Successful use of platelet-rich plasma as a regeneration technique for a non-healing diabetic leg ulcer with chronic osteomyelitis: A case report
*Corresponding author: Ziyad Alharbi, Plastic Surgery and Burn Unit, Dr. Soliman Fakeeh Hospital and Fakeeh College for Medical Sciences, Jeddah, Saudi Arabia. zialharbi@fcms.edu.sa
-
Received: ,
Accepted: ,
How to cite this article: Alrayes MM, Alghamdi AA, Waggas D, Alharbi Z. Successful use of platelet-rich plasma as a regeneration technique for a non-healing diabetic leg ulcer with chronic osteomyelitis: A case report. J Musculoskelet Surg Res. 2024;8:172-6. doi: 10.25259/JMSR_249_2023
Abstract
Chronic diabetic leg ulcers can be challenging to manage, particularly when osteomyelitis coexists resulting in serious or even life-threatening conditions if not managed appropriately. Such cases require very long periods of treatment with several debridements, antibiotic bead implants, skin grafts or even amputations in many unfortunate cases. Despite that, conventional management appears to be inadequate with poor outcomes and a higher relapse rate. We report a case of a 26-year-old type 1 diabetic female patient presented with a history of non-healing diabetic leg ulcer complicated by chronic osteomyelitis of the left leg. Several wound debridements were performed with the application of vacuum-assisted closure, and culture-guided antibiotics were given. However, only minimal improvements were observed. Eventually, the leg was labeled as an unsalvagable limb due to poor blood supply based on an ankle-brachial index. Platelet-rich plasma (PRP) was tried showing promising results and significant improvement as confirmed by a gallium scan, which showed evidence of osteomyelitis remission. Two months later, the patient improved significantly with the ulcer healed and the osteomyelitis resolved. Autologous PRP promotes wound healing by providing necessary growth factors, reducing inflammation, and showing bactericidal activity. All efforts must be taken to preserve any limb before labeling it non-salvageable. This case report aimed to draw attention to the method that can be implemented to manage non-healing diabetic leg ulcers complicated by chronic osteomyelitis.
Keywords
Chronic osteomyelitis
Diabetic foot
Non-healing ulcer
Platelet-rich plasma
INTRODUCTION
Chronic non-healing leg ulcers are a leading cause of morbidity and mortality for diabetic patients resulting in a considerable impact on the quality of life of the affected ones increasing the socioeconomic burden, as patients usually require longer durations of treatment and several operations. Despite all efforts, amputations are still frequently performed, as more than 85% of all lower extremity amputations are due to foot and leg ulcers with diabetes being reported as a major cause for non-traumatic amputations of the lower limbs.[1,2] Things can be more complicated when osteomyelitis coexists as a consequence of the disrupted immune response of diabetic patients. Almost 60% of diabetic foot and leg ulcers are complicated by infections that may reach deeper structures involving the bones. All diabetic foot and leg ulcer patients with clinical findings of infection should be suspected of potential bone involvement, especially those with chronic wounds or in case of ulcer recurrence.[1-3] Conventional therapies appear inadequate in some complicated cases with poor and higher recurrence rates. Autologous platelet-rich plasma (PRP) is an emerging solution that is worthy of much discussion; thus, here we report a case in which PRP was used successfully in treating a gangrenous diabetic leg ulcer that was complicated by osteomyelitis. The PRP is a safe and cost-effective method for treating such cases that deserve more attention and discussion. This paper highlights an approach for managing non-healing diabetic leg ulcers, especially those complicated by chronic osteomyelitis. The intention is to stimulate further research and exploration in this field fostering a deeper understanding of the proposed method’s efficacy and potential implications for the broader management of such complex medical conditions.
