar shift, sagTS: Sagittal talar shift, CV: Coefficient of variation, afor the normal values, see references in the “Discussion” section, *t-test
Using cluster analysis, we could identify three morphotypes (M1, M2, and M3) that differ in LLM [Figure 1a] and BMI [Figure 1b]. Morphotype 1 included only females. Morphotypes 2 and 3 included only males. Males in morphotype 2 were obese (mean BMI 31.4). Morphotypes 1 and 3 have a normal BMI (mean BMI was 26.9 and 27.7, respectively). There was no difference in height between morphotypes 2 and 3 [Figure 1c].
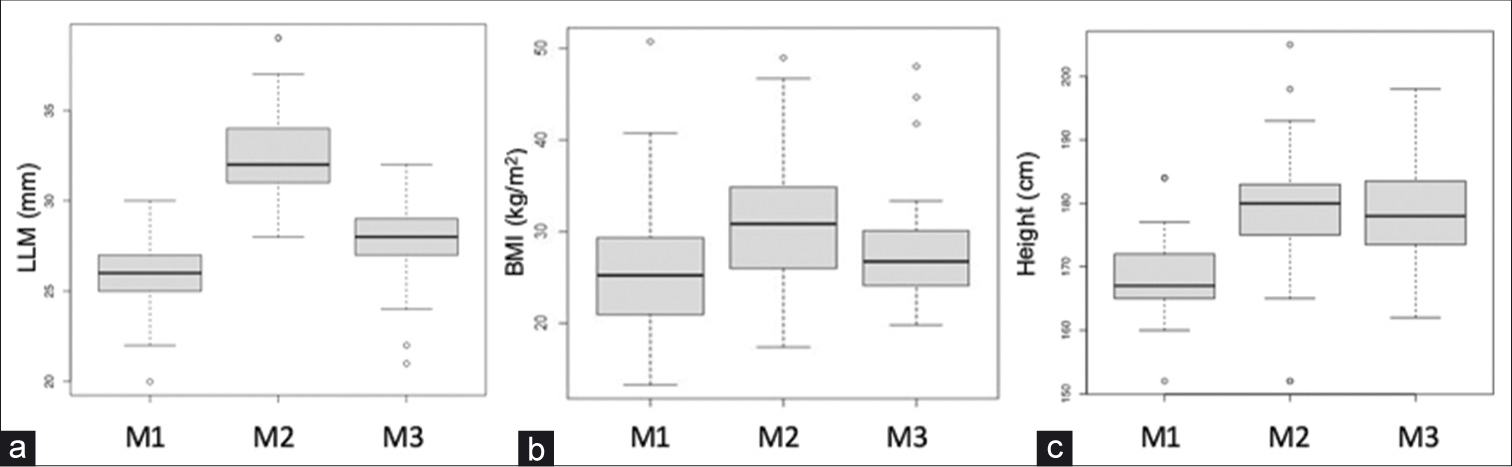
- Distribution of length of lateral malleolus (a), body mass index (b), and height (c) between the three morphotypes identified using cluster analysis.
DISCUSSION
Tibial pilon fractures are complex injuries that need challenging operative care. A possible intra- and post-operative support is the radiological parameters, which can confirm the correct reduction.
In the present study, LDTA (89.79 ± 2.76) was comparable to the values in the literature (88.6 ± 3.8).[19] However, TCA and ADTA were 77.62 ± 2.64 and 84.71 ± 3.00, respectively, and thus nearly a standard deviation smaller than what is described in the literature by Carr (83 ± 4) and Paley et al. (79.8±1.6).[19,24] This difference could be explained through the different composition of the population and/or a different method of defining the tibial shaft axis [Line C of Figure 2]; the study by Carr and Paley et al. did not specify the composition of the population.
