Translate this page into:
Submuscular bridge plating in the treatment of unstable femur fractures in children and adolescents
Corresponding Author:
Jamil Soni
Av Silva jardim 1502, 91, Curitiba, Paraná 80250 200
Brazil
jamilfsoni@hotmail.com
| How to cite this article: Valenza W, Soni J, Gasperin W, Faria F. Submuscular bridge plating in the treatment of unstable femur fractures in children and adolescents. J Musculoskelet Surg Res 2019;3:286-291 |
Abstract
Objectives: To evaluate the recommendations for submuscular bridge plating and the outcomes of this procedure in pediatric patients with unstable femur fractures. Methods: This was a retrospective analysis of 13 patients with unstable femur fractures treated over a period of 2 years. We analyzed the patients' age, mechanism of trauma, fracture type and location, follow-up duration, and associated injuries. The results were evaluated using the modified Flynn's criteria. Results: Overall, 12 patients were boys and 7 fractures affected the right femur. Two open fractures were classified as Gustilo Type IIIA. The mean age of the patients was 10.2 years. The mechanism of trauma included falls (n = 5), automobile accidents (n = 4), direct trauma (n = 2), and gunshot (n = 2). Six fractures involved the proximal third of the femur, whereas four involved the middle third and three involved the distal third. The fractures were long oblique in 7 cases, spiral in 2 cases, and comminuted in 4 cases. We had 11 excellent and 2 acceptable results. As for potential complications, we observed no pseudarthrosis, malalignment, or leg-length discrepancy. Conclusions: Despite the small number of patients in this study, submuscular bridge plating emerged as a viable and safe therapeutic alternative for unstable femur fractures and fractures in the distal and proximal femoral metaphysis in children and adolescents.Introduction
Femur fractures account for 1.4%–1.7% of all pediatric fractures and have an estimated annual rate of 19:100,000. They affect mainly preschool children and adolescents with twice as many boys as girls.[1],[2],[3] In younger children, femur fractures result from low-energy trauma, such as same-level falls, whereas in adolescents, they occur mostly due to high-energy trauma.[3] Of note, 80% of the femur fractures in children below the age of 18 months result from nonaccidental trauma.
The American Academy of Orthopaedic Surgery (AAOS) published in 2009 a clinical practice guideline for the treatment of diaphyseal femur fractures based on the age group.[4] For infants aged ≤6 months, the guideline recommends immobilization treatment with a Pavlik harness. For children between the ages of 6 months and 5 years, the treatment of choice is noninvasive reduction and immobilization with early spica casting; however, in high-energy fractures with important shortening, the options are traction followed by cast immobilization after initial bone callus formation or surgical stabilization with flexible intramedullary nailing. Between the ages of 6 and 11 years, the treatment of choice is fixation with flexible intramedullary nailing; in unstable fractures, possible alternatives are percutaneous submuscular bridge plating, as well as external fixators and lateral trochanteric nailing for patients older than 8 years. For those above the age of 12 years, the options are lateral trochanteric nailing, submuscular bridge plating, and external fixators, whereas flexible nailing can be used for patients above the age of 12 years with body weight below 50 kg.
Besides weigth and age other factors are important to determine the treatment, exposed fracture, polytrauma, floating knee and whether the fracture is metaphyseal either proximal or distal femur. Along with these variables, the configuration of the fracture line is fundamental in defining whether a fracture is stable or unstable.[5] These characteristics make the study of femur fractures in children stimulating and challenging.[6] Regarding the instability of the fracture, Kocher defined length-unstable fracture as those comminuted, spiral, or long oblique fractures with ≥2 cm shortening.[4]
The aim of this retrospective study was to evaluate the outcomes and complications of pediatric patients with unstable femur fractures treated with submuscular bridge plating in a tertiary referral trauma hospital.
Materials and Methods
We performed a retrospective analysis of all unstable femur fractures in patients under the age of 16 years treated at a tertiary hospital between January 2016 and December 2017.
The exclusion criteria were incomplete records, closed femoral physes, presence of osteometabolic or neuromuscular diseases, pathological fractures, and fractures that were either stable or treated by other methods.
