Translate this page into:
Synovial chondromatosis of the elbow: A rare case with severe joint destruction treated with arthrodesis
*Corresponding author: Ilham S. W. Antono, Department of Orthopaedics and Traumatology, Dr. Cipto Mangunkusumo Hospital, Faculty of Medicine Universitas Indonesia, Jakarta, Indonesia. ilham.suryow@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Cahayadi SD, Antono IS, Pratama WS. Synovial chondromatosis of the elbow: A rare case with severe joint destruction treated with arthrodesis. J Musculoskelet Surg Res. doi: 10.25259/JMSR_94_2025
Abstract
Synovial chondromatosis is a rare benign tumor that generally affects large joints such as the knee and hip. Elbow joint involvement is very rare, especially with severe joint destruction. Diagnosis is often delayed because the symptoms are non-specific and resemble other conditions. A 59-year-old woman presented with a progressive lump in the right elbow that had appeared for the past year and was accompanied by tingling, numbness, pain, and limited movement to only 90° flexion. Radiographs showed radioulnar joint dislocation and multiple opacities resembling loose bodies. Magnetic resonance imaging showed active synovitis, bursitis, and cartilage nodules (hypointense on T1 and hyperintense on T2) accompanied by synovial thickening and loss of articular cartilage. Core biopsy showed synovial tissue without a typical tumor pattern. After tumor excision, elbow arthrodesis with internal fixation in a 90° flexion position was performed. The patient showed significant clinical improvement without complications at 1-month post-operative evaluation. This case demonstrates that synovial chondromatosis of the elbow can cause severe joint destruction and dysfunction if not treated properly. Management by excision and arthrodesis can be the definitive choice in cases with extensive joint damage. Early detection, appropriate therapy choices, and long-term monitoring are important to prevent recurrence or malignant transformation.
Keywords
Arthrodesis
Bone neoplasm
Chondromatosis
Locoregional neoplasm recurrences
Osteochondromas
Osteochondromatosis
INTRODUCTION
Synovial chondromatosis is a non-malignant, tumor-like abnormality that affects the cartilage in soft tissues, particularly the synovium of joints. This condition can result in the development of nodules or loose masses composed of cartilage.[1] Most cases occur in males aged 30–50 with a 1:1.8 ratio. Synovial chondromatosis often manifests unilaterally, with unusual bilateral occurrences. The major joints, notably the knee, are mostly affected, although it may involve any joint. It commonly affects the knees, hips, and elbows.[1,2] Furthermore, synovial chondromatosis has been observed both intra- and extra-articularly, including locations such as the extensor digitorum longus tendon, even when it is rarely documented.[2]
The most commonly affected parts by synovial chondromatosis are the knee and hip, while the involvement of the elbow is quite rare. Other than that, the majority of the elbow cases do not exhibit severe joint destruction, leading to the seldom documented case of severe synovial involvement leading to secondary degenerative changes and joint instability of the elbow.[3]
According to the findings of Bell et al., trauma has been identified as a potential risk factor for the development of primary or secondary synovial chondropathy.[4] The loose entities within the joint compartment lacked autonomous proliferative activity. Three distinct stages of disease progression have been identified. The initial stage, or stage I, is characterized by synovial hyperplasia, hyperemia, and the metaplasia of synovial connective tissue into cartilage, while the formation of loose bodies has not yet occurred. The subsequent stage II is marked by active synovium. Inflammation is commonly linked to the presence of loose bodies. Stage III involves the reduction of synovitis, characterized by the presence of either a single or several loose bodies. The nourishment provided by synovial fluid facilitates the growth of loose bodies, enabling them to develop in a localized manner. When untreated in its early stages, it has the potential to cause permanent damage to cartilage and joints and may progress into synovial chondrosarcoma.[5] The majority of loose bodies consist of cartilage and either central bone or calcified components. In addition, there are cases when loose bodies solely consist of cartilage without bone involvement. Consequently, conventional radiographs may not be sufficient for detection, necessitating the use of more sensitive diagnostic techniques such as computed tomography (CT) or magnetic resonance imaging (MRI). The existing therapeutic interventions include pharmacological agents and surgical procedures. In the initial stage, the utilization of non-steroidal anti-inflammatory drugs may be employed as a means to alleviate pain symptoms. In the context of stages II and III, it is commonly advised to undertake the removal of the afflicted synovial membrane or the elimination of any loose bodies. The surgeon chooses between open and arthroscopic surgical resection based on the specific problem, with other options beyond synovectomy being treatments such as elbow arthroplasty or arthrodesis.[5]
This report includes a comprehensive case study examining the occurrence of synovial chondromatosis in the elbow joint of a 59-year-old female patient. This report aimed to describe the severe clinical presentation and provide a detailed clinical description of the severe deterioration linked to synovial chondromatosis.
