Translate this page into:
Staged bilateral Colonna arthroplasty in an adolescent within a 10-month difference: A case report with a literature review
*Corresponding author: Matias Sepulveda, Institute of Medical Specialities, Universidad Austral de Chile, Valdivia, Los Ríos, Chile. matias.sepulveda@uach.cl
-
Received: ,
Accepted: ,
How to cite this article: Arévalo G, Birrer E, Slongo T, Sepulveda M. Staged bilateral Colonna arthroplasty in an adolescent within a 10-month difference: A case report with a literature review. J Musculoskelet Surg Res. doi: 10.25259/JMSR_101_2025
Abstract
Colonna capsular arthroplasty is an intervention that has gained interest in recent years by adopting the controlled hip dislocation approach. In this report, we present the case of a 15-year-old adolescent with a history of congenital bilateral hip dislocation without prior treatment. She presented with significant symptoms, pain after activity, bilateral Trendelenburg gait, more remarkable on the left, symmetrical lower extremity length, and altered range of hip motion. Radiographs showed a Crowe IV high hip dislocation in a Sommerville stage III. Surgical treatment was performed, with modified Colonna capsular arthroplasty, associated with femoral shortening osteotomy and lateral acetabular augmentation, bilaterally, with 10 months between the two hips. In the 4-year follow-up, the patient was without coxalgia, walking without Trendelenburg gait, with a painless complete range of motion, without lower limb difference, and with high patient satisfaction. Radiographic evaluation showed centered hips with preserved joint space. Based on the result, we can point out that modified Colonna capsular arthroplasty can once again be an effective surgical technique, with excellent functional results, even in bilateral cases, accompanied by adequate rehabilitation and strict clinical and radiographic follow-up.
Keywords
Adolescent orthopedics
Colonna arthroplasty
Congenital hip dislocation
Developmental hip dysplasia
Surgery
INTRODUCTION
Persistent congenital high hip dislocation in adolescents is a complex pathology that involves the acetabulum and the proximal femur. It alters normal hip biomechanics, predisposing to the future development of hip osteoarthritis (OA).[1] At the age of over 8 years old, there are, up to now, no reasonable solutions to reconstruct the hip. As the acetabulum is strongly involved and mostly non-existent, even the modern types of acetabular re-orientation operations, such as triple osteotomy or the periacetabular osteotomy (PAO), are not successful, as no good articular congruence can be achieved. A useful procedure in this situation is the Chiari pelvic osteotomy, which can be used in patients with dysplastic acetabular sockets, sometimes combined with an additional bone augmentation procedure.[2] The other option is total hip replacement, which is a surgically demanding procedure with the need for additional femoral shortening.[3]
Colonna capsular arthroplasty is a surgical procedure for managing congenital hip dislocation in children and young adults.[4,5] The technique was first described by Codivilla in 1901 and later popularized by Colonna in 1932 and Hey Groves in 1962. In 1932, Colonna published the first three cases using a technique for anatomical reduction and correct positioning of a high dislocated hip, using a new type of arthroplasty.[6] This was based on a newly created cavity by reaming and interposing the elongated joint capsule, which, over time, will transform into fibrous cartilage. The results of this technique were not as good as expected and fell into disuse in the 70s. With the introduction of the safe method of surgical hip dislocation by Ganz et al.,[7] this surgical procedure resurfaces. The improvement of the arthroplasty described by Colonna is the possibility of clear visualization and detachment of the joint capsule from the acetabulum through his approach.
When the diagnosis of developmental hip dysplasia (DDH) is made early, management can achieve good to excellent results with a simpler treatment, but when a correct diagnosis is not made or is made late, surgical management is frequently needed, often with mixed results. Late presentation is defined as when DDH is not detected in the first 3 months from birth, with rates varying from 0.07 to 2.0/1000 births. Late diagnosis is seen particularly in developing countries, such as India and South America, and the most common cause is the failure or absence of adequate screening during the first month of life. Surgical treatment to prevent OA is known as hip preservation surgery. Various techniques, such as pelvic osteotomies and hip arthroscopy, have been described and included in this concept. For skeletal immature patients, capsular arthroplasty is an interesting alternative.