![Radiographic measurements. (a) Coronal talar shift. (b) Sagittal talar shift. corTS: Lines A, B, C, and D are drawn as described in Sommer et al.[16] Line D’ is parallel and 5 mm distal to Line D. Point y is defined as the intersection between line C and line D’, and point x is the center of line D’ (projected on talus). The distance in mm between x and y is designated as talar shift; a positive coronal talar shift is when x is medial to y and a negative coronal talar shift is when x is lateral to y. (a) sagTS: Lines A, B, C, and D are drawn as described in Sommer et al.[16] Point z is the center of the talus, defined as the center of the circle that best fit the shape of the talar dome. The distance between point z and line C measures the sagittal talar shift: When z is anterior to line C, it is designated as positive sagittal talar shift; when z is posterior to C, negative sagittal talar shift (b).](/content/136/2022/6/1/img/JMSR-6-019-g002.png)
- Radiographic measurements. (a) Coronal talar shift. (b) Sagittal talar shift. corTS: Lines A, B, C, and D are drawn as described in Sommer et al.[16] Line D’ is parallel and 5 mm distal to Line D. Point y is defined as the intersection between line C and line D’, and point x is the center of line D’ (projected on talus). The distance in mm between x and y is designated as talar shift; a positive coronal talar shift is when x is medial to y and a negative coronal talar shift is when x is lateral to y. (a) sagTS: Lines A, B, C, and D are drawn as described in Sommer et al.[16] Point z is the center of the talus, defined as the center of the circle that best fit the shape of the talar dome. The distance between point z and line C measures the sagittal talar shift: When z is anterior to line C, it is designated as positive sagittal talar shift; when z is posterior to C, negative sagittal talar shift (b).
We found the TT values comparable with the literature (0.17 ± 0.98),[20,21] and this was the only angle measurement with a high CV, making it inappropriate for use as a reference value. The high CV might be explained by a few outliers, which presumably resulted from measurement errors due to radiographs with incorrect projection. It has been described that surgically treated pilon fractures with normal TT and MW show a good clinical result in 97.2%. In contrast, patients with abnormal TT and/or MW have a significantly worse clinical result and were significantly associated with the development of osteoarthritis.[5,19] Initial cartilage damage is also associated with osteoarthritis development. Even patients with good reduction but initial cartilage damage develop osteoarthritis and have a worse functional outcome.[25]
Talar shifts in the coronal and sagittal planes have not yet been described in the literature. The lower limb’s mechanical axis corresponds to the tibial axis and passes through the center of the talus. A coronal talar shift results in malalignment.[26] Furthermore, due to the high CV, it is necessary to compare with the contralateral ankle. Only one patient displayed a posterior talar shift. Therefore, we conclude that there should always be a slight anterior talar shift. Future research on the coronal and sagittal talar shifts in patients with tibial pilon fractures should be done to evaluate their clinical significance.
Reference values for lengths have been described in the literature for MCS, LCS, and MW. They are all comparable with the lengths measured in the present study, MCS is <4 mm (3.12 ± 0.65), LCS is <5 mm (4.64 ± 1.41), respectively, 6 mm, and MW is <4 ± 2 mm (5.41 ± 1.37).[20,22,24] In the literature, no reference values can be found for the lengths of the medial and lateral malleolus, although the length of the lateral malleolus has been found to be clinically relevant. Pilon fractures were accompanied in 85% by a fibula fracture.[11] Already Ruedi et al. showed that reconstruction of the correct length of the fibula is important for better functional results.[27] Sommer et al. also showed in their study that only prolongation of the LLM leads to a significant worsening of the “activity of daily living” – score (ADL).[16] Fractures with fibular shortening or malrotation had poor results and were significantly associated with osteoarthrosis development.[10,13,19] Apparently, the displacement of the medial malleolus, with an intact lateral malleolus, does not have the same biomechanical significance.[8] In our study, we found that for the overall population, a relation between the height and the length of the lateral malleolus and none for the medial malleolus. However, the difference of mean LLM between tall (>175 cm) and shorter (<175) individuals, despite statistical difference, is too small for practical purposes (only 1.6 mm).
We have found that there is a morphotype of males that have significantly longer LLM. This morphotype also has an increased BMI. There are no studies investigating different morphotypes of the ankle. Standard values can be determined for the three morphotypes, although this is not significantly different in females (mean LLM 26 mm) and males with normal weight (mean LLM 27.8). Only males with overweight have longer LLM (mean LLM 32.6). These references should also be considered intraoperatively since overweight males tolerate an apparent overlength of the LLM better than males of normal weight since LLM is constitutionally longer. In contrast, males of normal weight have an increased risk of a negative outcome, for example, in ADL. For this reason, looking at radiographs of the opposite side is particularly advised for males of normal weight.
Our study has some limitations. The study population consisted of patients with tibial pilon fractures, of which 73% were male and 72.4% had a high-energy trauma.[16] Therefore, there might be a certain bias in the patient population. Furthermore, our study is of cross-sectional design and the measured 11 parameters are, therefore, static. It would be interesting to see if they change over time and if this change correlates with the variation of BMI or age.
