Translate this page into:
Single and double hamstring tendon anterior cruciate ligament reconstruction – A prospective, comparative cohort study
*Corresponding author: Assala Abu-Mukh, Department of Orthopedics and Traumatology, Vita-Salute San Raffaele University - San Raffaele Hospital, Milan, Lombardy, Italy. abumukh.assala@hsr.it
-
Received: ,
Accepted: ,
How to cite this article: Chillemi M, Abu-Mukh A, Tei MM, Pace V, Bartoli M, Cerulli G, et al. Single and double hamstring tendon anterior cruciate ligament reconstruction – A prospective, comparative cohort study. J Musculoskelet Surg Res 2022;6:148-53.
Abstract
Objectives:
Excellent knee stability is necessary to achieve good postoperative clinical results in anterior cruciate ligament (ACL) reconstruction. However, there is little evidence in the literature regarding hamstring graft choice for ACL reconstruction. Our study intended to debate the best autograft choice for this procedure. We aimed to examine the functional and biomechanical outcomes of three different autografts used in ACL reconstruction, namely, Semitendinosus and Gracilis quadrupled (STGR) autograft, tripled or quadrupled ST autograft, and tripled Gracilis tendon autograft (GR).
Methods:
We conducted an observational, comparative, prospective cohort on 248 ACL reconstructed patients spanning 2 years (2009–2010) and evaluated the primary outcome with KT-1000 knee arthrometer and secondary outcomes with International Knee Documentation Committee (IKDC), Tegner ctivity cale, and Lysholm score.
Results:
The data suggest a statistically significant increase in IKDC score and Lysholm score in the GR group – standing for better subjective outcomes like pain – compared to the STGR and ST groups (P = 0.0018 and P = 0.0034, respectively) and statistically non-significant differences between the STGR and ST groups for all evaluated parameters. KT-1000 side-to-side evaluation demonstrates that STGR autograft offers less structural knee laxity compared to GR autograft in ACL reconstruction (P = 0.044).
Conclusion:
The study found that STGR autograft offers more stability to the knee compared to the GR autograft alone yet is associated with inferior subjective outcomes compared to the GR group. GR autograft is a valid substitute for ACL reconstruction, especially in patients presenting with hyperlaxity or demanding lower functional performance.
Keywords
Anterior cruciate ligament reconstruction
Gracilis
Hamstrings
Semitendinosus
Knee injuries
Outcome
INTRODUCTION
A good reconstruction outcome of the anterior cruciate ligament (ACL) is achievable using various grafts and surgical techniques.[1,2] Due to their characteristics, hamstring tendons are commonly used.[3] What surgical technique or graft type to choose depends on the individual case and is molded based on concomitant factors such as knee and limb injuries and the surgeon’s expertise and preference.[4]
The use of hamstring tendons offers advantages over the bone-patellar tendon-bone graft, such as reduced inferior patellar contracture, quadriceps weakness, and donor site morbidity.[5,6]
Semitendinosus and Gracilis quadrupled grafting (STGR) evidenced sufficient mechanical strength and satisfying outcomes in terms of joint stability, becoming a suitable alternative for ACL reconstruction. However, studies proved that STGR grafting impacts knee performance-limiting active knee flexion, accentuating muscle weakness[7] up to 9 months after surgery, and lowering internal tibial torque and joint stability, thus negatively affecting athletic performance.[8]
Over the past two decades, neurophysiological[9] and biomechanical[10] discoveries such as all-inside techniques[11] led surgeons to opt for a onetendon approach.[10] We found little evidence in the literature referring to Gracilis tendon (GR) grafting.[12-14]
We were intrigued to examine ACL reconstruction using different autografts to provide standardized indications when choosing tendon grafts for ACL reconstruction. Thus, we compared the performance of ACL reconstruction using different autografts: ripled GR autograft, STGR, and tripled or quadrupled ST autografts.
We conducted a prospective, comparative cohort study to provide standardized indications that evaluate the pros and cons when choosing tendon grafts for ACL reconstruction to clinically and functionally inquire different outcomes between the mentioned groups.
MATERIALS AND METHODS
Design
We conducted a prospective, comparative cohort study including 311 patients who underwent ACL reconstruction using hamstring tendon autografts over 24 months (2009– 2010). We diagnosed the ACL injury based on our center’s standard protocol that includes accurate medical history, physical examination, and the use of a KT-1000 arthrometer. The diagnosis was confirmed using magnetic resonance imaging for all cases. In our center’s policy, all ACL ruptures are operated on. additionally addition, the ligaments status, and concomitant injuries were assessed and confirmed intraoperatively.
