Translate this page into:
Rotational instability of the knee: Injury of anterior cruciate and anterolateral knee ligaments, MRI findings
2 Department of Orthopaedic Surgery, Hospital Español de México, Mexico City, Mexico
Corresponding Author:
Ramón Gonzalez-Pola
Hospital Español de Mexico, Av. Ejército Nacional 613, Col. Granada, Del. Miguel Hidalgo, 11520 CDMX
Mexico
rgonzalezpola@gmail.com
| How to cite this article: Gonzalez-Pola R, Gómez Mont-Landerreche JG, Herrera-Lozano A, Torres-Valdés RA, Flores-Carrillo A. Rotational instability of the knee: Injury of anterior cruciate and anterolateral knee ligaments, MRI findings. J Musculoskelet Surg Res 2021;5:24-29 |
Abstract
Objectives: The anterior cruciate ligament (ACL) is a major stabilizing structure of the knee, restraining force of anterior translation, while also preventing excessive tibial medial and lateral rotation. Persistent rotatory knee laxity is increasingly recognized as a common finding after ACL reconstruction. The impact of the anterolateral knee structures is now known to be significant. This study aimed at evaluating patients with the symptoms of knee rotational instability through the use of simple magnetic resonance imaging (MRI) looking for the presence and combined injury of the ACL and anterolateral ligament (ALL). Methods: Descriptive study of 564 MRIs of patients with lesions of the ACL and symptoms of rotational instability, which were retrospectively evaluated in 5 years. The authors assessed the images. The visibility of ALL in T1, T2, and FatSat was evaluated in coronal, axial, and sagittal sections, as well as the presence of lesions. Results: The ALL was visible in a total of 505 MRIs (89.5%) similar to those previously reported in the literature, and its lesion was accompanied in 121 patients with partial ACL injury (23.9%), in 141 with total rupture of ACL (27.8%). Conclusions: The ALL is a dense structure seen by MRI in the coronal plane, similar to that of any other ligament structure, and its lesion was found, in conjunction with an ACL lesion, in 46.4% of the patients with the clinical symptoms of rotational instability, and it can also present itself as an isolated injury.
Introduction
The anterior cruciate ligament (ACL) provides approximately 85% of the total restraining force of anterior translation. It also limits excessive tibial lateral and medial rotation, in addition to varus and valgus stresses. Together with the posterior cruciate ligament, the ACL controls the joint kinematics, guiding the center of rotation of the knee.[1]
Rotatory knee laxity (RNL) is increasingly recognized as a frequent finding after ACL reconstruction. While the reasons behind RNL are multifactorial,[2],[3],[4],[5],[6] the impact of both, the anterolateral ligament (ALL) and iliotibial band (ITB), is important.[8],[9],[10] Therefore, much interest has been aimed toward better understanding these structures (anatomy, biomechanics, and injury patterns), to understand any RNL that results from the damage to these structures.
In general, the medial compartment allows less mobility than the lateral due to the junction of the medial meniscus with the articular capsule. The lateral compartment increases its mobility in a weight-bearing setting as a result of the anatomical aspects of the lateral tibia and medial plateau, as the convexity of the lateral plateau is unable to maintain the lateral condyle, whereas the concavity of the medial plateau secures the medial condyle. By removing the restriction function of the ACL as a result of an injury, rotational instability symptoms may appear, as determined by Hughston et al.,[11],[12] and it can be clinically evaluated using the pivot shift test.[7],[13]
Aiming to detail the origin, insertion, trajectory, and other distinct characteristics of the ALL, anatomical reviews emerged. From cadaveric studies to magnetic resonance imaging (MRI) findings, the origin of the ALL was located anterior and distal to the origin of the lateral collateral ligament (LCL), continuing next to the lateral femoral condyle, alongside the fibers of the popliteal muscle and the LCL. Its direction is oblique to the tibia, with a couplet insert, attached to the lateral meniscus and the proximal tibia, bounded by the head of the fibula and Gerdy's tubercle.[14],[15],[16],[17] Parsons et al. described the features of the ALL using MRI, reporting that its dimension varied from 3.9 cm in extension to 4.2 cm in flexion, indicates that there is greater flexural stress.[19]
From a biomechanical point of view, Rasmussen et al. and Nitri et al. proved that the ITB, the ALL, and the ACL all play crucial roles in anterolateral rotatory instability. Seemingly, significant rotational instability requires a combined injury of the ACL and either the ITB or the ALL.[21],[22] The latter appears to occur frequently, with Ferretti et al. demonstrating an incidence of 90% after a systematic surgical exploration.[23]
The objective of the current study was to assess the presence and injury of the ALL through simple knee MRI studies in patients with the symptoms of rotational instability and RNL, associated with diagnosed ACL injuries. Searching for a combined injury that could be an overlooked cause for rotational instability.