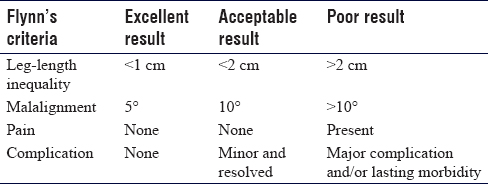
The collected data included age, mechanism of trauma, fracture type and location, date of surgery, follow-up duration, and associated lesions. The results were evaluated using the modified Flynn's criteria for treatment with intramedullary elastic osteosynthesis, which consists of evaluating the leg-length inequality, malalignment, presence of pain after consolidation, or postoperative complications.[7] Considering an excellent result, all criteria must be met. The Flynn's criteria are shown in [Table - 1].
We evaluated the time to implant removal and the occurrence of refracture and lack of consolidation.
Postoperative follow-up was performed at 2 and 6 weeks and at 3, 6, and 12 months; after 12 months, the removal of the plate is recommended.
Results
We retrieved data on 86 femur fractures in children and adolescents aged ≤16 years who were treated at our institution between January 2016 and December 2017. Of these, we excluded 1 fracture treated with Pavlik harness, 24 treated with early casting, 2 excessively distal fractures treated with crossed Kirschner wires, 30 treated with flexible intramedullary nails, 10 treated with external fixators, and 5 treated with locked intramedullary nailing.
Of the remaining 14 fractures treated with submuscular bridge plating, one patient was lost to follow-up after surgery and was excluded from the study.
Therefore, our final sample comprised 13 patients, including 12 boys and 1 girl. Seven fractures affected the right femur and six affected the left femur; two fractures were open and were classified as Gustilo Type IIIA, one resulting from a gunshot and the other from a motorcycle accident.
The mean age of the patients was 10 years and 2 months; the youngest patient was 7 years and the oldest was 13 years and 1 month.
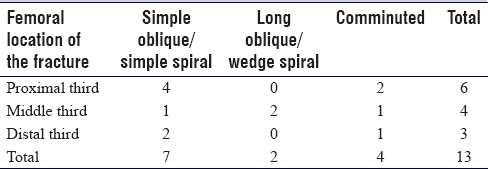
Regarding the mechanism of trauma, 4 fractures occurred due to automobile accidents, 5 due to falls (2 from the same level, 1 from a trampoline, 1 from a horse, and 1 from a skateboard), 2 from direct trauma, and 2 from gunshots [Table - 2].

Of the 13 diaphyseal fractures, 6 occurred in the proximal third of the femur, 4 in the middle third, and 3 in the distal third. As for the configuration of the fracture line, 7 were classified as long oblique or spiral fractures, 2 as spiral bending wedge fractures, and 4 as comminuted fractures; all the fractures were deemed unstable according to the Kocher's criteria [Table - 3].
After treatment, we observed 11 excellent, 2 satisfactory, and no poor results, according to the modified Flynn's criteria of intramedullary elastic osteosynthesis.[7]
All 13 patients were permitted 10% of weight-bearing in the immediate postoperative period, followed by progressive weight-bearing after the 6th week until full weight-bearing. All fractures were consolidated at the 12th week without any case of substantial malalignment or length inequality requiring correction.
We recommended the removal of the plate after the 1st postoperative year, and the removal was performed between the 1st and 2nd postoperative year. At the time of this study, eight patients had already undergone plate removal, and we observed no cases of refracture or considerable increase in technical difficulty due to the presence of bone callus because of the extended time until the removal.
Discussion
The protocol of the AAOS for the treatment of femur fractures in children is a very useful guide. However, in addition to age, other factors are important in choosing the appropriate therapeutic approach in this population, including the configuration of the fracture line, the region of the bone involved, presence or absence of instability, body weight, associated lesions, and mechanism of injury.
A fracture is considered unstable in length when it is comminuted, oblique, or spiral with a shortening >2 cm.[4] In most stable fractures, flexible intramedullary nailing has excellent results due to its elastic stability. However, application of this technique in children and adolescents with body weight above 50 kg or fractures defined as unstable may increase the risk of complications.[8],[9],[10]
In line with that, Moroz et al. indicated that weight >49 kg and age above 11 years are predictors of increased complications in fractures treated with flexible intramedullary nailing.[11] Sink et al.[12] reported that the adoption of the age of 11 years as a cutoff point was a better predictor of complications than weight alone; on the other hand, the adoption of both variables was not superior to age alone.