In the present report, we show the case of a patient treated using this technique, modified by surgical dislocation of the hip [7] performed bilaterally, which is scarcely reported in the literature, covering <10% of the cases. In this report, we show excellent functional results, without complications inherent to surgery, following a neat technique. We accompany this with a literature review, with the authors’ current treatment recommendations.
CASE REPORT
The case corresponds to a 15-year-old adolescent with a history of congenital high bilateral hip dislocation, without prior treatment. She presented with bilateral hip pain, predominantly left, with no history of trauma. She has no relevant family or obstetric history of the mesomorphic constitution with a body mass index of 20.4 kg/m2. A bilateral Trendelenburg gait stands out, more on the left, with minimal lower limb length discrepancy (0.5 cm). The range of motion (ROM) of the hips generates mild pain, achieving 90° flexion bilaterally, abduction of 40° to the right and 35° to the left, internal rotation of 30° to the right and 35° to the left, and external rotation of 35° bilaterally.
The radiographic study showed a congenital high hip dislocation in Sommerville stage III, with chronic bilateral Crowe type IV superior dislocation [Figure 1]. Computed tomography demonstrated posterior support, without stable pseudo-acetabulum formation [Figure 2].

- A 15-year-old girl with a bilateral high dislocated hip. Pelvis anteroposterior view radiograph shows a congenital high hip dislocation in Sommerville stage III, with chronic bilateral Crowe type IV superior dislocation.
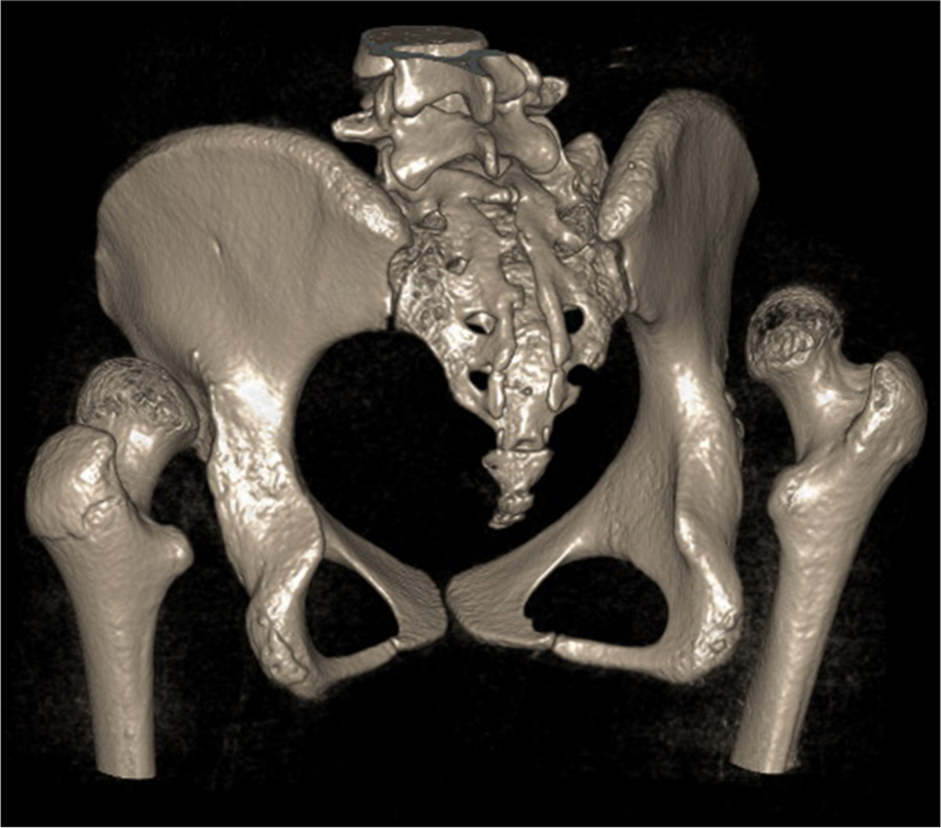
- A 15-year-old girl with a bilateral high dislocated hip. Computed tomography scan reconstruction shows a lack of pelvic support without stable pseudo-acetabulum formation.