Subjects and Methods
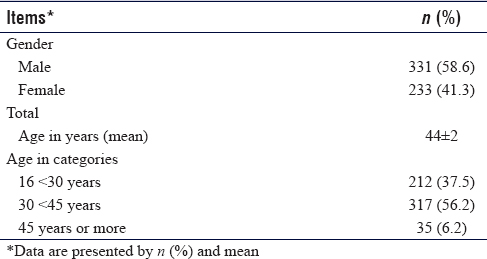
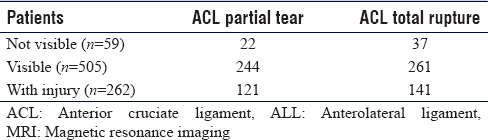
Over 5 years (2012–2017), a monocenter study was performed for evaluating rotational instability symptoms on patients. The inclusion criteria were patients between 16 and 50 years of age with a previously diagnosed ACL lesion, after conservative treatment or after a symptomatic ACL reconstruction, with proven ACL injury on MRI [Table - 1].
Patients with a history of recent lower limb or knee injury, complaints of the contralateral knee, locked knee, rheumatoid or other inflammatory diseases of the joints, and congenital lower limb malformation that could influence the rotation of the leg, were excluded. None of the evaluated patients had been previously, clinically or based on imaging studies, diagnosed with ALL injury.
Clinical examination of the knee
Two examiners independently performed physical examinations on the enrolled patients; the clinical diagnosis of rotational instability was made using the pivot-shift test[7] and the tibial internal rotation (TIR) test.[25] All examinations were performed in the same order. Physical examination of patients was repeated during a second appointment to confirm the diagnosis. Both examiners were blinded for the outcomes of the previous physical examination.
Magnetic resonance imaging of the anterolateral ligament and anterior cruciate ligament
The ALL was retrospectively identified on MRI, evaluated individually by all the authors, having experience in anatomic pathology and musculoskeletal imaging. The radiological and anatomical criteria for locating and describing the ALL, are the same used in studies previously described.[24],[26],[27],[31],[33]
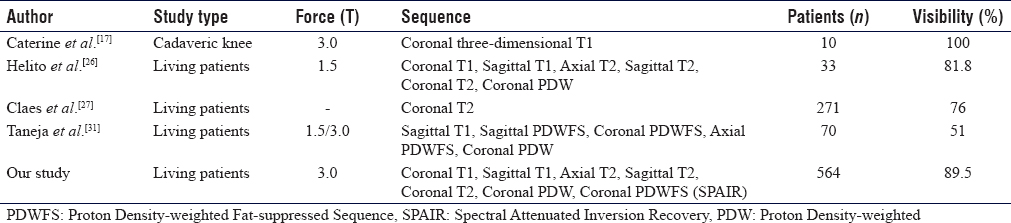
All MRI studies were performed on a 3.0-Tesla magnetic force resonator (Philips Achieva 3.0T TX). Images were obtained in T1 sequences in the coronal and sagittal view, and in T2 in axial, coronal, and sagittal views, with fat saturation, 3-mm thickness per slice. Axial and sagittal sequences by MRI were used solely to confirm the ALL's position and situation, based on previously commented anatomical reviews [Figure - 1].