The atients were randomly grouped using a selection algorithm into quadrupled STGR and tripled or quadrupled ST grating. Consequently, one out of four patients was randomly selected for tripled GR grafting using the algorithm. This method was cautiously chosen because the GR autograft use alone has not been described in the literature and presented as an initial approach.
We considered a previous or concomitant ligamentous injury, significant trauma, significant meniscal damage, contralateral knee injury, concurrent fracture, severe osteoarthritis, and loss in follow-up as exclusion criteria due to possible confounders interfering with the study outcome. Intermediate clinical evaluations were performed without data collection.
Out of 311 candidates who presented with ACL injury included in the study, 21 were excluded for concomitant major meniscal lesions, other pathological findings, and bilateral injuries to avoid confounders. A total of 42 were lost during follow-up. At the end of the 5-year follow-up, 248 patients concluded the study; 44 were women (17.8%) and 204 were men (82.2%).
We divided the patients into three groups based on the team’s evaluation and treatment choice; we included 98 patients in the STGR group (Group 1), 63 in the GR group (Group 2), and 87 in the ST group (Group 3) [Figure 1]. The candidates were homogenously distributed between groups to avoid confounders. We conducted the follow-up and observation consequently.
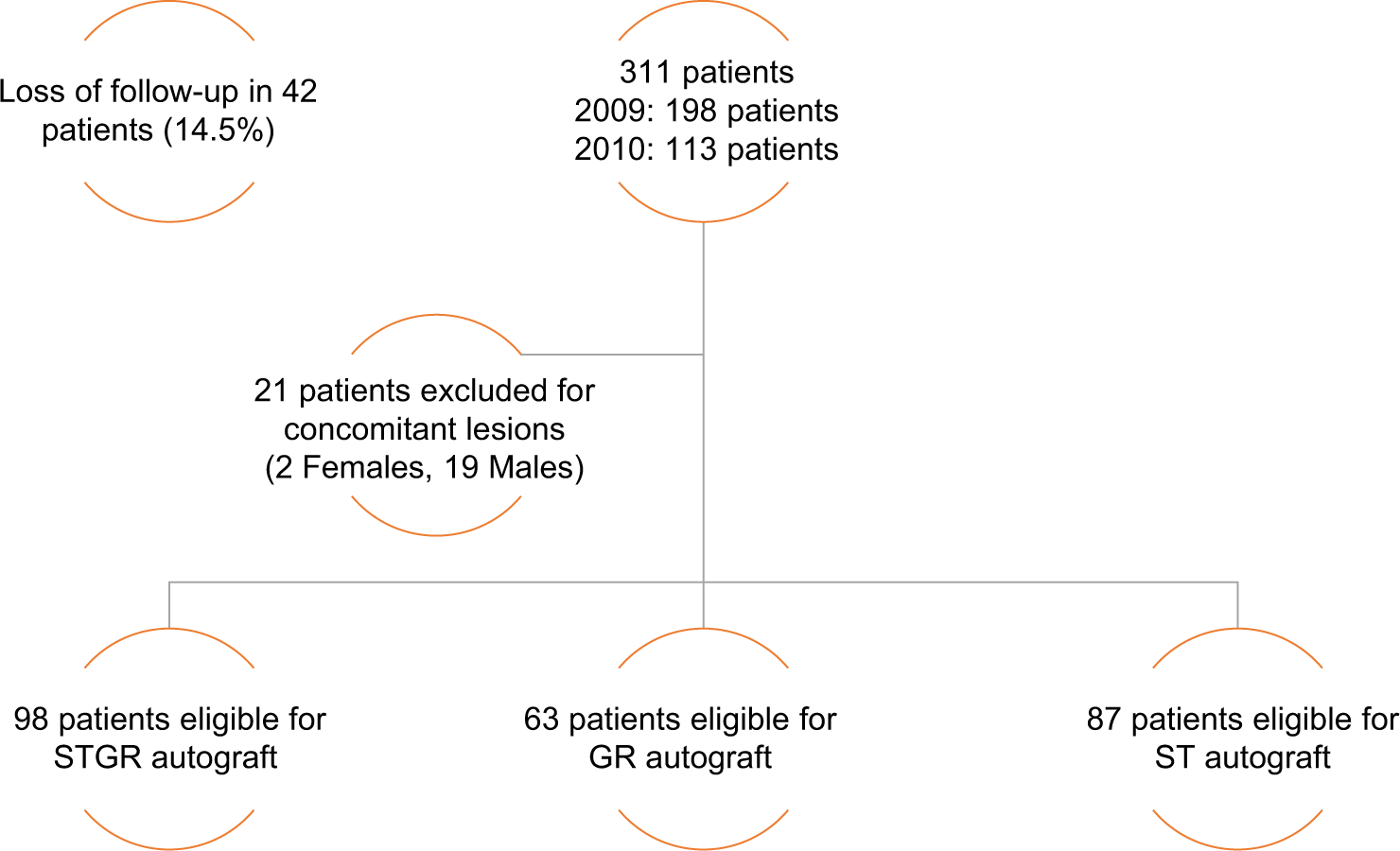
- Flowchart illustrating the exclusion and distribution of patients. STGR: Gracilis and semitendinosus, ST: Semitendinosus, GR: Gracilis.
