Translate this page into:
Return to full military activities post anterior cruciate ligament reconstruction
2 Department of Orthopaedic, Oman Medical Specialty Board, Muscat, Oman
3 Department of Orthopaedics, Armed Forces Hospital, Muscat, Oman
Corresponding Author:
Hilal S Al Housni
Department of Surgery, Division of Orthopedics, Suhar Hospital, Suhar
Oman
hilalhosni@gmail.com
| How to cite this article: Al Housni HS, Al Ghaithi AK, Al Shukaili AH, Al Abri FM, Al Kalbani SS. Return to full military activities post anterior cruciate ligament reconstruction. J Musculoskelet Surg Res 2019;3:346-349 |
Abstract
Objectives: Armed forces represent a physically active population who engage in regular exercises, recreational sports, and physical training that place them at high risk of injury to an anterior cruciate ligament (ACL). Considering the high occupational demand, uniformed military personnel (UMP) are encouraged to have a surgical reconstruction of a ruptured ACL to resume their military activities. The aim of this study was to assess the outcomes of a full return to duties in the armed forces after primary ACL reconstruction. Methods: A single-institution, retrospective review through the analysis of surgical record data and phone interviews of UMP who underwent primary ACL reconstruction during a 5-year period was conducted. Measured endpoints were the rate of return to full military duties as well as knee function (measured by the Lysholm score). Results: The total number of UMP who underwent ACL reconstruction included in the study was 137 with a minimum follow-up of 1 year. All patients were males. The mean age was 30.2 (minimum 22, maximum 44) years. Isolated ACL injury was found in 30.7%, whereas 69.3% were associated with a meniscus injury. The majority of the surgeries were done within 5 years of the injury (92%). The mean postoperative Lysholm functional score was 90.22. Seventy-five percent of the service members returned to full military activity. Conclusions: The overall majority of UMP returned to full military duties with excellent functional Lysholm score that shows the effectiveness of ACL reconstruction in this active population.Introduction
Anterior cruciate ligament (ACL) injury is one of the most common injuries in sports, especially those which involve pivoting and jumping movements.[1],[2],[3] ACL tears comprise a high percentage of the knee injuries in the uniformed military personnel (UMP) community due to the unique physical demands of the job. Although the true incidence of ACL injuries among UMP is unknown, a population study among all service members in U.S special operation forces between 1997 and 2003 calculated ACL injury rates to be ranging from 2.29–3.79 cases per 1000 person-years.[4]
Physical demand for professions such as the military makes it difficult to modify duties. UMPs are required to perform heavy duties such as distance running and aggressive impact on a daily basis to be able to continue in the profession. Therefore, UMPs accept surgical reconstruction as the most common treatment option. However, the existing literature shows that surgical treatment does not work in up to 50% of cases.[5],[6],[7],[8] Antosh et al. reported on 450 ACL reconstructions among UMPs and only 43% had a full return to military service.[9] Cullison et al. reported dismissal of 23% of 120 UMPs from service after ACL reconstruction surgery.[10] This is because the ability of this population to return back to their preinjury level of activity after ACL reconstruction is governed by different factors, which include the knee function after the operation, social reasons, and fear of reinjury. The military tough work environment is an added factor that might decrease the rate of return to the preinjury level of activity.[6] Rai et al. looked into the outcome of 300 ACL surgeries in UMP where 5% developed postoperative complications such as infection, graft failure anterior knee pain, and stiffness.[11]
Reliability and validity of the Lysholm score were well established in the literature.[12] As patient-administered scores, the Lysholm knee score demonstrated acceptable psychometric parameters. It also has acceptable responsiveness to be used in early return to function after ACL treatment. In this article, we report the outcomes of a full return to duties in the UMP after primary ACL reconstruction. We also analyzed the risk factors, which could lead to long-term disability.
Materials and Methods
Study design and data collection
This cross-sectional retrospective study was conducted in the main referral Armed Forces Hospital in Oman/Muscat. Data were retrieved from the electronic health system for 5 years (2011–2015). The target population was identified by the medical record number. With minimum of one-year follow-up, all active UMP who underwent ACL reconstruction surgery were matriculated in the study. Nonactive personals with multi-ligament injury or revision surgeries were excluded.