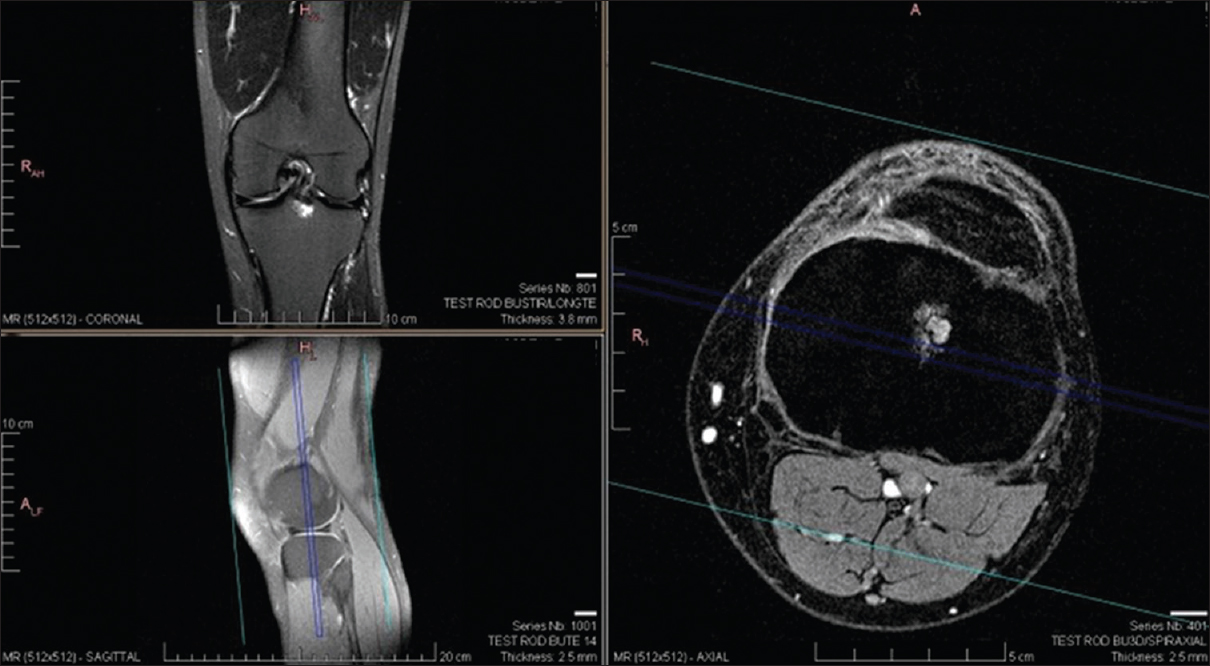 |
| Figure 1: The characterization of the ligament in the sequences acquired in the axial and sagittal planes was limited. These sequences were used to confirm the location of the anterolateral ligament, depending on the parameters of anatomical studies[8],[9],[31] |
The ALL was scored as visible or nonvisible. If the ALL was visible, it was scored visibly intact or injured. In addition, the MRI was also assessed for other injuries of the knee by a musculoskeletal radiologist as part of the routine protocol in patients with an ACL injury, which was independently scored as a partial or total tear.
Statistical analysis
Statistical analysis was performed using the IBM SPSS Statistics version 25.0. (IBM SPSS Statistics, Chicago, IL, USA). Because of difficulty in assessing both rotational instability and the visibility of the ALL, we focused on the degree of agreement between different raters. The outcomes measured were intra-rater agreement and inter-rater agreement for the pivot shift test, TIR test and visibility of the ALL on MRI. To determine coherence among raters Cohen's kappa coefficients (κC) were calculated for intra-rater agreement.[28] Moreover, for assessing inter-rater agreement, different raters are considered not unique; therefore, Fleiss' kappa coefficients (κF) were calculated.[29] For comparing the results of the pivot shift test and the TIR test, the effect size was measured using Cohen´ s d.