The same investigators evaluated all groups postoperatively at 5 years. The primary outcome was to evaluate knee stability using a KT-1000 knee arthrometer. Secondary evaluated outcomes were post-operative knee specific symptoms by Lysholm score, sports activity, and knee function outcomes using International Knee Documentation Committee (IKDC), and comparison between pre-operative and postoperative work and sports activities using Tegner ctivity cale was made.
Surgical technique and post-operative program
All cases were operated by the same surgeon (G.C.) using standardized techniques: arrying out independent tunneling with all-inside technique, preserving the ACL remnants with a two-incision technique and fixing the graft with femoral endo-button and tibial screw. The procedure details are described in the cited publication.[11]
The rehabilitation care center provided all patients with the same intensive rehabilitation program immediately following surgery with early passive range of movement and weight-bearing exercises. We encouraged active knee flexion (up to 90°) and quadriceps exercises after the 1st post-operative week and authorized patients to bear partial weight with the knee brace fixed in extension from post-operative day 1 and removed the knee brace after 3 weeks. In addition, we prescribed Acetaminophen and encouraged ice applications. Full knee flexion and complete weight-bearing were permitted 1 month after surgery and in the presence of adequate muscular recovery; sports were approximately introduced after the 5th post-operative month.
Data collection and evaluation
We assessed all operated and followed patients in two specialized centers. additionally addition, we reviewed the patients’ clinical notes and electronic hospital records for data collection. Data were collected prospectively and recorded using Microsoft Excel. The primary outcome evaluated knee stability measuring anterior tibial translation at 5 years with a KT-1000 arthrometer during physical examination. The secondary outcomes were subjective assessments using IKDC, Tegner activity scale, and Lysholm score in the three groups.
A total of 248 patients (80%) matched our inclusion criteria and underwent the before mentioned evaluations at 5 years, while the remaining 63 patients were excluded from the study or lost during follow-up [Figure 1].
Analysis
We used GraphPad Prism version 6.2 for Mac OSX (GraphPad Software, La Jolla, California, USA) for statistical data analysis. We used the Chi-square test to compare the recurrence of instability rate and the Mann–Whitney U-test for comparison to evaluate the non-parametric variables (IKDC, Lysholm, Tegner score, and KT-1000 side-to-side difference).
Considering the primary outcome of translation on KT-1000, we assumed the minimum clinical significance (defined as anterior-posterior knee laxity in KT-1000 side-to-side difference) to be 3 mm or more.[15,16] We calculated a minimum sample size of 60 patients per group to find statistically significant differences between groups at an alpha level of 0.1 and power of 90%.
RESULTS
After surgery, the STGR, GR, and ST groups averaged 91.52, 96.94, and 92.79 on IKDC, respectively, and Lysholm score averages were 95.88, 97.42, and 95.87, respectively. The Tegner score changed preoperatively to postoperatively by –0.53, –0.63, and –0.89 on the STGR, GR, and ST groups, respectively. KT-1000 side-to-side difference in postoperative scored 2.06, 2.55, and 2.22 on the STGR, GR, and ST groups, respectively.
