Translate this page into:
Surgical hip dislocation to treat chondroblastoma of the femoral head by transfoveal curettage and bone grafting
2 Department of Orthopaedic, Al-Rehab 2 Private Hospital; Department of Orthopaedic, Assiut University Hospital, Assiut, Egypt
3 Department of Orthopaedic, Al-Rehab 2 Private Hospital, Assiut, Egypt
Corresponding Author:
Ahmed A Khalifa
Department of Orthopaedic and Traumatology, Qena Faculty of Medicine and Its University Hospital, South Valley University, Kilo 6 Qena-Safaga Highway, Qena
Egypt
ahmed_adel0391@med.svu.edu.eg
| How to cite this article: Khalifa AA, Fadle AA, Alzohiry MA, Refai OA. Surgical hip dislocation to treat chondroblastoma of the femoral head by transfoveal curettage and bone grafting. J Musculoskelet Surg Res 2019;3:303-306 |
Abstract
Although chondroblastoma is rare, occasionally it may affect the femoral head with the dilemma of choosing the best surgical approach, which provides better access and avoids complications. We present a case of a 14-year-old female with chondroblastoma in the femoral head, which was treated through surgical hip dislocation by curettage and bone grafting through a transfoveal approach. At the latest follow-up at 24 months, there was no evidence of local recurrence or avascular necrosis on plain radiograph and the patient was pain-free. We believe that this approach is safe to treat such cases, but technically demanding.Introduction
Chondroblastomas represent 9% of benign bone tumors; proximal femur is the third commonplace after the proximal humerus and proximal tibia.[1]
Proximal femur lesions, which arise from the trochanteric area, are directly approached, but femoral head lesions represent a challenge to approach.[2]
Strong et al.[1] described three options to approach head lesions: (1) directly through a drill along the femoral neck, (2) “trapdoor” technique, or (3) dislocating the hip and a direct approach through the articular surface.
We report femoral head chondroblastoma case treated by transfoveal curettage and bone grafting using autologous bone from trochanteric osteotomy bed after surgically dislocating the hip.
Case Report
A 14-year-old female presented with 3 months of right hip pain and limping, along with no history of trauma, medication, or chronic diseases. Examination revealed a limitation of right hip motion (no internal rotation, external rotation 20°, and flexion to 90° were observed, but full range was observed when the patient was re-examined under anesthesia, indicating that the limitation was because of pain and not a true mechanical block). Plain radiographs (anteroposterior [AP] pelvis and lateral right hip) [Figure - 1]a and [Figure - 1]b showed an osteolytic lesion located in the upper lateral quadrant of the femoral head in the AP view and posterior to the central axis of the head in the lateral view. Computed tomography (CT) scan [Figure - 1]c and [Figure - 1]d confirmed the position of the lesion; however, the size appeared bigger and the lesion appeared well-circumscribed occupying half of the head with intact articular surface and no neck extension. A CT-guided biopsy (in a lateral decubitus position with the affected leg up, through the lateral cortex of the femur starting about an inch distal to the tip of the greater trochanter with a needle angled superomedially up through the femoral neck till the lesion is reached [3]) revealed benign featuring chondroblastoma. The option of conservatively treating the lesion using radiofrequency ablation (as mentioned in the literature [4]) was discussed with a radiology consultant, who recommended against this line of treatment based on the location and the size of the lesion. The decision was made to treat this lesion by local excision and bone grafting through hip surgical dislocation.
 |
| Figure 1: (a and b) Plain radiograph (anteroposterior, lateral); (c and d) computed tomography scan, well-defined osteolytic lesion |
Surgical technique
Surgery was done under general anesthesia. Exposure of the femoral head was achieved as described by Ganz et al. utilizing a surgical hip dislocation.[5] The approach was through a lateral longitudinal skin incision centered on the greater trochanter. The deep dissection was through the Gibson interval between the gluteus maximus and medius muscles. A trochanteric flip osteotomy [Figure - 2]a was performed and retracted anteriorly to expose the capsule [Figure - 2]b, which was opened by a Z-shaped incision; the hip was dislocated after transection of the ligamentum teres [Figure - 2]c.