The kappa values are interpreted as follows: <0.00, poor agreement; 0.00–0.20, slight agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; and 0.81–1.00, almost perfect agreement. For Cohen´ s d, suggested that >0.01, very small effect; 0.2, small effect; 0.5 medium effect; and 0.8, large effect size.[30]
Results
In this study, 600 patients were included; however, after physical examination, 24 patients turned out to meet one of the exclusion criteria, and were therefore, excluded from the study. Another 12 patients did not present their MRI on the follow-up visit and were also excluded. A sample size of 230 (40%) patients was assessed for inter-rater agreement and intra-rater agreement, given a confidence interval (CI) of 5 and a confidence level of 95% [Figure - 2].
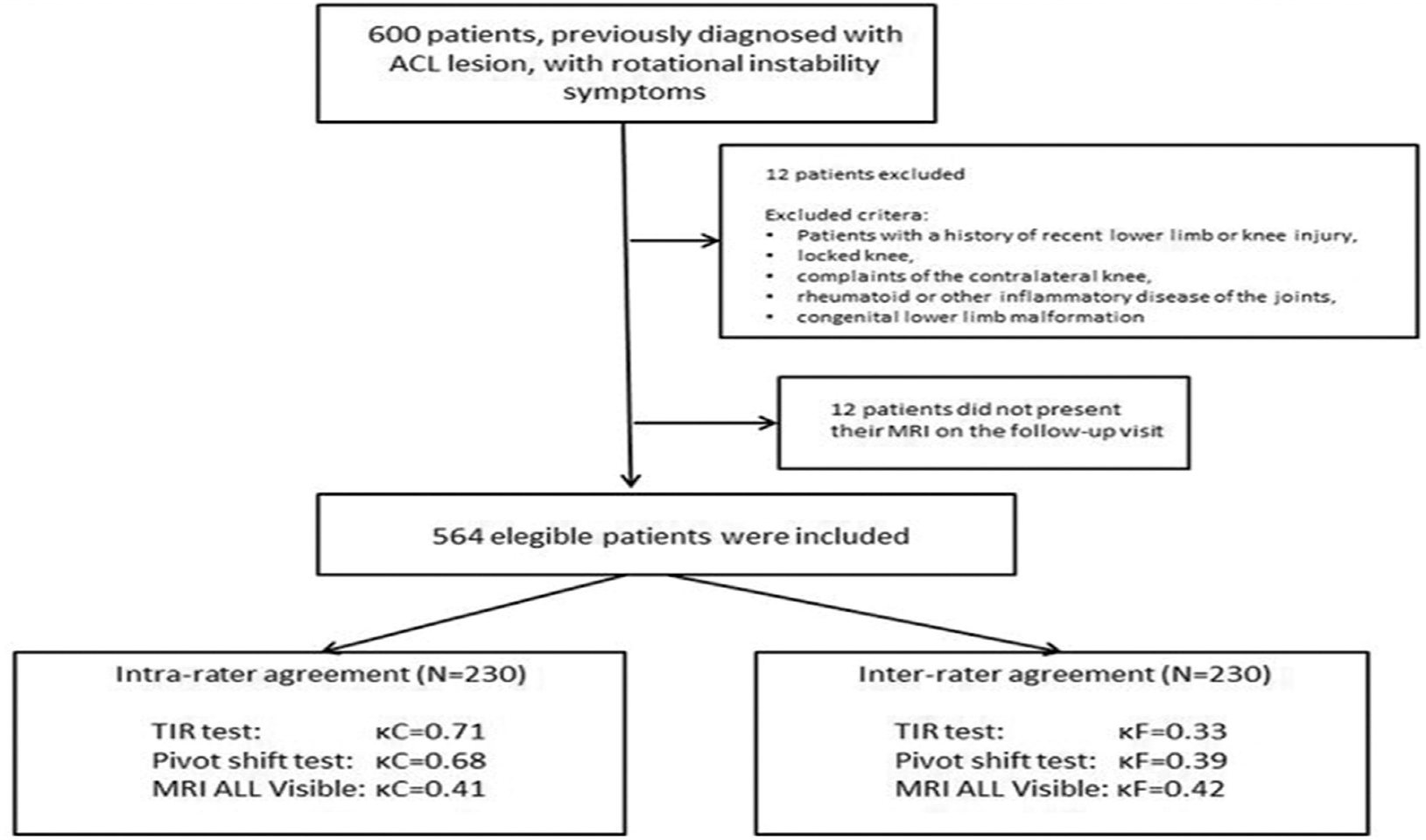 |
| Figure 2: Flowchart of patient selection for rater agreement reliability of the pivot shift test, tibial internal rotation test and anterolateral ligament visualization on magnetic resonance imaging |
Visualized as a slender structure, with a regular and occasionally undulating outline on the MR images, the ALL presented a characteristic signal similar to that of other knee ligament morphology, being hypointense on T2, seen distinctly in the coronal sections.