CONCLUSION
Reference values from the literature are insufficient to assess a reduction after ORIF of a tibial pilon fractures because they are dependent on the height. This does not apply to angles because they are independent of height. For clinical practice, a radiological comparison to the contralateral healthy ankle gives the best information about a successful reduction and should be done in any case, especially in normal weight males.
ACKNOWLEDGMENT
The authors thank Hans-Christoph Pape for participating in the study, Vilijam Zdravkovic for statistical analysis, and Anahí Hurtado for support in medical writing.
AUTHORS’ CONTRIBUTIONS
DG and AJ designed the study, analyzed, and interpreted data. CS collected and organized data. DG wrote the initial and final draft of the article. All authors have critically reviewed the final manuscript and are responsible for the content and similarity index.
Declaration of patient consent
The authors certify that they have obtained all appropriate patients consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
References
- Tibial plafond fractures: Changing principles of treatment. J Am Acad Orthop Surg. 1994;2:297-305.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and functional outcomes of internal fixations of displaced pilon fractures. Clin Orthop Relat Res. 1998;347:131-7.
- [CrossRef] [Google Scholar]
- A surgical approach to posterior pilon fractures. J Orthop Trauma. 2010;24:188-93.
- [CrossRef] [PubMed] [Google Scholar]
- Tibial pilon fractures: Which method of treatment? Injury. 2010;41:1183-90.
- [CrossRef] [PubMed] [Google Scholar]
- Tibial pilon fractures: A review of incidence, diagnosis, treatment,and complications. Acta Orthop Belg. 2011;77:432-40.
- [Google Scholar]
- Clinical outcome and changes in gait pattern after pilon fractures. Int Orthop. 2013;37:51-8.
- [CrossRef] [PubMed] [Google Scholar]
- Two-stage procedure protocol for minimally invasive plate osteosynthesis technique in the treatment of the complex pilon fracture. Int Orthop. 2012;36:833-7.
- [CrossRef] [PubMed] [Google Scholar]
- External fixation versus open reduction and internal fixation of pilon fractures: A systematic review and meta-analysis. J Musculoskelet Surg Res. 2018;2:41-50.
- [CrossRef] [Google Scholar]
- Open reduction and internal fixation of tibial plafond fractures: Variables contributing to poor results and complications. Clin Orthop Relat Res. 1993;292:108-17.
- [CrossRef] [Google Scholar]
- Long-term results of tibial plafond fractures treated with open reduction and internal fixation. Arch Orthop Trauma Surg. 1991;110:277-83.
- [CrossRef] [PubMed] [Google Scholar]
- Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647-59.
- [CrossRef] [Google Scholar]
- Assessment of the AO/ASIF fracture classification for the distal tibia. J Orthop Trauma. 1997;11:477-83.
- [CrossRef] [PubMed] [Google Scholar]
- Normal tibiofibular relationships at the syndesmosis on axial CT imaging. J Orthop Trauma. 2012;26:433-8.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of fracture reduction assessed by radiological parameters and its influence on functional results in patients with pilon fractures a prospective multicentre study. Injury. 2017;48:2853-63.
- [CrossRef] [PubMed] [Google Scholar]
- Interobserver and intraobserver variations in tibial pilon fracture classification systems. Foot. 2010;20:61-3.
- [CrossRef] [PubMed] [Google Scholar]
- X-ray film measurements for healed distal radius fractures. J Hand Surg Am. 1996;21:31-9.
- [CrossRef] [Google Scholar]
- Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994;25:425-65.
- [CrossRef] [Google Scholar]
- Fractures of the ankle clinical and biomechanical considerations. J Bone Joint Surg Am. 1977;59:510.
- [Google Scholar]
- Fractures of the ankle In: The Rationale of Operative Fracture Care. Berlin, Heidelberg: Springer Verlag; 1987.
- [CrossRef] [Google Scholar]
- A radiographic evaluation of the tibiofibular syndesmosis. Foot Ankle. 1989;10:156-60.
- [CrossRef] [PubMed] [Google Scholar]
- Medial Malleolar and Soft Tissue Injuries of the Ankle Philadelphia, PA: Saunders; 2003.
- [Google Scholar]
- The influence of initial cartilage damages in pilon fractures on the development of osteoarthritis and functional outcomes: A prospective multicentre case series. J Musculoskelet Surg Res. 2019;3:334-41.
- [CrossRef] [Google Scholar]
- Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745-9.
- [CrossRef] [PubMed] [Google Scholar]
- The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res. 1979;138:105-10.
- [Google Scholar]