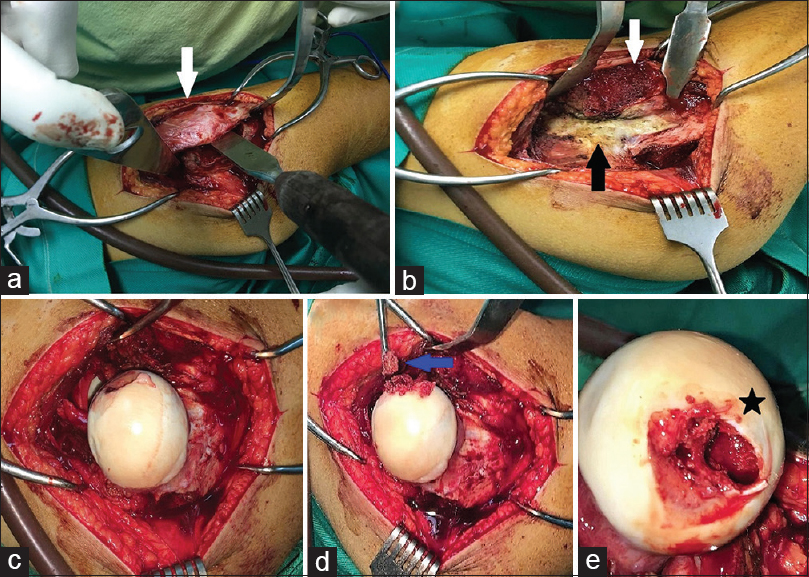 |
| Figure 2: Surgical steps. (a) Trochanteric osteotomy (white arrow), (b) capsule in view (black arrow), (c) dislocated hip, ligamentum teres is debrided, (d) transfoveal approach (blue arrow) lesion curettage, (e) cyst size (black star) |
Ligamentum teres insertion debridement was done to expose the fovea; after gentle probing of the head cartilage to confirm the location of the lesion, the decision was made to approach the lesion transfoveal. Using a 15-mm blade, the fovea was opened avoiding cartilage damage. The lesion was removed by curettage [Figure - 2]d, high-speed burring, and hydrogen peroxide, the size of the lesion was re-estimated, and it was about 1.5 cm × 2 cm [Figure - 2]e. With a new set of instruments to avoid contamination, a cancellous bone block as well as a morselized cancellous bone autograft was harvested from the trochanteric flip osteotomy site [Figure - 3]a and was impacted inside the lesion [Figure - 3]b. The fovea was closed by graft impacting to act as a bone plug. Intact vascularity was confirmed by drilling a hole in the intact part of the head, the joint was reduced, and the capsule was closed using interrupted sutures. The trochanteric fragment was reduced and fixed with two 3.5-mm cortical screws.
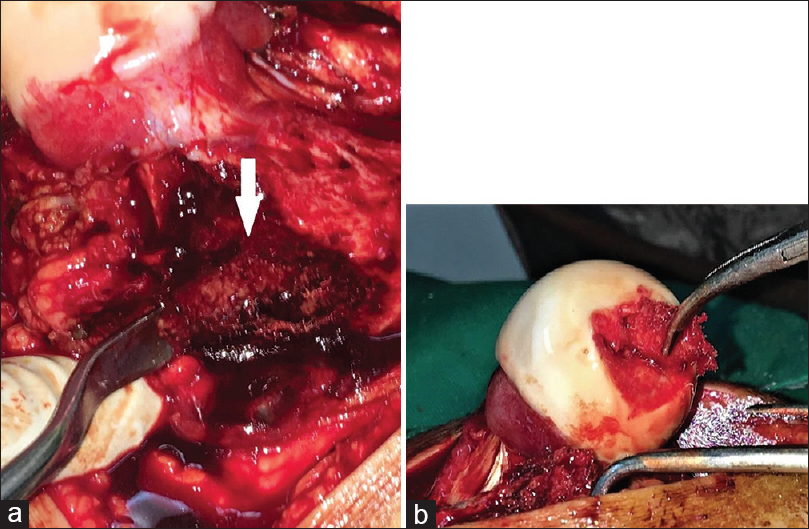 |
| Figure 3: Grafting of the lesion. (a) Graft harvesting, trochanteric osteotomy bed (white arrow), (b) graft impaction |
Postoperative management and follow-up
Toe-touch weight-bearing was allowed, and hip flexion was limited to 70° for 6 weeks. AP and lateral radiographs of the hip were obtained immediate postoperative [Figure - 4]a, at 6 weeks, and at the last follow-up, which was at 24 months [Figure - 4]b, at which the patient was pain-free, and the radiograph showed consolidation of the lesion with no signs of recurrence or collapse (the patient was asked to have hip magnetic resonance imaging at the last follow-up, but her parents refused).