The femoral origin insertion was distinguished near the anterior portion of the LCL, with a vertical distal path toward the lateral meniscus body, the meniscal portion showed an oblique path toward its distal insertion, maintaining a path parallel to the ITB, inserting marginally to Gerdy's tubercle [Figure - 3].
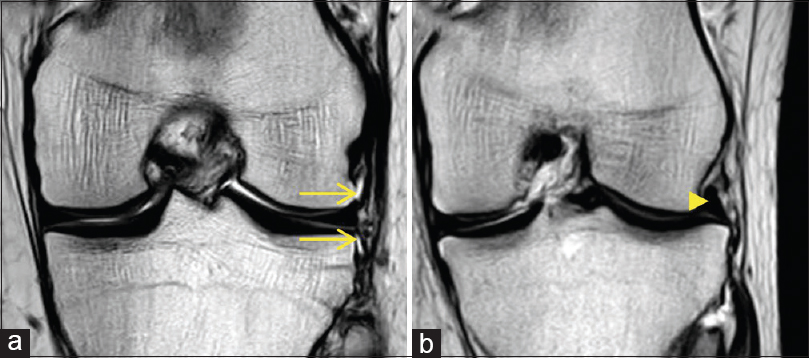 |
| Figure 3: Magnetic resonance imaging in the coronal plane that fully represents the anterolateral ligament shown as a dark dense band. (a) A complete view of the anterolateral ligament with arrows pointing at its body, above, at and below the lateral meniscus. (b) A coronal view showing fibers rupture of the anterolateral ligament at its meniscal insertion by the arrowhead |
From the total of our sample of 564 patients, we divided them into patients with partial injury and total rupture of the ACL, all participants with clinical rotational instability signs and symptoms [Table - 2].
In total, both examiners found a positive pivot shift test in 120 (52.2%) patients during the the first physical examination and 154 (69%) positive patients for a TIR test. Overall agreement between all the orthopedic surgeons for the visibility of the ALL thru MRI was 78%.
Substantial intra-rater agreement was found both for the pivot shift and TIR test, κC = 0.71 (95% CI: 0.64 ± 0.06), P = 0.02 and κC = 0.68 (95% CI: 0.63 ± 0.06), P = 0.02, respectively, with a d of very small effect size (0.02) [Table - 3].
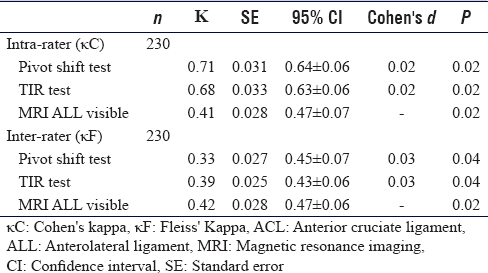
Similar results were found for intra-rater agreement, having a fair result both for the pivot shift and TIR test, κF = 0.33 (95% CI: 0.45 ± 0.07), P = 0.04 and κF = 0.39 (95% CI: 0.43 ± 0.06), P = 0.04, respectively, with a d of very small effect size (0.03).