CASE REPORT
This is a 26-year-old female patient, who is a known case of type 1 diabetes mellitus that was diagnosed at the age of 11 years. She is also a known case of hypertension and end-stage renal disease. Her blood glucose was uncontrolled, as her blood glucose ranged from 300 to 400 mg/dL, and her hemoglobin A1c fluctuated between 9 and 11. She was referred to the plastic surgery unit with a long-standing history of gangrenous non-healing diabetic leg ulcer with exposed bone and chronic osteomyelitis of the distal one-third of the left tibia. Upon admission, the patient was febrile with black-colored necrotic tissues and exposed bone, which is a typical presentation of a complicated diabetic leg ulcer [Figure 1]. Poor peripheral blood perfusion was noted on examination, which was confirmed by Doppler. During the workup, tissue culture and wound swabs were taken before antibiotics initiation that showed heavy Candida albicans and Enterobacter cloacae growth. The patient was stabilized, and her blood glucose was strictly controlled. Culture-guided antibiotics were started, and several wound debridements were performed with vacuum-assisted closure (VAC) application, yet no significant improvement was noticed. Hence, the vascular surgeons deemed the foot as an unsalvageable limb citing an ankle-brachial index of 0.3. This diagnosis was subsequently validated through lower-limb angiography affirming the presence of peripheral chronic arterial disease with minimal collateral circulation.

- Upon admission, showing black-colored necrotic tissues with exposed bone.
The plastic surgery team formulated a plan to implement PRP therapy incorporating it concurrently with each debridement procedure. A 15 cc of blood was collected from the patient and centrifuged to extract the PRP [Figure 2]. Then, a total of 4 cc of PRP was injected into the boundaries of the wound at the left leg followed by the application of VAC as postoperative care [Figure 3]. After four days, the patient was retaken to the OR for another session of PRP and extensive debridement with drilling of a small area of the exposed tibia, about 1 cm × 1 cm, to enhance the blood supply from inside the bone to the outside followed by injection of the second dose of PRP at the wound edges [Figure 4]. A split-thickness graft was harvested from the thigh and applied to the defect with VAC. The gallium scan was repeated two months later. It showed scintigraphic evidence of response regarding the left medial malleolus osteomyelitis with almost complete resolution of the left distal tibia infection focus. The patient exhibited dramatic clinical improvement marked by complete healing of the ulcer and resolution of all signs of infection [Figure 5].
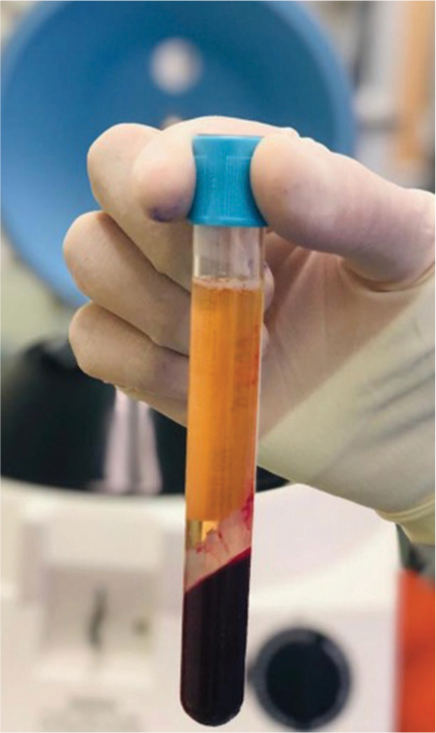
- The extracted platelet-rich plasma after centrifuging.