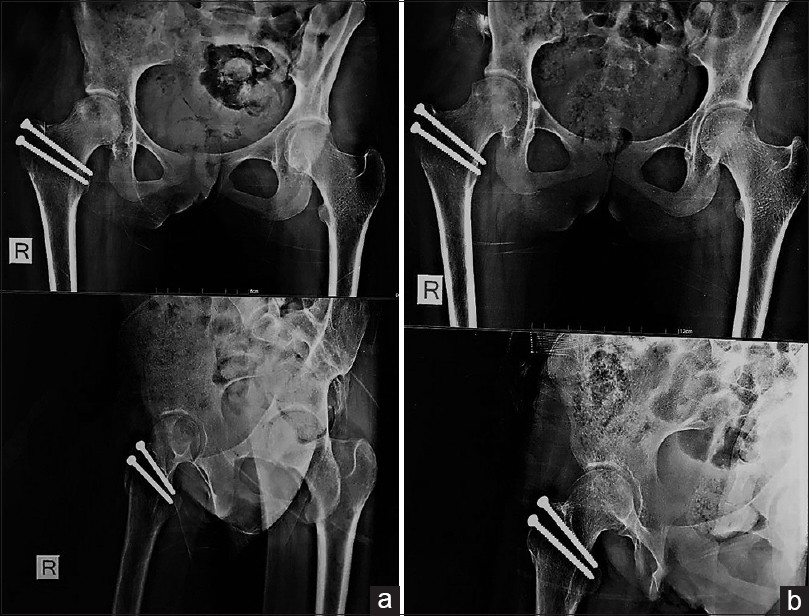 |
| Figure 4: Postoperative radiographs. (a) Immediate postoperative, (b) 24 months follow-up |
Discussion
In treating chondroblastoma, there is no role for chemotherapy, and radiotherapy is contraindicated; as it may induce malignant transformation,[1] radiofrequency ablation is a joint-sparing conservative line which may be utilized in some selected cases.[6] The surgical line of treatment mainly in young patients is by curettage, with or without bone graft or cement filling.[7]
Apart from dislocating the hip to attack these lesions, another two approaches were described. First is a direct approach through a drill in the femoral neck,[8] with the drawback of violating the cortical bone of the femoral neck, which has an increased risk of fracture; further, this approach necessitates a long intraosseous track, with difficulty in controlling head lesion curettage.[9]
Second is a trapdoor technique, which was described by Mont et al.[10] to treat femoral head avascular necrosis. Iwai et al.[11] modified this technique, where they used it in combination with surgical hip dislocation in treating femoral head chondroblastomas by curettage and grafting giving satisfactory results after almost 5 years.
Strong et al.[1] reported the use of two different approaches in 10 patients. Five patients were treated with a direct approach through the femoral neck in whom they had no recurrence and achieved full function. The other group of five patients who were treated using a femoral neck canal had two local recurrences.
To fully access the lesion, we utilized surgical hip dislocation described by Ganz et al.[5] which involved an anterior dislocation of the hip after a trochanteric flip osteotomy, which had been shown in many reports to be safer than other approaches from avascular necrosis endpoint.[12]
We approached the lesion through a transfoveal approach as was described by Rüdiger et al.[9] where they treated a giant cell tumor of the femoral head with excellent outcome after 2 years. However, they used another incision to harvest iliac bone graft, which was not the case in our technique where we harvested the graft from the trochanteric osteotomy bed and avoided iliac graft site morbidity.