Sink et al. treated 39 patients with unstable femur fractures, of whom 15 were treated with flexible intramedullary nailing. The author observed 12 complications with this method, in addition to a need for reoperation in six patients to increase fixation stability.[13]
Narayanan evaluated the use of flexible nailing in the treatment of children between 2 years and 11 months and 15 years and 8 months and observed no increase in complications due to age, but associated the increased risk of loss of reduction with the use of nails of mismatched diameters for fixation and the presence of comminution >25% of the diaphyseal circumference.[14]
Li et al. compared fixation of subtrochanteric femur fractures with flexible nails versus open plating and submuscular plating and observed an increased risk of complications, especially in unstable fractures, with 4 times more complications and less excellent and satisfactory results with nailing compared with plating fixation.[15]
Therefore, for unstable or comminuted fractures, for patients older than 12 years and/or weight >50 kg, we do not recommend using flexible nailing. In these cases, other alternatives can be considered, including external fixators, fixation with submuscular bridge plating, and rigid intramedullary nailing with trochanteric insertion.
External fixation should be reserved for the treatment of open or severely comminuted femur fractures, due to their increased risk of loss of reduction, vicious consolidation, pseudoarthrosis, and refracture, in addition to the common occurrence of nail tract infection.[16],[17]
Another treatment option for patients older than 9 years is fracture stabilization with locked intramedullary nailing, provided that the medullary canal is >8 mm in its narrowest portion. Reports of complications described by Buford et al. with nails inserted through the piriformis fossa,[18] such as abnormal proximal femur growth, avascular necrosis of the femoral head, and limb-length discrepancy, stimulated the development of new models of rigid intramedullary nails with insertion through the lateral aspect of the greater trochanter, thus reducing the occurrence of complications that have been previously reported.[19]
Park et al. compared submuscular bridge plating and intramedullary nailing with lateral insertion through the greater trochanter in patients older than 12 years and observed similar results with both methods.[20] Plating and nailing are obvious alternatives for stabilization of unstable and metaphyseal femur fractures.
Fixation of femur fractures with percutaneous submuscular bridge plating has some advantages compared with the open technique, such as less injury to soft tissues, preservation of the fracture hematoma, and vascularization of bone fragments, which reduces the infection rates and minimizes the possibility of delayed consolidation due to compromised blood supply at the fracture site. As reported by Samora et al.,[21] and aligned with the current literature,[12],[22],[23],[24] this technique is associated with excellent consolidation, low complication rates, and early return to full weight-bearing. Similar results were found in our study, despite the small sample size.
Abbot et al.[25] compared open plating with submuscular bridge plating in 58 and 22 femur fractures, respectively. The authors observed one case of postoperative infection and five reoperations (one due to deep infection, three due to implant failure, and one due to a periprosthetic femur fracture) in fractures fixed with open plating, but no case of leg-length discrepancy more than 2 cm or clinically relevant rotational asymmetry.
Samora et al. and Sutphen et al. used a surgical technique with two incisions, one proximal and one distal,[21],[23] whereas Sink et al. proposed a distal incision to insert the plate in the submuscular plane, followed by percutaneous fixation of the screws proximal to the fracture.[26] In our patients, we performed two small incisions (proximal and distal) and when necessary, added intermediate percutaneous screws.
The use of 3.5-mm plates has been associated with loss of reduction or failure due to implant fracture.[27] We used in all our patients the 4.5-mm narrow Dynamic compression plate (DCP), whereas locked plates were not used in any of our cases. Because our patients had no comorbidities (osteopenia or bone fragility), the use of a conventional plate (DCP) was sufficient to guarantee the necessary stability for consolidation.
The use of a long plate, with 10–16 holes, is preferable to increase the work area by reducing the strain on the plate. At least three open screw holes should be left proximally and distally to the fracture, and ideally, six holes should be left open on each side of the fracture site [Figure - 1] and [Figure - 2].