Therapeutic options were discussed with the patient and her family. An evaluation with the joint replacement surgery team was conducted. It was concluded that, given the technical means and specialized support, we could perform reconstructive surgery that would allow us to achieve a stable, pain-free hip, with the possibility of gaining some years before a joint replacement. The joint replacement team’s feedback on this decision was that, in their experience, an acetabulum previously prepared with a Colonna is much more anatomically congruent for the acetabular components and also has more stability. Furthermore, after the Colonna procedure, the dysplastic femur undergoes remodeling changes that allow the use of non-tapered stems, enabling a standard joint replacement. Added to this is the fact that neither sciatic release nor femoral shortening will be required at the time of a joint replacement, reducing the expected surgical morbidity. With all these considerations, it was decided to proceed with the Colonna capsular arthroplasty.
It was planned to release the sciatic nerve and perform femoral shortening to avoid neurological damage, seeking to preserve the symmetrical length of the lower limbs. She underwent staged surgery, first on the right side, and after 10 months, on the left side. Using a lateral Gibson approach for a controlled surgical hip dislocation performed according to the Ganz technique, achieving complete exposure of the acetabular cavity and allowing circumferential dissection of the capsule from its neighboring muscles, taking care not to damage the medial circumflex artery. The anterior “T” capsulotomy is performed as close to the acetabular rim as possible. The next stages of the technique follow the line described by Ganz et al.[6,7] Colonna capsular arthroplasty was performed, with a modified approach, a femoral shortening osteotomy, and lateral acetabular augmentation with a graft from a resected femoral fragment [Figure 3].
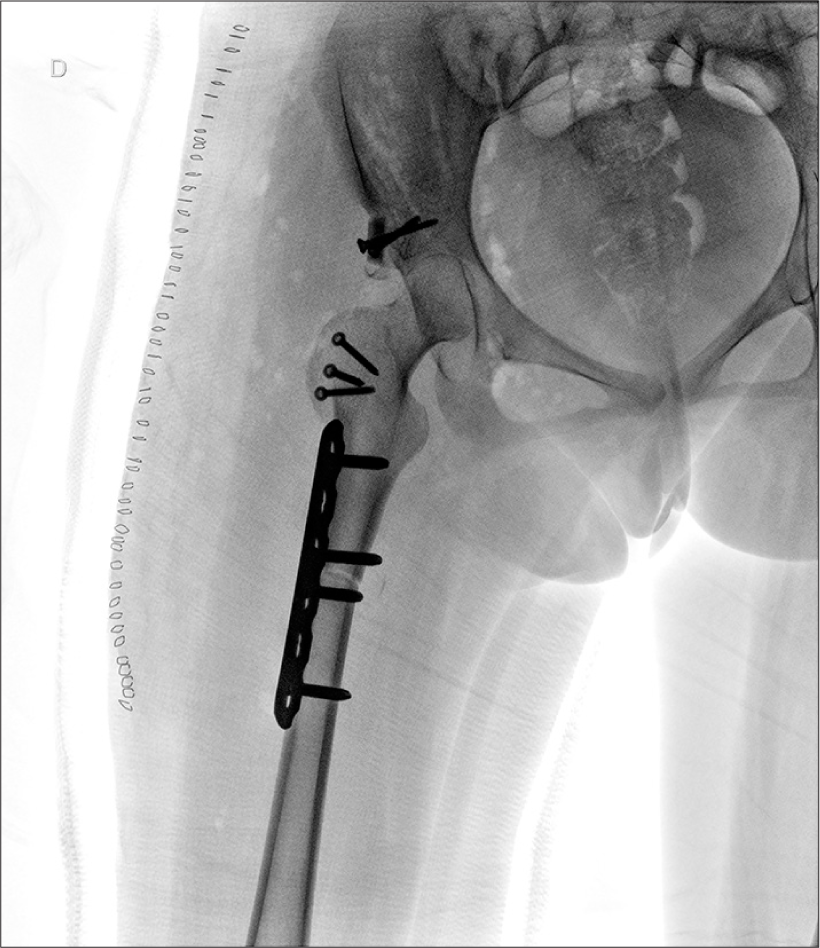
- Right hip anteroposterior view radiograph after a Colonna capsular arthroplasty was performed through a controlled surgical hip dislocation, associated with a femoral shortening osteotomy and lateral acetabular bone augmentation.