Xu et al.[2] used a Smith–Petersen approach to anteriorly dislocate the hip and gained access to chondroblastomas of the femoral head through the transfoveal approach in 14 patients; they reported one case of avascular necrosis and one case with heterotopic ossifications.
To decrease the incidence of complications, bone grafting helps reducing the incidence of avascular necrosis and collapse.[2] Furthermore, joint manipulation should be performed gently to avoid vascular flow disruption. When repairing the capsule, the sutures should be loose to reduce subsequent contracture.
Conclusion
This approach is a safe, effective way of treating femoral head chondroblastoma, avoiding iliac graft donor-site morbidity. Careful dislocation and relocation of the hip as well as cautious postoperative physical rehabilitation to avoid early collapse or avascular necrosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Author's contribution
AAK generated the concept, literature search, manuscript preparation, and reviewing; AAF contributed by defining the intellectual content and literature search; MAA contributed by manuscript preparation and edition; OAR contributed by data acquisition, manuscript editing, and reviewing. OAR was the surgeon for this case report and AAF and MAA were the assistants during the surgery. All authors contributed equally to the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Strong DP, Grimer RJ, Carter SR, Tillman RM, Abudu A. Chondroblastoma of the femoral head: Management and outcome. Int Orthop 2010;34:413-7. [Google Scholar] |
| 2. | Xu H, Niu X, Li Y, Binitie OT, Letson GD, Cheong D. What are the results using the modified trapdoor procedure to treat chondroblastoma of the femoral head? Clin Orthop Relat Res 2014;472:3462-7. [Google Scholar] |
| 3. | Liu PT, Valadez SD, Chivers FS, Roberts CC, Beauchamp CP. Anatomically based guidelines for core needle biopsy of bone tumors: Implications for limb-sparing surgery. Radiographics 2007;27:189-205. [Google Scholar] |
| 4. | Petsas T, Megas P, Papathanassiou Z. Radiofrequency ablation of two femoral head chondroblastomas. Eur J Radiol 2007;63:63-7. [Google Scholar] |
| 5. | Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 2001;83:1119-24. [Google Scholar] |
| 6. | Erickson JK, Rosenthal DI, Zaleske DJ, Gebhardt MC, Cates JM. Primary treatment of chondroblastoma with percutaneous radio-frequency heat ablation: Report of three cases. Radiology 2001;221:463-8. [Google Scholar] |
| 7. | Suneja R, Grimer RJ, Belthur M, Jeys L, Carter SR, Tillman RM, et al. Chondroblastoma of bone: Long-term results and functional outcome after intralesional curettage. J Bone Joint Surg Br 2005;87:974-8. [Google Scholar] |
| 8. | Davidson D. CORR insights®: What are the results using the modified trapdoor procedure to treat chondroblastoma of the femoral head? Clin Orthop Relat Res 2014;472:3468-70. [Google Scholar] |
| 9. | Rüdiger HA, Piasecki K, Becce F, Cherix S. Trans-foveal approach for curettage and bone grafting of a giant cell tumour in the femoral head. Hip Int 2016;26:612-4. [Google Scholar] |
| 10. | Mont MA, Einhorn TA, Sponseller PD, Hungerford DS. The trapdoor procedure using autogenous cortical and cancellous bone grafts for osteonecrosis of the femoral head. J Bone Joint Surg Br 1998;80:56-62. [Google Scholar] |
| 11. | Iwai T, Abe S, Miki Y, Tokizaki T, Matsuda K, Wakimoto N, et al. Atrapdoor procedure for chondroblastoma of the femoral head: A case report. Arch Orthop Trauma Surg 2008;128:763-7. [Google Scholar] |
| 12. | Sink EL, Beaulé PE, Sucato D, Kim YJ, Millis MB, Dayton M, et al. Multicenter study of complications following surgical dislocation of the hip. J Bone Joint Surg Am 2011;93:1132-6. [Google Scholar] |
Fulltext Views
2,062
PDF downloads
486