CASE REPORT
A 59-year-old female patient presented to the hospital with a complaint of a progressively growing lump on her right elbow. She noticed the lump a year ago but ignored it as it was asymptomatic. However, over the past 5 months, she began experiencing tingling and numbness in the fingers of her right hand. The pain during movement progressively worsens, forcing her to switch most of her activities to her left hand. Her elbow was unstable, limited to 90° flexion.
Upon physical examination, a swelling approximately the size of a golf ball was discovered on the medial side of the right cubital region, with no signs of inflammation.
Plain radiographs of the right elbow (anteroposterior and lateral) showed dislocation of the radioulnar joint with articular deformity, multiple irregular radiopaque opacities resembling loose bodies, and osteophytes indicating advanced degenerative changes. Synovial hypertrophy with osteophyte formation could indicate extensive cartilage loss. However, there were no typical signs of a tumor mass [Figure 1]. MRI showed active synovitis and bursitis with a hypointense mass on T1 and hyperintense on T2, consistent with cartilaginous lesions. Loose bodies were visible, accompanied by synovial thickening and loss of articular cartilage. These images support the diagnosis of synovial chondromatosis complicated by severe joint destruction [Figure 2]. Subsequent core biopsy examination showed synovial tissue with no typical tumor pattern. The diagnosis of synovial chondromatosis was then established.

- (a) Pre-operative anteroposterior view and (b) lateral view of the right elbow showing dislocation of the radioulnar joint, articular deformity, multiple radiopaque loose bodies, and osteophyte formation consistent with advanced degenerative changes due to synovial chondromatosis.

- Pre-operative magnetic resonance imaging of the right elbow. (a) Coronal T1-weighted image showing hypointense lesions. (b) Coronal T2-weighted image showing hyperintense loose bodies. (c) Sagittal view showing synovial thickening and joint effusion. (d) Axial view showing articular cartilage loss, all indicating advanced joint destruction due to synovial chondromatosis.
We conducted an excision of the tumor followed by arthrodesis. We approached the elbow with a posterior approach until the tumor was completely exposed. Intraoperative assessment found severe joint destruction and cartilage loss, making joint preservation impossible. With prior chronic worsening pain and limited range of motion, arthrodesis would be an ideal option; another option, synovectomy alone, would not restore function. Elbow arthrodesis was then conducted in 90° fixed flexion. Plate and screw fixation was then conducted [Figure 3]. The excised specimen consisted of multiple irregular cartilaginous nodules consistent with synovial chondromatosis as shown in the gross specimen [Figure 4]. Postoperatively, the patient showed no complications or signs of infection or wound dehiscence. We did a 1-month follow-up, and in the last visit, the patient showed resolved symptoms with no pain. However, the patient still feels a slight sensory deficit with numbness in the hand. The patient has no motor deficit on the distal part of the elbow; a long-term follow-up is still necessary to determine the full prognosis of functional outcomes and monitor for recurrence or malignant transformation.