 |
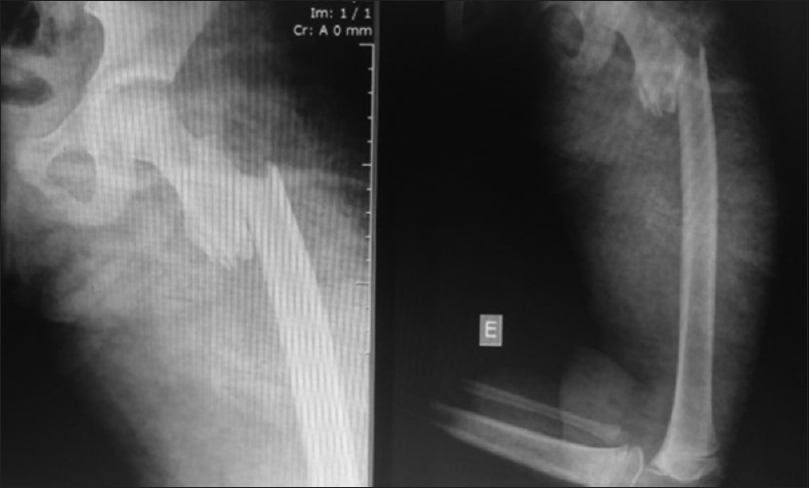
| Figure 1: A 10-year-old male, struck by a car |
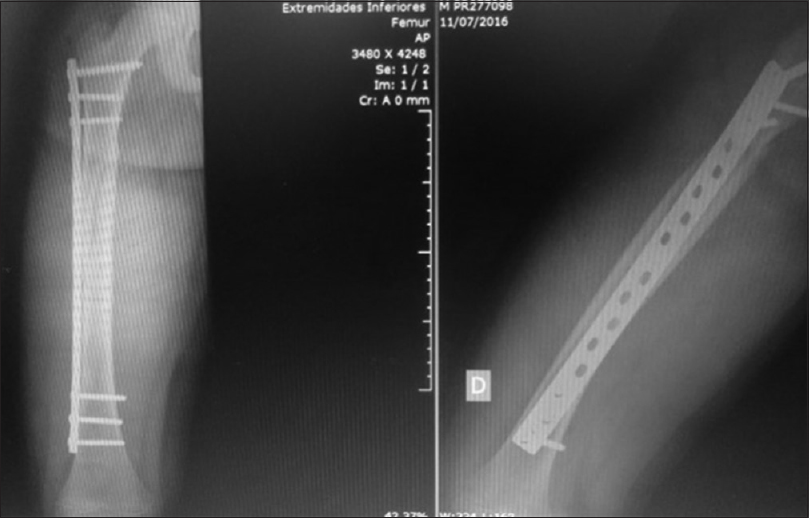 |
| Figure 2: 45 days after surgery |
With long plates, the plate should be molded to better adapt to the proximal and distal femoral anatomy [12],[26],[28],[29] [Figure - 3], [Figure - 4], [Figure - 5].
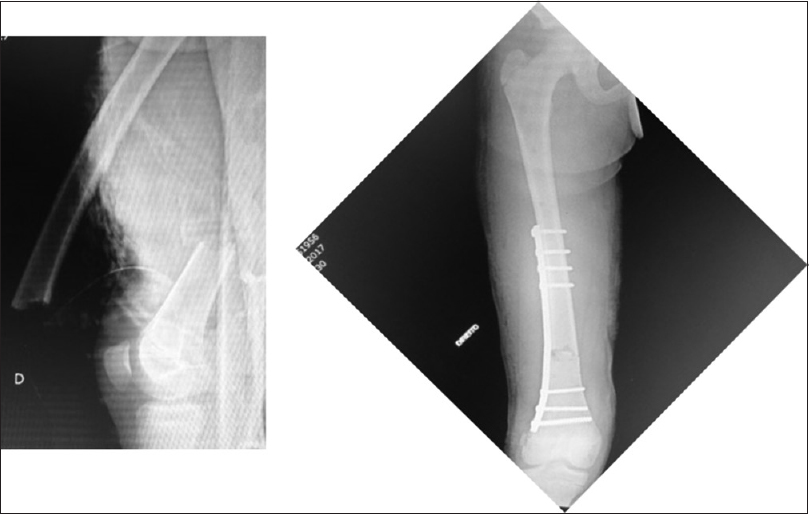 |
| Figure 3: A 12-year-old male, open fracture Gustilo II, distal molded submuscular plate |
 |
| Figure 4: A 11-year-old female, car accident |
 |
| Figure 5: Proximal molded submuscular plate postoperative |
The incision for the initial procedure is small and sufficient to insert the plate and screws, whereas the incision required for the removal of the plate is often larger than the one required for its insertion. This has been shown by Pate et al., who reported in 7 out of 22 cases a requirement for larger incisions for plate removal compared with the size of the incision required for insertion of the plates.[30]
Kelly et al. reported complications associated with plate retention in three patients who were lost to follow-up after consolidation.[31] Distal molding of the plate was used in all three cases to adapt the plate to the distal femoral metaphysis. The patients were readmitted at 3, 4, and 7 years after surgery and showed proximal migration of the plate due to distal femoral growth, bony overgrowth of the plate, femoral valgus deformity (15°, 10°, and 14°), and stress shielding at the distal end of the plate, as well as screw tip prominence in the medial thigh due to bone remodeling. All three patients had the plates removed, and one of the patients required two osteotomies to correct the femoral deformity.