The overall instability recurrence rate (defined as new onset of instability using KT-1000 after surgery) was relatively low. However, the study suggests a higher – yet not statistically significant – instability recurrence rate in the GR autograft group compared to other groups. The overall instability recurrence rate averaged 8.06% (nine patients, of which eight were male and one was female). Instability recurred in 9.2% of the STGR group, 4.6% in the ST group, and 11.1% in the GR group [Table 1].
| M | F | Total | I.M. | I.F. | Total I | I Percentage | |
|---|---|---|---|---|---|---|---|
| STGR | 90 | 8 | 98 | 8 | 1 | 9 | 9.2 |
| ST | 69 | 18 | 87 | 3 | 1 | 4 | 4.6 |
| GR | 47 | 16 | 63 | 5 | 2 | 7 | 11.1 |
| Total | 206 | 42 | 248 | 16 | 4 | 20 | 8.1 |
M: Male, F: Female, I.M.: Instability recurrence in males, I.F.: Instability recurrence in females, Total I: Total instability recurrence, I Percentage: Percentage of instability. STGR: Gracilis and semitendinosus, ST: Semitendinosus, GR: Gracilis
On the subjective evaluation using IKDC, Lysholm, and pre-to-post-operative Tegner scores, the following data were obtained [Table 2]. IKDC scored lowest in the STGR group and highest in the GR group, reaching statistical significance only when comparing STGR with GR (P = 0.0018) and ST with the GR groups (P = 0.0034). The GR group had the highest IKDC and Lysholm scores, but Lysholm score significantly differed only between the ST and GR groups (P = 0.022).
| STGR group | GR group | ST group | P-value (significance if P<0.05) | |||
|---|---|---|---|---|---|---|
| STGR versus GR | STGR versus ST | ST versus GR | ||||
| IKDC | 91.52 (SD 14.51) | 96.94 (SD 5.84) | 92.79 (SD 9.77) | P=0.0018 | n.s. | P=0.0034 |
| Lysholm | 95.88 (SD 8.69) | 97.42 (SD 4.42) | 95.87 (SD 6.65) | n.s. | n.s. | P=0.022 |
| Δ Tegner | -0.53 (SD 1.13) | -0.63 (SD 1.36) | -0.89 (SD 1.32) | n.s. | n.s. | n.s. |
| KT-1000 | 2.06 (SD1.02) | 2.55 (SD 1.48) | 2.22 (SD 1.17) | P=0.044 | n.s. | n.s. |
Statistical significance was considered when P<0.05. STGR: Gracilis and semitendinosus, ST: Semitendinosus, GR: Gracilis
Instability recurrence analysis (as above defined) using KT-1000 showed a significant difference between the STGR and GR groups; the STGR group had more stability than the GR group.
Although the delta in Tegner scores (∆ Tegner) from before to after surgery decreased for all groups, none of the differences were statistically significant.
DISCUSSION
A noteworthy finding of this study is that when using STGR autograft compared to the GR group, KT-1000 side-to-side presents lesser laxity and the difference reached statistical significance. This correlates to higher knee stability (as STGR is thicker) and is associated with inferior subjective outcomes. Considering both IKDC and Lysholm scores, pain and functional knee impairment peak in both the ST and STGR groups compared to the GR autograft group.
Many studies examined ACL reconstruction with different surgical procedures, illustrating different standards and indications. However, this led to conflicting results concerning some aspects, such as muscular atrophy in STGR autografting.[17] Graft choice and single versus double tendon reconstructions,[18,19] most surgeons favor STGR reconstruction with a quadrupled hamstring tendon.[20-24] Our findings indicate that the use of GR graft reduces knee symptoms, yet that STGR and ST graft offer better knee stability.
We acknowledge that accepting a high error level (0.1) limits the power of our study yet considering the period in which we performed our observation, we expected that the average number of patients with ACL reconstruction would not allow a higher statistical power. In addition, we found limited evidence in the literature regarding ACL reconstruction using GR tendon only to compare our results with. This led us to consider GR autograft performance in our patient pool.
We would like to add that although a part of our evaluation assessed subjective (Tegner, IKDC, and Lysholm) patient scores, we believe in their validity and consider the post-operative experience of our patients as the ultimate target.
We believe that the treatment should never overlook a personalized approach that should be molded on the individual case and is necessary to obtain the best feasible outcome. Therefore, we encourage further studies aimed at considering treatment costs of early and late complications in ACL reconstruction.
Studies demonstrated that pain and hamstring muscle atrophy limit STGR autograft use in ACL reconstruction.[19] We presume that GR autograft – although it leads to lower knee stability compared to STGR – is a reasonable substitute for ACL reconstruction, particularly in certain cases. Knees requiring a lesser functional demand or presenting with hyperlaxity may benefit from GR autograft ACL reconstruction.
We aspire to restore knee function while maintaining knee stability after ACL reconstruction with autografts and believe that more studies on the best autograft choice will get us one step closer to reaching this goal.
CONCLUSION
We conclude that choosing one tendon autograft in ACL reconstruction is a valid approach. However, using GR autograft offers less knee stability, and should be considered when operating knees that present hyperlaxity or require limited functional demand. GR alone autograft is correlated with better subjective outcomes. In addition, the KT-1000 side to side indicates that STGR autograft guarantees higher structural knee stability but is associated with less controlled pain compared to GR tendon autografting.