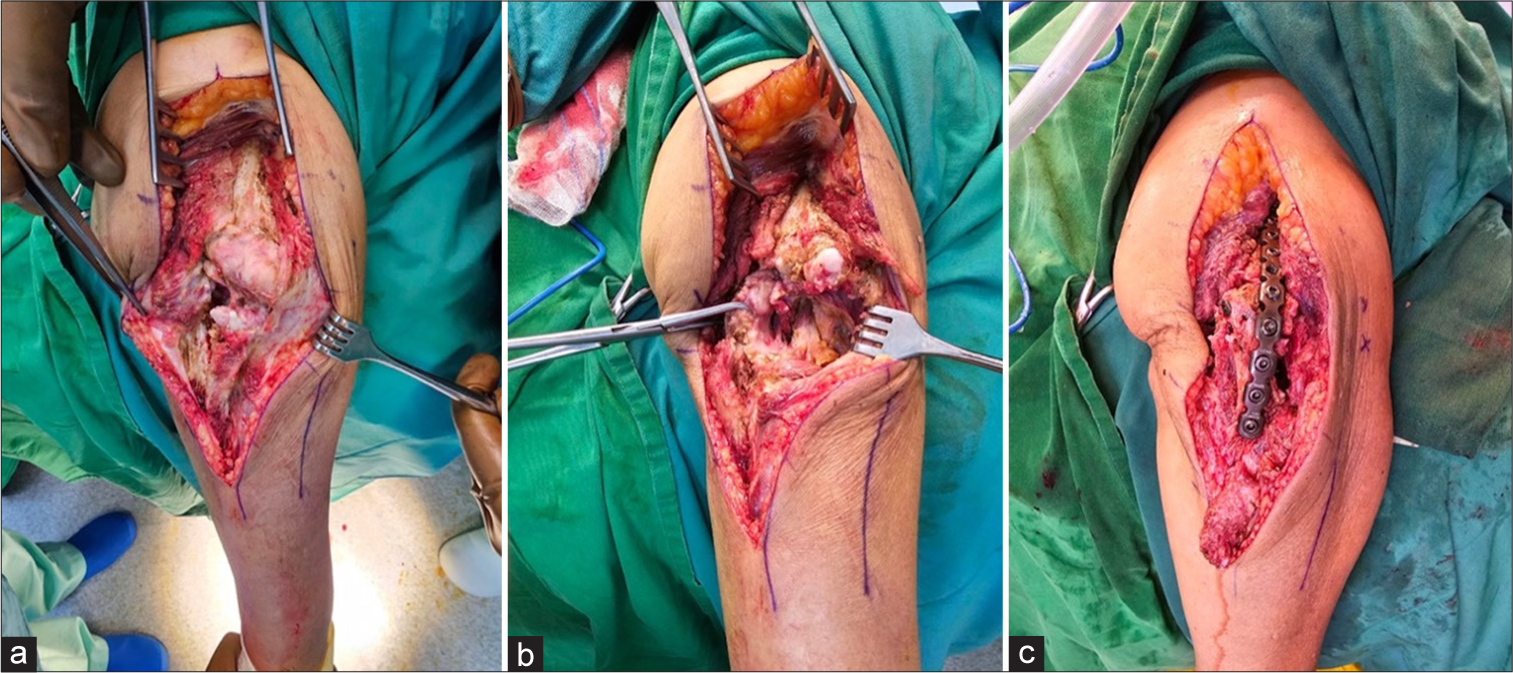
- (a) Intraoperative photograph during arthrodesis procedure showing the posterior approach to the right elbow. The joint is exposed with visible loose cartilaginous bodies and synovial proliferation consistent with advanced synovial chondromatosis. (b) Intraoperative photograph during arthrodesis procedure of the right elbow following complete excision of loose bodies and hypertrophic synovium. The joint space is clearly visible and prepared for arthrodesis following tumor clearance in synovial chondromatosis. (c) Final intraoperative image demonstrating completed elbow arthrodesis using plate and screw fixation after tumor excision for advanced synovial chondromatosis. The joint was fused in 90° of flexion to provide structural stability and pain relief.

- Gross specimen of the excised tumor from the right elbow, showing multiple irregular cartilaginous nodules of varying sizes consistent with loose bodies in synovial chondromatosis. A sterile surgical ruler is included for scale.