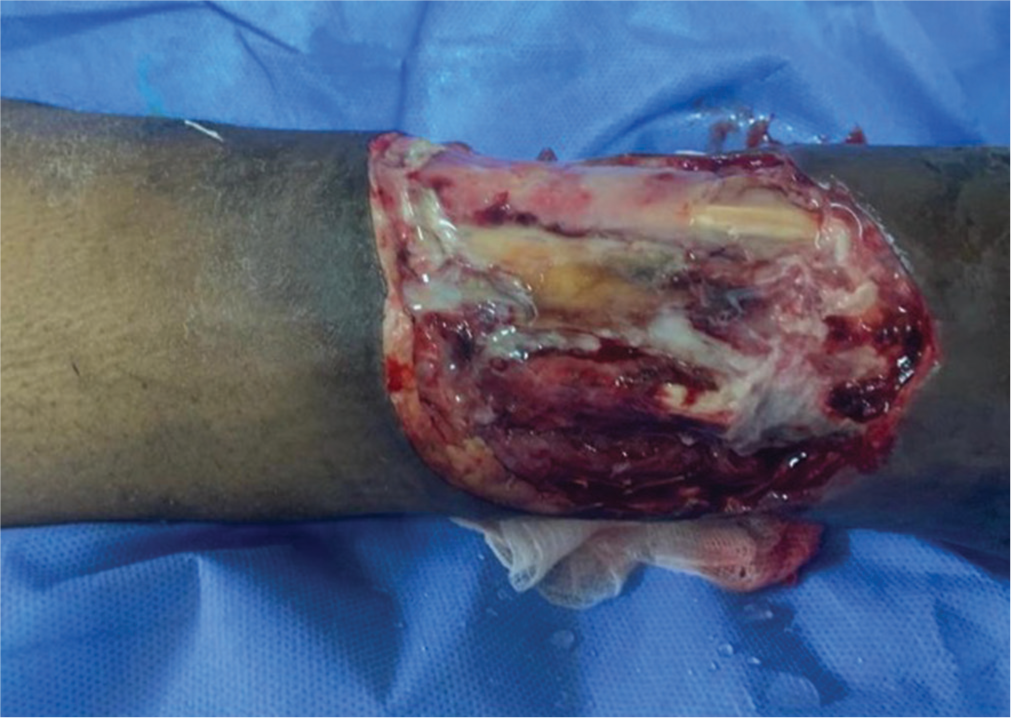
- Immediate post-operative image after an extensive debridement and the initiation of the first platelet-rich plasma session.

- Immediate Post-Op image after the second debridement after the initiation of the platelet-rich plasma (PRP) therapy, with bone drilling and second dose PRP.

- Showing the improvement of the wound after the debridements and two doses of platelet-rich plasma injections.
DISCUSSION
Disruption of glucose regulation results in a hyperglycemic state leading to abnormal activation of many metabolic pathways that subsequently lead to the development of peripheral vascular diseases and insufficiencies as well as neural damage manifested by ulceration in the lower extremity due to plantar pressures and foot deformity. Foot injury caused by trauma to the affected site goes unnoticed by the patient due to sensory loss. In addition, resistance to infection is another key modulator of the pathophysiological picture of diabetic foot ulcers, as diabetes increases the risk and severity of wound infection, which can be attributed to elevated glucose levels as well as granulocytic activity and chemotaxis deficiency.[3] In addition, there seems to be excessive inflammation, neovascularization impairment, reduced collagen production, an irregular extracellular matrix protein synthesis pattern, and decreased fibroblast proliferation.[4] The healing as well as non-healing nature of ulcers relies upon the wound microbial communities and the extent of their pathogenicity.[5] The mainstay of treatment depends on optimizing the patient’s condition by controlling blood sugar, avoiding any pressure on the wound, adequate infection control, and debridement of all non-viable necrotic tissues. Such measures seem to be inadequate for some complicated cases. Hence, new options include recombinant human growth factors and bioengineered skin substitutes, which might be beneficial, yet the high cost is a limiting factor.[6]
Autologous PRP is an emerging cost-effective method that is worthy of much discussion. The PRP facilitates the wound-healing process through seven growth factors that are present in it. They are platelet-derived growth factor (PDGF-αα, αβ, and αβ), fibroblast growth factor, vascular endothelial growth factor, epidermal growth factor, and transforming growth factor. These factors are essential in modulating mesenchymal cell recruitment as well as proliferation and synthesis of extracellular matrix during the healing process.[6] The PRP contributes to local debridement and exhibits bactericidal activities in chronic and infected wounds. The topical application of PRP in treating chronic infected wounds and osteomyelitis appeared effective in the published literature.[7,8] An interesting paper reports a successful case of treating chronic osteomyelitis in bilateral femurs that was resistant to prolonged antibiotic therapy and approximately 20 debridement procedures. Despite these extensive efforts, the sinus remained unhealed for over four years. Ultimately, applying PRP led to favorable outcomes when employed to address the persistent sinus marking a significant reported improvement.[8] In a prospective, randomized, controlled clinical trial, the efficacy of PRP gel compared to saline gel dressing in treating chronic diabetic foot ulcers was evaluated. The study enrolled 16 cases treated with PRP gel and 19 treated with saline gel dressing, all subjected to a rigorous follow-up protocol. Remarkably, 81.3% of wounds in the PRP gel group achieved healing, compared to only 42.1% in the saline gel group. Furthermore, it is noteworthy that PRP gel exhibited no adverse side effects throughout the study period.