Based on the literature and our personal experience, we consider the removal of the plate to be an absolute recommendation in cases with plates in the distal femur and preferably and whenever possible, as well as in plates in diaphyseal fractures. The removal is usually performed after the 1st postoperative year. In our series, we had no problems in performed this procedure. The limitations of this study are the short follow-up and the lack of comparison of our results with other alternative methods of fixation such as lateral entry intramedullary nails.
Conclusions
In the present study, submuscular bridge plating was a viable and safe alternative for the treatment of unstable femur fractures and fractures located in the distal and proximal femoral metaphyses in children and adolescents.
Ethical consideration
The study was approved by the Research Ethics Committee (CAAE: 76529717.7.0000.5225), according to Resolutions 196/96 and 251/97 of the Brazilian National Health Council.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Author's contribution
WV, JS, WG and FF conceived and designed the study, conducted research, provided research materials, and collected and organized data. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Sahlin Y. Occurrence of fractures in a defined population: A 1-year study. Injury 1990;21:158-60. [Google Scholar] |
| 2. | McCartney D, Hinton A, Heinrich SD. Operative stabilization of pediatric femur fractures. Orthop Clin North Am 1994;25:635-50. [Google Scholar] |
| 3. | Hinton RY, Lincoln A, Crockett MM, Sponseller P, Smith G. Fractures of the femoral shaft in children. Incidence, mechanisms, and sociodemographic risk factors. J Bone Joint Surg Am 1999;81:500-9. [Google Scholar] |
| 4. | Kocher MS, Sink EL, Blasier RD, Luhmann SJ, Mehlman CT, Scher DM, et al. Treatment of pediatric diaphyseal femur fractures. J Am Acad Orthop Surg 2009;17:718-25. [Google Scholar] |
| 5. | Soni J, Valeza WR, Faria FF. Femur shaft fractures in children. In: Hebert SK, Barros Filho TEP, Xavier R, Pardini A, editors. Ortopedia e Traumatologia: Princípios e Prática/[Organizadores]. 5th ed. Porto Alegre: Artmed; 2017. p. 32, 1651. [Google Scholar] |
| 6. | Heffernan MJ, Gordon JE, Sabatini CS, Keeler KA, Lehmann CL, O'Donnell JC, et al. Treatment of femur fractures in young children: A multicenter comparison of flexible intramedullary nails to spica casting in young children aged 2 to 6 years. J Pediatr Orthop 2015;35:126-9. [Google Scholar] |
| 7. | Flynn JM, Hresko T, Reynolds RA, Blasier RD, Davidson R, Kasser J. Titanium elastic nails for pediatric femur fractures: A multicenter study of early results with analysis of complications. J Pediatr Orthop 2001;21:4-8. [Google Scholar] |
| 8. | Garner MR, Bhat SB, Khujanazarov I, Flynn JM, Spiegel D. Fixation of length-stable femoral shaft fractures in heavier children: Flexible nails vs. rigid locked nails. J Pediatr Orthop 2011;31:11-6. [Google Scholar] |
| 9. | Leet AI, Pichard CP, Ain MC. Surgical treatment of femoral fractures in obese children: Does excessive body weight increase the rate of complications? J Bone Joint Surg Am 2005;87:2609-13. [Google Scholar] |
| 10. | Wall EJ, Jain V, Vora V, Mehlman CT, Crawford AH. Complications of titanium and stainless steel elastic nail fixation of pediatric femoral fractures. J Bone Joint Surg Am 2008;90:1305-13. [Google Scholar] |
| 11. | Moroz LA, Launay F, Kocher MS, Newton PO, Frick SL, Sponseller PD, et al. Titanium elastic nailing of fractures of the femur in children. Predictors of complications and poor outcome. J Bone Joint Surg Br 2006;88:1361-6. [Google Scholar] |
| 12. | Sink EL, Faro F, Polousky J, Flynn K, Gralla J. Decreased complications of pediatric femur fractures with a change in management. J Pediatr Orthop 2010;30:633-7. [Google Scholar] |
