Translate this page into:
Systematic review and meta-analysis of the efficacy of hip distraction in Legg-Calve-Perthes disease
*Corresponding author: Ghadeer A Alsager, Department of Orthopedics, King Saud Medical City, Riyadh, Saudi Arabia. ghadeer.alsagr@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Alsager GA, Aljafar F, Alrabai HM. Systematic review and meta-analysis of the efficacy of hip distraction in Legg-Calve-Perthes disease. J Musculoskelet Surg Res. 2025;9:193-201. doi: 10.25259/JMSR_497_2024
Abstract
Legg-Calve-Perthes disease (LCPD) is a common disease, with multiple treatment options, including hip distraction (HD), which is considered a relatively promising new modality. The main objective of the present study is to perform a systematic review and meta-analysis of the literature to determine if HD is a beneficial method for treating LCPD. A systematic review of existing literature was conducted. After screening for eligibility, clinical and radiographic outcomes were extracted. A meta-analysis of the extracted data was undertaken. All English full-text reports studying HD in LCPD patients aged 18 or less between 1990 and 2021 were considered eligible. A total of 65 full-text articles were assessed for eligibility. Clinical and radiographic outcomes were extracted. A meta-analysis of the extracted data was undertaken. Seventeen studies were included, with 259 patients diagnosed with LCPD. There were significant changes in abduction [mean = 20.97°, 95% confidence interval (CI): 17.39, 24.55, I2 = 0%], flexion (mean = 24.48°, 95% CI: 19.47, 29.50, I2 = 20%), and internal rotation (mean = 12.24°, 95% CI: 8.06, 20.42, I2 = 71%). The mean difference between pre-operative and post-operative pain scores was significant (P < 0.05) (mean 2.86, 95% CI: 2.5, 3.21). In terms of radiological parameters, the epiphyseal index indicated significant increases after distraction among the included studies (mean = 4.58, 95% CI: 0.05, 9.11, I2 = 89%). The current literature supports using HD among patients with LCPD, as it showed satisfactory outcomes in hip range of motion, pain, and radiographic parameters. Further focused research is warranted in this field to demonstrate the efficacy of HD.
Keywords
Efficacy
External fixators
Hip distraction
Late-onset
Legg-Calve-Perthes disease
Outcome
INTRODUCTION
Legg-Calve-Perthes disease (LCPD) is a common pathology of the adolescent hip.[1] It is characterized by idiopathic avascular necrosis of the femoral head, leading to femoral head morphological changes and subsequent articular incongruency.[1,2] The end result seems to be related to the degree of damage to the femoral head.[3] Many authors advocated preventing or lessening the collapse of the femoral head during the critical period of active disease.[1,2,4] The underlying bone infarction leads to remarkable absorption of bone stock out of the femoral head, resulting in a feeble femoral head that is unable to withstand hip-crossing forces.[3] Weight-bearing is considered one of the major forces that can deform the femoral head.[1]
There are multiple options for conservative and operative treatment modalities. Most treatment strategies aim to keep the femoral head as spherical as possible until the remodeling stage is reached. These treatment modalities include bed rest, offloading brace, limb traction, osteotomies of the hip, and shelf procedures.[1-5] Hip distraction (HD) is considered a relatively new modality for the treatment of LCPD. An external fixator creates a distraction through the joint to reduce the stress on the articulating surfaces and protect against collapse.[4,6,7]
HD has been studied and reported in the present literature. Some reports have demonstrated significant improvement in hip range of motion (ROM), pain, along with the degree of superior and lateral subluxation, and its efficiency in postponing the need for total hip replacement and preventing further femoral collapse.[8-10] A study compared outcomes of Salter acetabuloplasty with HD for the treatment of LCPD and noticed that both methods led to similar radiological outcomes, apart from a higher morbidity rate related to external fixators in the HD group.[11] Another study estimated the rate of pin-tract infection in HD as high as 76%, with more prevalence on the acetabular side.[12]
The question about the effectiveness of HD in LCPD is not clearly answered in the current literature. The authors believe that available evidence should be synthesized and analyzed in a systematic review and meta-analysis. The main objective of the present study is to systematically review the evidence related to the efficacy of HD in the management of LCPD.
MATERIALS AND METHODS
This study followed the preferred reporting items for systematic reviews and meta-analysis statements.[13]
Eligibility criteria
All cohorts included in our study met the following criteria: (1) English articles that presented data concerning, (2) HD arthroplasty in (3) LCPD, (4) in patients aged 18 or less, (5) comparing clinical outcomes before and after treatment (6) from 1990 to 2021, (7) with full-text articles available. The following studies were excluded: Review articles, expert opinions, biomechanical, animal, and cadaveric studies. We conducted citation chaining of included references on an ongoing basis. We manually screened reference lists of the included studies to search for additional publications. Forward citation chaining was performed using Google Scholar.