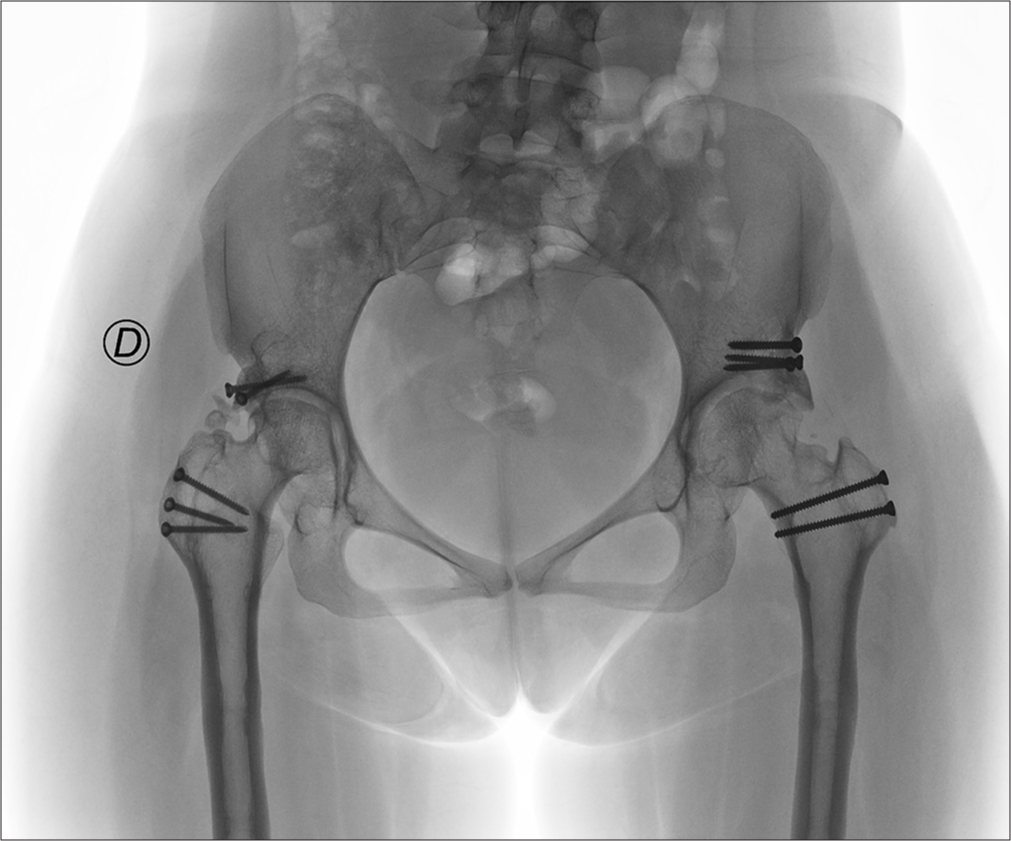
The postoperative protocol was immobilization with a spica cast and unloading for 6 weeks. After six weeks, the cast was removed, and the hip was protected with a hip abduction brace for another six weeks, allowing hip mobilization. At four months post-surgery, she began with protected weight bearing with two crutches, and at six months, full weight bearing was allowed. Ten months after the first procedure, contralateral surgery was performed, following the exact same technique, with no complications [Figure 4]. Two years after the first surgery, the removal of the femur osteosynthetic was scheduled [Figure 5].