[9] Yet, another case study delves into the outcome of a patient grappling with chronic calcaneal osteomyelitis, methicillin-resistant Staphylococcus aureus-positive, coupled with a soft-tissue defect. Despite undergoing frequent debridement, vancomycin lavage, and adhering to regular dressing changes, the patient displayed no signs of improvement. However, after a series of three PRP sessions, the wound displayed a seamless healing process, yielding remarkable outcomes. Importantly, upon the latest reported follow-up, no infection recurrence was noted.[10] Our patient showed a significant response to the PRP injections with a substantial resolution of the osteomyelitis as well as healing of the ulcer. Even though it is unclear how PRP cures chronic osteomyelitis at the present time, the findings warrant more research.
Limitations
While this report highlights the potential efficacy of PRP in managing non-healing diabetic leg ulcers complicated by osteomyelitis, it is important to note that this is a case report. Further investigations employing methodologies such as case–control studies and randomized controlled trials are warranted to establish more robust conclusions. These comparative studies would contribute significantly to assessing the effectiveness of PRP over other existing treatment modalities.
CONCLUSION
Autologous PRP promotes the wound-healing process by providing necessary growth factors, reducing inflammation, and showing bactericidal activity. Although the exact mechanism by which PRP treats chronic osteomyelitis remains unclear, these promising results warrant further investigation and study. We treated a non-healing diabetic leg ulcer complicated by osteomyelitis successfully with PRP after the failure of the conventional therapies. We believe that PRP is a safe and cost-effective method for treating such cases.
AUTHORS’ CONTRIBUTIONS
MMA and AAA: Wrote and prepared the manuscript and the literature review. DW: Provided the clinical and laboratory data necessary for this case and provided an overall paper revision with substantial edits. ZA: The primary surgeon for this case. Provided overall supervision for writing the paper, provided the scientific content and the discussion. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
Institutional Review Board approval is not required.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published, and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Cellular and molecular basis of wound healing in diabetes. J Clin Invest. 2007;117:1219-22.
- [CrossRef] [PubMed] [Google Scholar]
- Lower extremity foot ulcers and amputations in diabetes In: Diabetes in America. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 1995. p. :409-28.
- [Google Scholar]
- Differences in cellular infiltrate and extracellular matrix of chronic diabetic and venous ulcers versus acute wounds. J Invest Dermatol. 1998;111:850-7.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetic foot ulcer--a review on pathophysiology, classification and microbial etiology. Diabetes Metab Syndr. 2015;9:192-9.
- [CrossRef] [PubMed] [Google Scholar]
- Quality assessment of platelet concentrates prepared by platelet rich plasma-platelet concentrate, buffy coat poor-platelet concentrate (BC-PC) and apheresis-PC methods. Asian J Transfus Sci. 2009;3:86-94.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet gel for healing cutaneous chronic wounds. Transfus Apher Sci. 2004;30:145-51.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of chronic femoral osteomyelitis with platelet-rich plasma (PRP): A case report. Transfus Apher Sci. 2008;38:167-73.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective, randomized, controlled trial of autologous platelet-rich plasma gel for the treatment of diabetic foot ulcers. Ostomy Wound Manage. 2006;52:68-70. 72, 74 passim
- [Google Scholar]
- Chronic calcaneal osteomyelitis associated with soft-tissue defect could be successfully treated with platelet-rich plasma: A case report. Int Wound J. 2013;10:105-9.
- [CrossRef] [PubMed] [Google Scholar]