When analyzing MRI sequences, it was observed that the ALL could be clearly seen in 505 MRIs, leaving only 59 (10.4%) where none of the examiners could identify it. A section of the ligament was seen measurably in 89.6% of all the MRIs, and the meniscal portion was the most consistent image observed. A fair intra-rater agreement κC = 0.41 (95% CI: 0.47 ± 0.07), P = 0.02 and inter-rater agreement κF = 0.42 (95% CI: 0.47 ± 0.06), P = 0.02 were found between all the orthopedic surgeons raters.
An association of a combined ACL-ALL injury was found in 262 MRIs (46.45%) of all the patients enrolled. Also, we encountered 8 patients (1.4%) that had symptoms of rotational instability, with an isolated lesion of the ALL.
Discussion
The importance of ALL as a source of anterolateral and rotational knee stability has recently gained new interest, having its anatomy and biomechanics positively identified, it is now understood that injury to this ligament increases anterolateral instability, clinically visible through the degree of the pivot, resulting in a poor functional result after ACL reconstruction.[18],[19],[20] Despite this, there are still few studies that demonstrate an adequate protocol to observe this structure through MRI.
The percentage of visibility of ALL achieved in our study, similar to that already reported in the literature[24],[25],[26],[27] reveals that it is possible to visualize it, although not all of its morphology, with the standard sequence for knee resonance, being able to characterize completely in one examination and determine possible injuries.
The inability to see the ligament can be attributed to a poor technique or limitations of MRI sequences and views. For example, the origin of ALL and LCL, as well as the insertion of the popliteal muscle tendon, are contiguous and it is not always possible to distinguish them easily, and there may also be overlapping of the joint capsule or the ITB.[32],[34] When in doubt and with a suspicious examination, look intently for the structure.
Carpenter et al.[33] showed that after an ACL reconstruction, internal rotation usually increases, being clinically noted in flexion-extension movement, compared to knees with a native ACL. Therefore, it is necessary to adequately identify injuries in other structures, such as the ALL, and the failure to obtain a perfect knee rotation control with modern ACL reconstruction procedure.
It is necessary to improve the visualization of the ligament, of specific sequences on MRI, and by knowing the relatively new ALL and its significance in the rotational stability, not to mention looking for alternative factors causing instability and/or failure of a primary ACL repair. We found that, out of a total of 564 MRI scans, in only 59 we were unable to locate the ALL and that in 262 MRIs there was an injury associated with an ACL injury, that is, 46.4% of the studies. This large percentage must infer the importance of directly looking for the pathology of the ALL. A limitation of the present study is the fact of its retrospective nature [Table - 4].
Conclusion
Being able to conclude that the ACL reconstruction may not completely restore the biomechanics of the knee and it is always necessary to search directly for associated injuries; Large-scale clinical studies will be needed to direct patient care, but the clinical and imaging evaluation of the ALL is important and should be the norm for future studies, since its injury may be responsible for a poor evolution after an ACL reconstruction or simple knee arthroscopy.
Recommendations
There should be a careful assessment of the ALL in patients with rotational instability and directly relating the residual instability in patients at risk, possibly after an ACL reconstruction, since this structure and its pathology often go unnoticed. Further studies and an adequate MRI protocol are necessary to advance our knowledge of the ALL and its contribution to knee stability.
Ethical approval
This study has been approved by the Research Ethics Board of Hospital Español on November 13th 2019. Patient consent was obtained for all participants and is compliant with the Declaration of Helsinki.