Documented data included age, rank, injury type, time until surgical intervention, and radiological and surgical arthroscopic information. The radiological and arthroscopic information confirmed whether the ACL injury was isolated or associated with meniscus injury as well as confirming osteoarthritis (OA) changes if any. The second stage was conducting phone interviews by an orthopedic resident to obtain information about their current work status and to perform Lysholm functional knee scores. The response rate to phone interviews was 100%.
The ACL reconstructions were performed or supervised by the same orthopedic surgeon at a tertiary military hospital. All surgeries were done arthroscopically following the same technique. Quadruple hamstring autograft was used, fixed with tight rope in the femoral side and interference screw in the tibial side. All patients followed the same structured rehabilitation program postoperatively.
Endpoint measure and statistical analysis
The primary endpoint was the rate of return to military missions. Return to full duties is defined as the return to previous professional activities without physical limitations as reported by the Medical Council and the Military Battalion. Although our military forces are not engaged in war or active combat, it is planned to have regular physical training to stay in shape. These activities include Combat fitness training (CFT), Physical fitness training (PFT), heavy driving, and sports. Failure to return to duties was defined as the inability to continue military service; patients were discharged from the army or transferred to a job where they were no longer required to perform military physical training. The third group of patients returned to their duties with restrictions. These patients have returned to their jobs but are still unable to carry out heavy physical activities.
Categorical data were concise using percentages and Chi-squared tests or Fisher's exact test, whichever was most appropriate. Continuous variables such as means and standard deviations or medians and interquartile ranges were examined using the Student's t-test and analysis of variance or Mann–Whitney U-test as appropriate. Significance was recognized when P > 0.05. All data were entered into SPSS program for Windows version 22 (SPSS, Chicago, IL, USA) which was used for subsequent statistical analysis.
Results
The total number of UMP who underwent ACL reconstruction was 137, all of whom were included in the study [Table - 1]. All patients were males, with a mean age of 30.2 years (minimum 22 maximum 44). Majority of the sampled population were none officers (93.4%, 128), whereas only 6.6% (9) were officers. More than two-thirds (69.3%, 95 UMP) had an associated meniscus injury and 30.7% (42 UMP) had an isolated ACL injury. One hundred and two patients (74.5%) returned to full military activity, (they were able to perform fitness combat training [CFT], fitness training [PFT], heavy driving, and sports) and 32 patients (23.4%) returned to duties with physical restrictions as they were not able to re-join CFT, PFT, or sports. Three patients (2.2%) did not return to their duties and left military services.
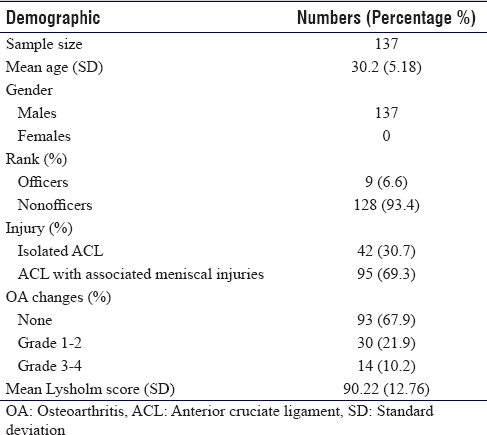
Operating surgeon reported OA changes of Grade 1–2 in 21.9% (30 UMP), and Grade 3–4 in 10.2% (14 UMP), whereas 93 UMPs showed no arthritic changes.
Subgroup analysis was done to assess if associated OA changes, meniscal injury, or delayed surgery affected the functional scores or return to duties. None of these variables showed a statistically significant difference.