AUTHORS’ CONTRIBUTIONS
CM, TMM, and CG conducted the study, participated in the operations, and evaluated patients postoperatively. PV and BM selected, collected, and analyzed the patient’s database before and at follow-up. The coordination and the drafting were made by PG and final revision, rewriting, and editing was made by AA. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the I.r.t.a.l. Ethics Committee. The approval was obtained in May 2014.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patients consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICTS OF INTEREST
There are no conflicts of interest.
References
- Long-term follow-up of patellar tendon grafts or hamstring tendon grafts in endoscopic ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2013;21:576-83.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction: A multicenter prospective cohort study evaluating 3 different grafts using same bone drilling method. Clin J Sports Med. 2011;21:294-300.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective randomized study of anterior cruciate ligament reconstruction a comparison of the patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med. 2007;35:384-94.
- [CrossRef] [PubMed] [Google Scholar]
- How to choose the ideal graft for anterior cruciate ligament reconstruction. Rev Med Suisse. 2017;13:1339-42.
- [CrossRef] [PubMed] [Google Scholar]
- Rupture of the patellar ligament after use of its central third for anterior cruciate reconstruction. A report of two cases. J Bone Joint Surg Am. 1984;8:1294-7.
- [CrossRef] [Google Scholar]
- Fractures associated with patellar ligament grafts in cruciate ligament surgery. Bone Joint J. 1992;74:617-9.
- [CrossRef] [PubMed] [Google Scholar]
- Graft site morbidity with autogenous semitendinosus and gracilis tendons. Am J Sports Med. 1995;23:706-14.
- [CrossRef] [PubMed] [Google Scholar]
- Neuromuscular control of the hamstrings to protect the ACL: In vivo experimentation. J Biomech. 2006;39:S190-1.
- [CrossRef] [Google Scholar]
- Biomechanical evaluation of using one hamstrings tendon for ACL reconstruction: A human cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2010;18:11-9.
- [CrossRef] [PubMed] [Google Scholar]
- The true story of the original All-Inside Technique for biological ACL reconstruction. J Orthop. 2011;3:93-100.
- [Google Scholar]
- The gracilis tendon autograft is a safe choice for orthopedic reconstructive procedures: A consecutive case series studying the effects of tendon harvesting. BMC Musculoskelet Disord. 2019;20:138.
- [CrossRef] [PubMed] [Google Scholar]
- Can the gracilis replace the anterior cruciate ligament in the knee? A biomechanical study. Int Orthop. 2016;40:1647-53.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated gracilis tendon harvesting is not associated with loss of strength and maintains good functional outcome. Knee Surg Sports Traumatol Arthrosc. 2020;28:637-44.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation between hamstring flexor power restoration and functional performance test: 2-year follow-up after ACL reconstruction using hamstring autograft. Knee Surg Relat Res. 2012;24:113-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of additional gracilis tendon harvest on muscle torque, motor coordination, and knee laxity in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1287-92.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of semitendinosus and gracilis harvest in anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:1177-85.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of results after anterior cruciate ligament reconstruction using a four-strand single semitendinosus or a semitendinosus and gracilis tendon. Knee Surg Sports Traumatol Arthrosc. 2015;23:3238-43.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy. 2005;21:791-803.
- [CrossRef] [PubMed] [Google Scholar]
- Return to sport activity after anterior cruciate ligament reconstruction in skeletally immature athletes with manual drilling original all inside reconstruction at 8 years follow-up. Acta Orthop Traumatol Turc. 2016;50:635-8.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior cruciate ligament graft positioning, tensioning and twisting. Knee Surg Sports Traumatol Arthrosc. 1998;6(Suppl 1):S2-12.
- [CrossRef] [PubMed] [Google Scholar]
- Why autologous hamstring tendon reconstruction should now be considered the gold standard for anterior cruciate ligament reconstruction in athletes. Br J Sports Med. 2009;43:325-7.
- [CrossRef] [PubMed] [Google Scholar]
- An international survey on anterior cruciate ligament reconstruction practices. Int Orthop. 2013;37:201-6.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of randomized controlled clinical trials comparing hamstring autografts versus bone-patellar tendon-bone autografts for the reconstruction of the anterior cruciate ligament. Arch Orthop Trauma Surg. 2012;132:1287-97.
- [CrossRef] [PubMed] [Google Scholar]