Financial support and sponsorship
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
GPR, GLJ and FCA conceived and designed the study. GPR, HLA and TVR conducted research, provided research material, and collected and organized data. GPR, GLJ and HLA analyzed and interpreted data. GPR and GLJ wrote the initial and final draft of the article, TVR and FCA provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the manuscript's content and similarity index.
| 1. | Hollis JM, Takai S, Adams DJ, Horibe S, Woo SL. The effects of knee motion and external loading on the length of the anterior cruciate ligament (ACL): A kinematic study. J Biomech Eng 1991;113:208-14. [Google Scholar] |
| 2. | Zantop T, Schumacher T, Diermann N, Schanz S, Raschke MJ, Petersen W. Anterolateral rotational knee instability: Role of posterolateral structures. Winner of the AGA-DonJoy Award 2006. Arch Orthop Trauma Surg 2007;127:743-52. [Google Scholar] |
| 3. | Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA. Posteromedial meniscocapsular lesions increase tibiofemoral ioint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med 2016;44:400-8. [Google Scholar] |
| 4. | Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H. Risk factors associated with grade 3 pivot shift after acute anterior cruciate ligament injuries. Am J Sports Med 2016;44:362-9. [Google Scholar] |
| 5. | Rahnemai-Azar AA, Abebe ES, Johnson P, Labrum J, Fu FH, Irrgang JJ, et al. Increased lateral tibial slope predicts high-grade rotatory knee laxity pre-operatively in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2017;25:1170-6. [Google Scholar] |
| 6. | Musahl V, Rahnemai-Azar AA, Costello J, Arner JW, Fu FH, Hoshino Y, et al. The influence of meniscal and anterolateral capsular injury on knee laxity in patients with anterior cruciate ligament injuries. Am J Sports Med 2016;44:3126-31. [Google Scholar] |
| 7. | Thein R, Boorman-Padgett J, Stone K, Wickiewicz TL, Imhauser CW, Pearle AD. Biomechanical assessment of the anterolateral ligament of the knee: A secondary restraint in simulated tests of the pivot shift and of anterior stability. J Bone Joint Surg Am 2016;98:937-43. [Google Scholar] |
| 8. | Tavlo M, Eljaja S, Jensen JT, Siersma VD, Krogsgaard MR. The role of the anterolateral ligament in ACL insufficient and reconstructed knees on rotatory stability: A biomechanical study on human cadavers. Scand J Med Sci Sports 2016;26:960-6. [Google Scholar] |
| 9. | Samitier G, Marcano AI, Alentorn-Geli E, Cugat R, Farmer KW, Moser MW. Failure of anterior cruciate ligament reconstruction. Arch Bone Jt Surg 2015;3:220-40. [Google Scholar] |
| 10. | Carson EW, Anisko EM, Restrepo C, Panariello RA, O'Brien SJ, Warren RF. Revision anterior cruciate ligament reconstruction: Etiology of failures and clinical results. J Knee Surg 2004;17:127-32. [Google Scholar] |
| 11. | Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities. Part I. The medial compartment and cruciate ligaments. J Bone Jt Surg 1976;3:159-72. [Google Scholar] |
| 12. | Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities. Part II. The lateral compartment. J Bone Jt Surg 1976;3:173-9. [Google Scholar] |
| 13. | Diermann N, Schumacher T, Schanz S, Raschke MJ, Petersen W, Zantop T. Rotational instability of the knee: Internal tibial rotation under a simulated pivot shift test. Arch Orthop Trauma Surg 2009;129:353-8. [Google Scholar] |
| 14. | Claes S, Luyckx T, Vereecke E, Bellemans J. The Segond fracture: A bony injury of the anterolateral ligament of the knee. Arthroscopy 2014;30:1475-82. [Google Scholar] |
| 15. | Dodds AL, Halewood C, Gupte CM, Williams A, Amis AA. The anterolateral ligament: Anatomy, length changes and association with the Segond fracture. Bone Joint J 2014;96-B: 325-31. [Google Scholar] |