Lysholm knee functional score
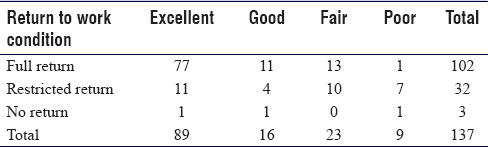
The mean Lysholm functional score was 90.22. The scores were graded as excellent (95–100), good (84–94), fair (65–83), and poor (<65) according to the Tegner activity scale. Eighty-nine (65%) patients had an excellent functional score, 16 (11.7%) patients had a good score, 23 (16.8%) patients had a fair score, and 9 (6.6%) patients had a poor score [Table - 2].
Discussion
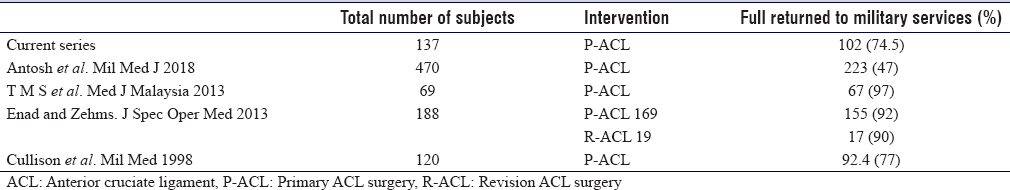
Our results show a lower rate of return to full duties compared to the literature; however; military training and the level of physical activities are expected to be variable. The ability to return to the previous level of activity after ACL reconstruction surgery is variable, as reported by the previous literature [Table - 3]. However, this outcome measure is influenced largely by the type of activity involved. A research study among U.S military aviators showed that 94.3% returned to aviation service and 2.3% were terminated.[13]
UMPs are thought to resemble high-level athletes who have similar expectations of returning to preinjury status.[14] The athlete's state of mind plays an important role in his return to sport after the successful rehabilitation of ACL reconstruction surgery. Previous literature has shown that fear of reinjury was a critical factor in not returning to the level of preinjury activity.[14] This can explain why 46.8% (11 excellent and 4 good of 32 patients) of our patients who have returned to work had good and excellent functional grades, compared to the patients who did not return to their duties.
The literature showed that ACL injury may be associated with meniscal injuries in 42%–77% of the cases and cartilage injury in 20%–23% of the cases. These associate injuries were associated with a lower return rate to play.[15] Furthermore, patients with cartilage lesions showed worse outcome in functional score compared to patients without cartilage lesions 2 years after ACL reconstruction.[16] In this series, most patients underwent delayed ACL surgery approximately 1-year delay after injury, which may have led to higher rates of associated injuries. However, we could not correlate the presence of associated injuries to lower return to military tasks.
The result of our study was to measure the ability to return to the previous level of duty. Although this is not easy task, reports have shown that athletes were able to return to their previous of activity, although they couldn't perform their best.[3] Similarly, in this series, although 75% of the patients return to preinjury activities, the remaining questions are they facing difficulty in performing the required duties? The Lysholm functional score of the knee was used to study the effectiveness of their postoperative performance where the majority showed an excellent score; however, the average score among different groups was not statically significant. This finding should future work to determine the quality of postoperative military work performance.
Although high-rank officers are expected to undergo relatively less physical activity jobs compared to nonofficers,[10] our study did not show a statistically significant difference in returning to activities between different ranks after ACL reconstruction. However, it is worth mentioning that only 9 patients (6.57%) were officers.
Limitation
The study has a few limitations that could not be overcome. Although reliability and validity of the Lysholm score were well established in the literature, the patient-administered Lysholm knee score demonstrated acceptable psychometric parameters. It also has acceptable responsiveness to be used in early return to function after the ACL treatment. In this study, the obtained functional score corresponded with the return to activity. However, the reliability and responsiveness of physician-administered Lysholm functional knee scores are lower compared to self-administered Lysholm functional knee scores. Moreover, it was difficult to obtain the exact time to return to full duties due to the lack of information from the e-health system, and it was difficult to obtain accurate numbers from patients. Another limitation is the fact that this study is a retrospective analysis; it would be more reliable to conduct a similar study prospectively.
Conclusions
The vast majority of UMP who have returned to full military assignments with an excellent functional Lysholm degree demonstrate the effectiveness of the surgical intervention in this active population. This report may instruct sports surgeons working in a military setting to advise patients with ACL deficiencies and who are considering surgical reconstruction on a possible return to work. It also may guide the employers on the expectations and prognosis of their injured personnel.