DISCUSSION
Synovial chondromatosis lacks definitive diagnostic criteria due to its rarity. Symptoms are non-specific, mimicking other conditions. In severe cases, we can find severe joint destruction, dislocations, and severe instability, just like what we see in this case. In the majority of cases, symptoms manifest as discomfort and/or limited joint mobility.[6] One of the primary indications is the incapacity to attain complete extension, which may afterward be accompanied by joint locking. The trait of rigidity is not readily apparent.[1,6]
In this case, we described a 59-year-old woman who initially reported a lump on her elbow, along with symptoms of numbness and tingling. There were no reports of hand pain, edema, or other related concerns. Numerous scholarly works explore the phenomenon of nerve compression, specifically focusing on the ulnar nerve and its consequential impact on the sensory and motor capabilities of the extremities located distally. Clinicians encounter heightened challenges in differentiating this condition from other diseases, such as synovial chondrosarcoma, pigmented villonodular synovitis, osteochondritis dissecans, calcifying aponeurotic fibroma, elbow tuberculosis, hydroxyapatite deposition, and rheumatoid arthritis, due to the presence of nonspecific symptoms and signs.[7]
Although commonly described as a non-malignant neoplasm, the individual under consideration has a clinical presentation of a small lump situated on the elbow. Nevertheless, it is important to highlight that during the next 5 months, the lump demonstrated significant and accelerated expansion, thus necessitating additional investigation. The individual provided an account of feeling the first sensations of tingling and instability in the elbow region. MRI showed radioulnar dislocation and synovitis. In addition, the examination indicated the existence of synovitis and bursitis, accompanied by the presence of loose bodies. There was no visible evidence of the presence of a tumor mass. It is recommended that the utilization of MRI for each patient should be contemplated, contingent upon the patient’s financial capacity to procure such services. The efficacy of MRI in visualizing the degenerative changes related to synovial chondromatosis has been well-established. MRI thoroughly evaluates the lesion’s scope, making it a valuable tool in this context. Furthermore, MRI facilitates detecting and characterizing the potential engagement of adjacent soft tissues, bone marrow, and neurovascular systems. The data it provides to the practitioner holds significant importance in establishing the suitable treatment approach, whether it involves conservative measures or surgical interventions, for patients affected by diverse illnesses. Pathology confirms the diagnosis.[1,8]
Due to rapid growth causing severe joint destruction, cartilage loss, and chronic worsening pain with limited range of motion, synovectomy alone would not restore function. Therefore, excision with arthrodesis was performed. There was apprehension regarding the potential consequences of the tumor’s exponential growth on tissue damage.[1,7]
Treatment options may vary depending on the underlying cause. The minimally invasive arthroscopy procedure involves removing loose bodies and synovectomy (removing the affected synovial tissue) for synovial chondromatosis. Arthroscopy has the advantages of low morbidity, early rehabilitation, and higher patient satisfaction. However, patients must be informed that recurrence is possible. In cases where arthroscopy is not feasible or if there are extensive loose bodies, open surgery may be performed to remove the loose bodies and perform a synovectomy [Figure 3]. This approach may be more invasive than arthroscopy, but it can effectively treat synovial chondromatosis. Arthrodesis ensured a clear margin and disease evaluation by providing complete excision of the affected synovial tissue and loose bodies, minimizing the risk of recurrence, while providing structural stability to the damaged elbow joint.