| 13. | Sink EL, Gralla J, Repine M. Complications of pediatric femur fractures treated with titanium elastic nails: A comparison of fracture types. J Pediatr Orthop 2005;25:577-80. [Google Scholar] |
| 14. | Narayanan UG, Hyman JE, Wainwright AM, Rang M, Alman BA. Complications of elastic stable intramedullary nail fixation of pediatric femoral fractures, and how to avoid them. J Pediatr Orthop 2004;24:363-9. [Google Scholar] |
| 15. | Li Y, Heyworth BE, Glotzbecker M, Seeley M, Suppan CA, Gagnier J, et al. Comparison of titanium elastic nail and plate fixation of pediatric subtrochanteric femur fractures. J Pediatr Orthop 2013;33:232-8. [Google Scholar] |
| 16. | Miner T, Carroll KL. Outcomes of external fixation of pediatric femoral shaft fractures. J Pediatr Orthop 2000;20:405-10. [Google Scholar] |
| 17. | Ramseier LE, Janicki JA, Weir S, Narayanan UG. Femoral fractures in adolescents: A comparison of four methods of fixation. J Bone Joint Surg Am 2010;92:1122-9. [Google Scholar] |
| 18. | Buford D Jr., Christensen K, Weatherall P. Intramedullary nailing of femoral fractures in adolescents. Clin Orthop Relat Res 1998;(350):85-9. [Google Scholar] |
| 19. | Gordon JE, Swenning TA, Burd TA, Szymanski DA, Schoenecker PL. Proximal femoral radiographic changes after lateral transtrochanteric intramedullary nail placement in children. J Bone Joint Surg Am 2003;85:1295-301. [Google Scholar] |
| 20. | Park KC, Oh CW, Byun YS, Oh JK, Lee HJ, Park KH, et al. Intramedullary nailing versus submuscular plating in adolescent femoral fracture. Injury 2012;43:870-5. [Google Scholar] |
| 21. | Samora WP, Guerriero M, Willis L, Klingele KE. Submuscular bridge plating for length-unstable, pediatric femur fractures. J Pediatr Orthop 2013;33:797-802. [Google Scholar] |
| 22. | Aǧuş H, Kalenderer O, Eryanilmaz G, Omeroǧlu H. Biological internal fixation of comminuted femur shaft fractures by bridge plating in children. J Pediatr Orthop 2003;23:184-9. [Google Scholar] |
| 23. | Sutphen SA, Mendoza JD, Mundy AC, Yang JG, Beebe AC, Samora WP 3rd, et al. Pediatric diaphyseal femur fractures: Submuscular plating compared with intramedullary nailing. Orthopedics 2016;39:353-8. [Google Scholar] |
| 24. | Sutphen SA, Beebe AC, Klingele KE. Bridge plating length-unstable pediatric femoral shaft fractures. J Pediatr Orthop 2016;36 Suppl 1:S29-34. [Google Scholar] |
| 25. | Abbott MD, Loder RT, Anglen JO. Comparison of submuscular and open plating of pediatric femur fractures: A retrospective review. J Pediatr Orthop 2013;33:519-23. [Google Scholar] |
| 26. | Sink EL, Hedequist D, Morgan SJ, Hresko T. Results and technique of unstable pediatric femoral fractures treated with submuscular bridge plating. J Pediatr Orthop 2006;26:177-81. [Google Scholar] |
| 27. | Kanlic EM, Anglen JO, Smith DG, Morgan SJ, Pesántez RF. Advantages of submuscular bridge plating for complex pediatric femur fractures. Clin Orthop Relat Res 2004;(426):244-51. [Google Scholar] |
| 28. | Rozbruch SR, Müller U, Gautier E, Ganz R. The evolution of femoral shaft plating technique. Clin Orthop Relat Res 1998;(354):195-208. [Google Scholar] |
| 29. | Apivatthakakul T, Chiewcharntanakit S. Minimally invasive plate osteosynthesis (MIPO) in the treatment of the femoral shaft fracture where intramedullary nailing is not indicated. Int Orthop 2009;33:1119-26. [Google Scholar] |
| 30. | Pate O, Hedequist D, Leong N, Hresko T. Implant removal after submuscular plating for pediatric femur fractures. J Pediatr Orthop 2009;29:709-12. [Google Scholar] |
| 31. | Kelly B, Heyworth B, Yen YM, Hedequist D. Adverse sequelae due to plate retention following submuscular plating for pediatric femur fractures. J Orthop Trauma 2013;27:726-9. [Google Scholar] |
Fulltext Views
4,407
PDF downloads
532