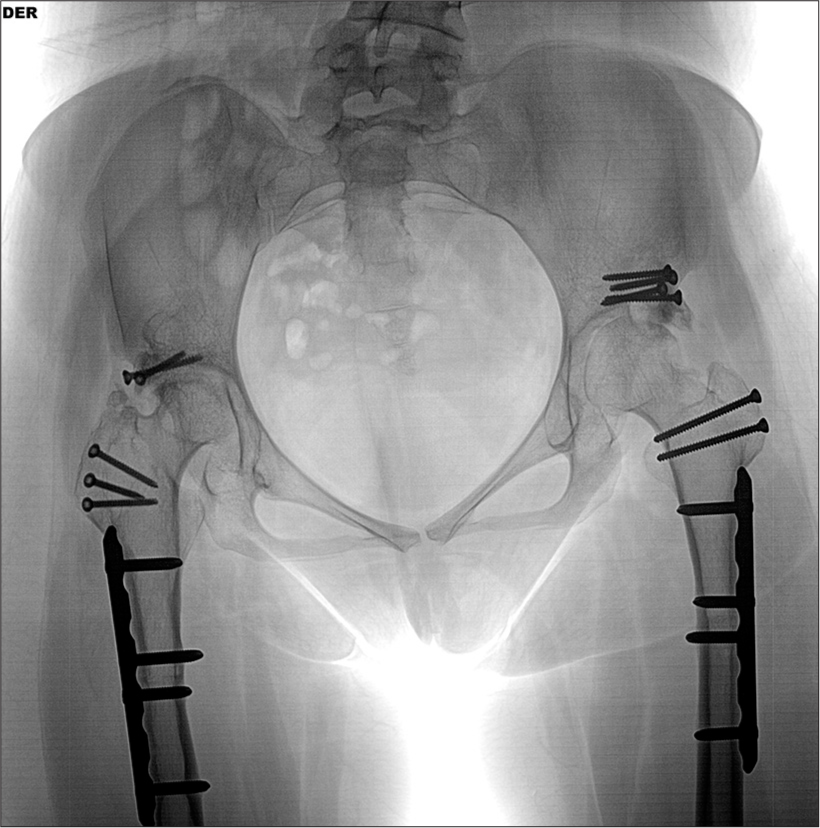
- A pelvis anteroposterior view radiograph after the left hip Colonna capsular arthroplasty was performed, 10 months after the first procedure on the right side.

- A pelvis anteroposterior view radiograph after hardware removal of femur osteosynthesis, 2 years after the first surgery.
At four years of follow-up, the patient did not have hip pain and could walk without Trendelenburg gait, with complete, symmetrical, painless ROM. There was no difference in length in the lower limbs. The radiograph showed reduced, centered femoral heads, with preserved joint space and consolidated osteotomies [Figure 6]. Radiographically, it represented a Tönnis 0, and in the clinic, she had an excellent functional result with a Harris Hip Score (HHS) of 100 points.
- A pelvis anteroposterior view radiograph demonstrates preserved joint space and consolidated osteotomies, 6 years after the first surgery.
DISCUSSION
Capsular arthroplasty is a hip preservation surgery developed to treat congenital hip dislocation, especially in cases where treatment has been delayed. It has an important role in young patients older than 9 years, with preserved femoral head cartilage and with subluxation or complete hip dislocation, in which open reduction, combined with re-directional femoral or acetabular orientation, produces a high risk of recurrence.[4]
Its concept involves a two-stage procedure. The first stage focuses on overcoming soft tissue contractures by continuous limb traction, while the second stage focuses on open reduction and insertion of the femoral head, covered by the joint capsule, into a reconstructed acetabulum. It is technically demanding and has a high incidence of complications, such as avascular necrosis (AVN) and joint stiffness. This procedure, which was common in the 1960s, is currently out of use.[7,8]
Stans and Coleman reported long-term results in 22 hips of 20 patients, demonstrating that a shortening rotational femoral osteotomy allows preoperative traction to be abandoned, with highly satisfactory results and a low prevalence of AVN.[9]
This Codivilla-Hey Groves-Colonna technique was modified in 2012 by Ganz et al.,[7] who reported a series of 9 patients with 1-stage surgery, a technique on which the resolution of the current case was based.
While Colonna himself primarily advocated this procedure in unilateral cases, subsequent studies have explored its application in bilateral dislocations, with variable results. Recent literature reports the use of this technique in a few cases of congenital hip dislocation, and it is even less used in bilateral cases. In what is reported, a period of 4 weeks of difference is described between each intervention, allowing the cast to be removed before surgery on the second hip.