| 16. | Vieira EL, Vieira EA, da Silva RT, Berlfein PA, Abdalla RJ, Cohen M. An anatomic study of the iliotibial tract. Arthroscopy 2007;23:269-74. [Google Scholar] |
| 17. | Caterine S, Litchfield R, Johnson M, Chronik B, Getgood A. A cadaveric study of the anterolateral ligament: Re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc 2015;23:3186-95. [Google Scholar] |
| 18. | Kittl C, El-Daou H, Athwal KK, Gupte CM, Weiler A, Williams A, et al. The Role of the Anterolateral Structures and the ACL in Controlling Laxity of the Intact and ACL-Deficient Knee. Am J Sports Med 2016;44:345-54. [Google Scholar] |
| 19. | Parsons EM, Gee AO, Spiekerman C, Cavanagh PR. The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med 2015;43:669-74. [Google Scholar] |
| 20. | Van der Watt L, Khan M, Rothrauff BB, Ayeni OR, Musahl V, Getgood A, et al. The structure and function of the anterolateral ligament of the knee: A systematic review. Arthroscopy 2015;31:569-82000. [Google Scholar] |
| 21. | Rasmussen MT, Nitri M, Williams BT, Moulton SG, Cruz RS, Dornan GJ, et al. An In vitro Robotic Assessment of the Anterolateral Ligament, Part 1: Secondary Role of the Anterolateral Ligament in the Setting of an Anterior Cruciate Ligament Injury. Am J Sports Med 2016;44:585-92. [Google Scholar] |
| 22. | Nitri M, Rasmussen MT, Williams BT, Moulton SG, Cruz RS, Dornan GJ, et al. An In vitro robotic assessment of the anterolateral ligament, Part 2: Anterolateral ligament reconstruction combined with anterior cruciate ligament reconstruction. Am J Sports Med 2016;44:593-601. [Google Scholar] |
| 23. | Ferretti A, Monaco E, Fabbri M, Maestri B, De Carli A. Prevalence and classification of injuries of anterolateral complex in acute anterior cruciate ligament tears. Arthroscopy 2017;33:147-54. [Google Scholar] |
| 24. | Helito CP, Demange MK, Bonadio MB, Tirico LE, Gobbi RG, Pecora JR, et al. Radiographic landmarks for locating the femoral origin and tibial insertion of the knee anterolateral ligament. Am J Sports Med 2014;42:2356-62. [Google Scholar] |
| 25. | Slichter ME, Wolterbeek N, Auw Yang KG, Zijl JAC, Piscaer TM. A novel test for assessment of anterolateral rotatory instability of the knee: The tibial internal rotation test (TIR test). J Exp Orthop 2018;5:29. [Google Scholar] |
| 26. | Helito CP, Demange MK, Helito PV, Pereira CP, Batista BM, Pecora JR, et al. Marcelo. Evaluation of the anterolateral ligament of the knee by means of magnetic resonance examination. Rev Bra Ortop 2015:2:214-9. [Google Scholar] |
| 27. | Claes S, Bartholomeeusen S, Bellemans J. High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg 2014;80:45-9. [Google Scholar] |
| 28. | Cohen J. A coefficient of agreement for nominal scales. Educational and psychological measurement. Educ Psychol Meas1960;20:37-46. [Google Scholar] |
| 29. | Fleiss J. Measuring nominal scale agreement among many raters. Psychol Bull 1971;76:378-82. [Google Scholar] |
| 30. | Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. [Google Scholar] |
| 31. | Taneja AK, Miranda FC, Braga CA, Gill CM, Hartmann LG, Santos DC, et al. MRI features of the anterolateral ligament of the knee. Skeletal Radiol 2015;44:403-10. [Google Scholar] |
| 32. | Sonnery-Cottet B, Daggett M, Fayard JM, Ferretti A, Helito CP, Lind M, et al. Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament-deficient knee. J Orthop Traumatol 2017;18:91-106. [Google Scholar] |
| 33. | Carpenter RD, Majumdar S, Ma CB. Magnetic resonance imaging of 3-dimensional in vivo tibiofemoral kinematics in anterior cruciate ligament-reconstructed knees. Arthroscopy 2009;25:760-6. [Google Scholar] |
| 34. | Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat 2013;223:321-8. [Google Scholar] |
Fulltext Views
4,422
PDF downloads
1,821