Ethical consideration
The study was approved by the Ethical Committee at the Armed Forces Hospital.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contribution
HSA conceived the study, helped in data collection, and planned and wrote this manuscript. SSA and AKA contributed to the critical revision of the manuscript. AHA and FA helped in data collection and planning the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Kaeding CC, Léger-St-Jean B, Magnussen RA. Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med 2017;36:1-8. [Google Scholar] |
| 2. | Ellman MB, Sherman SL, Forsythe B, LaPrade RF, Cole BJ, Bach BR Jr. Return to play following anterior cruciate ligament reconstruction. J Am Acad Orthop Surg 2015;23:283-96. [Google Scholar] |
| 3. | Theiss JL, Gerber JP, Cameron KL, Beutler AI, Marshall SW, Distefano LJ, et al. Jump-landing differences between varsity, club, and intramural athletes: The jump-ACL study. J Strength Cond Res 2014;28:1164-71. [Google Scholar] |
| 4. | Owens BD, Mountcastle SB, Dunn WR, DeBerardino TM, Taylor DC. Incidence of anterior cruciate ligament injury among active duty U.S. military servicemen and servicewomen. Mil Med 2007;172:90-1. [Google Scholar] |
| 5. | Enad JG, Zehms CT. Return to full duty after anterior cruciate ligament reconstruction: Is the second time more difficult? J Spec Oper Med 2013;13:2-6. [Google Scholar] |
| 6. | Tengku M, Shahrulazua A, Masdiamin M, Musa K, Muhamad F, Mohammad A. The activity leading to ACL injury and the ability to resume duty following reconstructive surgery in Malaysian military patients. Med J Malaysia 2013;68:115-8. [Google Scholar] |
| 7. | Ryu JH, Provencher MT. Special considerations for ACL graft selection in the young, active military patient. J Knee Surg 2011;24:73-82. [Google Scholar] |
| 8. | Tennent DJ, Posner MA. The military ACL. J Knee Surg 2019;32:118-22. [Google Scholar] |
| 9. | Antosh IJ, Patzkowski JC, Racusin AW, Aden JK, Waterman SM. Return to military duty after anterior cruciate ligament reconstruction. Mil Med 2018;183:e83-9. [Google Scholar] |
| 10. | Cullison TR, O'Brien TJ, Getka K, Jonson S. Anterior cruciate ligament reconstruction in the military patient. Mil Med 1998;163:17-9. [Google Scholar] |
| 11. | Rai SK, Varma R, Wani SS. Study of outcome of 300 cases of arthroscopic anterior cruciate ligament reconstruction with quadrupled hamstrings tendon graft using anterior cruciate ligament tightrope for femoral fixation. J Musculoskelet Surg Res 2018;2:26-30. [Google Scholar] |
| 12. | Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR, et al. The reliability, validity, and responsiveness of the lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med 2009;37:890-7. [Google Scholar] |
| 13. | Belmont PJ Jr., Shawen SB, Mason KT, Sladicka SJ. Incidence and outcomes of anterior cruciate ligament reconstruction among U.S. army aviators. Aviat Space Environ Med 1999;70:316-20. [Google Scholar] |
| 14. | Bottoni CR. Anterior cruciate ligament reconstructions in active-duty military patients. Oper Tech Sports Med 2005;13:169-75. [Google Scholar] |
| 15. | Mithoefer K, Della Villa S. Return to sports after articular cartilage repair in the football (Soccer) player. Cartilage 2012;3:57S-62. [Google Scholar] |
| 16. | Røtterud JH, Sivertsen EA, Forssblad M, Engebretsen L, Arøen A. Effect of meniscal and focal cartilage lesions on patient-reported outcome after anterior cruciate ligament reconstruction: A nationwide cohort study from Norway and Sweden of 8476 patients with 2-year follow-up. Am J Sports Med 2013;41:535-43. [Google Scholar] |
Fulltext Views
5,748
PDF downloads
1,728