A key consideration in bilateral Colonna arthroplasty is the possibility of reduced ROM and joint stiffness, which may present more significant limitations compared to unilateral cases.[4,8] Long-term follow-up studies have reported promising results, including good walking ability, even with radiographic evidence of joint reformation.[10,11] However, the risk of complications such as AVN is close to 19%, and joint stiffness remains a concern, especially in bilateral procedures.[12] Other long-term studies have reported varying degrees of success, with patients experiencing excellent or good results on HHS by more than 50% after 17 years.[12] However, others faced unsatisfactory results, even more so in bilateral cases associated with joint stiffness.[8]
The most recent follow-up study of capsular arthroplasty involves 90 patients with DDH, carried out in China between 2012 and 2021. Only two bilateral cases were reported in this series, with a modified HHS of 83.61 and joint stiffness as the main complication, at 14.1%.[4]
Patient selection and meticulous surgical technique are paramount to obtaining good results. The indications of this surgical procedure are severe chronic subluxation with acetabular cartilage destruction or absence, or high congenital hip dislocation, in patients between 10 and 25 years old. It is contraindicated for severely deformed femoral heads or femoral head cartilage damage due to joint incongruency and stiffness risk. Special consideration should be taken in cases of subluxation, where the femoral head is at the level of the acetabulum, and the joint capsule is small and not elongated enough to cover the entire femoral head.
Colonna surgery, by a safe surgical hip dislocation, associated with a subtrochanteric osteotomy, allows management in cases with significant acetabular deformity in patients over 10 years old, in which a triple PAO or Chiari osteotomy is not possible.[13] Augmentation with decellularized dermal allograft has even been reported in cases lacking an adequate capsule, allowing a durable interposition surface.[14]
CONCLUSION
With a proper patient selection and meticulous surgical technique, the modified Colonna capsular arthroplasty can be an effective treatment, with excellent functional results, allowing to achieve a stable, pain-free hip, with the possibility of gaining some years before the need of a total joint replacement, that will have a lower expected surgical morbidity.
Acknowledgment:
This manuscript was supported by protected working time by the Graduate School of Medicine of the Universidad Austral de Chile, Valdivia, Chile.
Authors’ contributions:
GA: Literature search, data acquisition, data analysis, statistical analysis, manuscript preparation. EB: Concept, design, data acquisition. TS: Concept, design, data acquisition, manuscript editing. MS: Concept, design, definition of intellectual content, data analysis, manuscript preparation, manuscript editing. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published, and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI. Conflict of interest: There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Developmental dysplasia of the hip: Update of management. EFORT Open Rev. 2019;4:548-56.
- [CrossRef] [PubMed] [Google Scholar]
- Role of chiari osteotomy in treating degenerative hip arthritis: A review. J Clin Orthop Trauma. 2021;24:101687.
- [CrossRef] [PubMed] [Google Scholar]
- Total hip arthroplasty for high hip dislocation. Z Orthop Unfall. 2020;158:170-83.
- [CrossRef] [PubMed] [Google Scholar]
- The modified capsular arthroplasty for young patients with developmental dislocation of the hip. J Hip Preserv Surg. 2023;10:149-57.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital dislocation of the hip in older subjects. J Bone Joint Surg. 1932;14:277.
- [Google Scholar]
- Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119-24.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical technique: The capsular arthroplasty: A useful but abandoned procedure for young patients with developmental dysplasia of the hip. Clin Orthop Relat Res. 2012;470(11):2957-67.
- [CrossRef] [PubMed] [Google Scholar]
- Colonna capsular arthroplasty. A long-term follow-up of forty hips. J Bone Joint Surg Am. 1968;50:1305-26.
- [CrossRef] [Google Scholar]
- Colonna arthroplasty with concomitant femoral shortening and rotational osteotomy. Long-term results. J Bone Joint Surg Am. 1997;79:84-96.
- [CrossRef] [PubMed] [Google Scholar]
- Colonna capsular arthroplasty: A 33-year follow-up of four patients. Int Orthop. 1999;23:145-7.
- [CrossRef] [PubMed] [Google Scholar]
- The Colonna capsular arthroplasty. A long-term follow-up study of fifty-six patients. J Bone Joint Surg Am. 1971;53:1511-27.
- [CrossRef] [PubMed] [Google Scholar]
- The Colonna-hey groves arthroplasty in the late treatment of congenital dislocation of the hip. A long-term review. J Bone Joint Surg Br. 1987;69:220-8.
- [CrossRef] [PubMed] [Google Scholar]
- Capsular arthroplasty for neglected developmental dysplasia of hip. J Orthop Surg (Hong Kong). 2018;26:2309499018777888.
- [CrossRef] [PubMed] [Google Scholar]
- Capsular augmentation in Colonna arthroplasty for the management of chronic hip dislocation. J Hip Preserv Surg. 2018;5:34-8.
- [CrossRef] [PubMed] [Google Scholar]