Following tumor resection in cases with extensive joint destruction, such as advanced synovial chondromatosis, several elbow reconstruction options can be considered based on the patient’s age, degree of tissue damage, and functional needs.[9,10] Total elbow arthroplasty may be an option in elderly patients with low activity, providing a functional range of motion and pain relief.[9,11] For younger patients or those with significant bone damage, interpositional arthroplasty or modular tumor endoprosthesis may be considered, although they carry a higher risk of complications.[10,11] In these cases, arthrodesis is the definitive approach because the joint damage is extensive and stability cannot be maintained.[10,11] Arthrodesis provides good structural stability, relieves pain, and reduces the risk of recurrence because all pathological synovial tissue is completely removed.[11]
Bell et al.[4] conducted a study wherein they recorded a case of synovial chondropathy of the temporomandibular joint. The decision to abstain from the surgical excision of the tumor was motivated by concerns regarding the potential adverse effects on underlying tissues. Nevertheless, the continuous observation conducted for 18 months did not exhibit any signs or indications of the reappearance of the tumor. There exists debate surrounding the potential influence of prolonged trauma experienced during surgical operations as a potential risk factor for relapse. Based on the findings of Aydin et al.,[12] authors who have reported comparable cases to Bell, it was determined that the presence of metaplastic activity during treatment was recognized as the key factor contributing to the probability of recurrence. The uncommon documentation of malignant transformation into chondrosarcoma has also been reported. Evans conducted a study in which a comprehensive analysis was performed on a sample of 78 instances of primary synovial chondromatosis. This investigation revealed that out of these cases, a total of 5 exhibited a progression toward chondrosarcoma.[13] The occurrence of malignant transformation in four cases was shown in a study undertaken by McCarthy et al.,[14] which analyzed a total of 155 occurrences of primary synovial chondromatosis. Hence, it is crucial to commence timely surgical intervention and provide regular post-operative surveillance to improve the overall prognosis of the illness.
CONCLUSION
Severe elbow synovial chondromatosis may require excision and arthrodesis, and surgeons should monitor for recurrence or transformation into malignancy.
Authors’ contributions:
SDC: Contributed to concepts, design, and literature search. ISWA: Responsible for design, literature search, and manuscript preparation. WSP: Contributed to the manuscript preparation, editing, and review. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published, and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Conflicts of interest:
There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Arthroscopic treatment of synovial osteochondromatosis of the elbow. Case report and literature review. Rev Bras Ortop (English Ed). 2015;50:607-12.
- [CrossRef] [Google Scholar]
- tenosynovial (extra-articular) chondromatosis of the extensor digitorum longus tendon and synovial chondromatosis of the ankle: Treated by extensor digitorum longus tendoscopy and ankle arthroscopy. Foot Ankle Spec. 2015;8:422-5.
- [CrossRef] [PubMed] [Google Scholar]
- Ankle synovial chondromatosis: Clinical, radiological, and surgical findings: A case report. Radiol Case Rep. 2024;19:3227-30.
- [CrossRef] [PubMed] [Google Scholar]
- Conservative surgical management of synovial chondromatosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:592-3.
- [CrossRef] [PubMed] [Google Scholar]
- Arthroscopic management of elbow synovial chondromatosis. Medicine (Baltimore). 2018;97:e12402.
- [CrossRef] [PubMed] [Google Scholar]
- Synovial osteochondromatosis of the elbow. J Bone Joint Surg Br. 2002;84:961-6.
- [CrossRef] [PubMed] [Google Scholar]
- Extremely rare synovial chondrosarcoma arising from the elbow joint: Case report and review of the literature. J Shoulder Elbow Surg. 2012;21:e7-11.
- [CrossRef] [PubMed] [Google Scholar]
- Synovial chondromatosis of the elbow in a child. Indian J Orthop. 2011;45:181-4.
- [CrossRef] [PubMed] [Google Scholar]
- Total elbow arthroplasty for primary and metastatic tumor. Orthop Traumatol Surg Res. 2016;102:459-65.
- [CrossRef] [PubMed] [Google Scholar]
- Joint replacement surgery for elbow tumours: A systematic review of outcomes. Shoulder Elbow. 2021;13:656-70.
- [CrossRef] [PubMed] [Google Scholar]
- Bone tumours around the elbow: A rare entity. EFORT Open Rev. 2019;4:133-42.
- [CrossRef] [PubMed] [Google Scholar]
- A case of synovial chondromatosis of the TMJ: Treatment based on stage of the disease. J Craniofac Surg. 2002;13:670-5.
- [CrossRef] [PubMed] [Google Scholar]
- Synovial chondrosarcoma arising in synovial chondromatosis. Sarcoma. 2014;2014:647939.
- [CrossRef] [PubMed] [Google Scholar]
- Primary synovial chondromatosis: A reassessment of malignant potential in 155 cases. Skeletal Radiol. 2016;45:755-62.
- [CrossRef] [PubMed] [Google Scholar]