Identification of studies
A comprehensive literature search by two reviewers independently was performed using the following search terms: Hip, hip joint, Perthes, LCPD, distraction arthroplasty, joint distraction, articulated distraction, arthrodiastasis, hinged distraction, arthrodistraction, and joint distraction arthroplasty. Searches were tailored using the Boolean operators “AND/OR.” The search was limited to humans in the following electronic databases (MEDLINE [Ovid], EMBASE [Ovid], Web of Science [ISI Web of Knowledge], and Cochrane (Clinical Trial Register). Reference lists of reviews and retrieved articles were assessed for further studies. Preliminary screening was conducted by reading the titles and abstracts of the retrieved literature. The selected literature was further filtered by reading the full text.
Data extraction
After the initial assessment for inclusion, two authors independently extracted the data from the included articles. Following initial data extraction, the exclusion criteria were reassessed. Disagreement was resolved by group discussion and consulting a third author, where differences remained. The data extracted include the number of patients, gender, age, device used, mean age at operation, mean follow-up, number of patients reached skeletal maturity, frame time, hip ROM, complications, LCPD classifications, radiological parameters, and epiphyseal index. The data were extracted for both pre- and post-distraction periods to compare the changes in these outcomes after HD.
Statistical analysis
Effect estimates of the intervention were synthesized using a random-effect meta-analysis with inverse-variance weighting. A random-effect model was applied as it is more conservative than a fixed-effect method for assessing the heterogeneity of included studies and confidence intervals of the effect sizes. The meta-analysis was separately applied to each outcome for which the number of eligible studies was two or more. The meta-analysis combined the results of the studies reporting the number of patients, point estimates (mean, risk ratios), and distribution variables [standard deviation (SD), interquartile ranges, confidence intervals (CIs), etc.]. When these statistical estimates were not directly reported in a study, we calculated them using the reported data of each patient’s outcomes. For such calculations, we used R version 3.3.0.[14] The analysis was conducted using Review Manager (RevMan) version 5.4.1.[15] Funnel plots were used for visually inspecting potential publication bias and were generated for outcome variables with pooled data from more than ten studies. Differences between groups were assessed using the chi-square statistic for categorical data and the Z-test for two proportions. A P-value greater than 0.05 was considered statistically insignificant. Kendall’s Tau (Tau) tool was used to determine the degree of association between two ordinal variables. The I2 statistic was used to quantify heterogeneity, which represents the percentage of variation among studies caused by heterogeneity rather than random chance. The degree of heterogeneity was categorized into the following categories: <30% (low), 30%-49% (moderate), 50%-79% (substantial), and >80% (considerable).
RESULTS
The search through the database yielded a total of 339 studies. Duplicates were removed, and articles were screened on titles and abstracts; 65 full-text articles were assessed for eligibility. Of these, 48 articles were excluded [Figure 1], 17 articles were selected for the systematic review, and 16 for the meta-analysis. This review included 259 patients diagnosed with LCPD, who underwent HD. Characteristics of the included population are shown in Table 1.
| Study | Study group | Intervention | Outcome | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | M | F | Device | Mean age at operation (year) | Follow-up (year) | Reached skeletal maturity | Frame time (months) | ||||||||
| Laklouk and Hosny[5] | 19 | 15 | 4 | Hinged Ex-Fix | 9.3 | 7.2 | 19 | 5 | |||||||
| Amer and Khanfour[8] | 30 | 21 | 9 | Non-hinged Ex-Fix | 9.7 | 3.6 | NA | 5 | |||||||
| Cañadell et al.[9] | 3 | 1 | 2 | Hinged Ex-Fix | 15.3 | 3.2 | NA | 3 | |||||||
| Maxwell et al.[10] | 15 | 11 | 4 | Hinged Ex-Fix | 10.4 | 3.2 | NA | 4 | |||||||
| Volpon[11] | 26 | NA | NA | Hinged Ex-Fix | 8.3 | 7.3 | 19 | 4.4 | |||||||
| Hosny et al.[12] | 29 | 22 | 7 | Non-hinged Ex-Fix | NA | 7.5 | 21 | 5 | |||||||
| Kucukkaya et al.[16] | 8 | NA | NA | Hinged Ex-Fix | 7.8 | 2.8 | 0 | 3.5 | |||||||
| Kocaoglu et al.[17] | 11 | 8 | 3 | Non-hinged Ex-Fix | 7.4 | 3.0 | 11 | 3.3 | |||||||
| Sabharwal and Van Why[26] | 1 | 1 | 0 | Hinged Ex-Fix | 8.0 | 2.0 | 0 | 3.2 | |||||||
| Segev et al.[24] | 10 | 8 | 2 | Hinged Ex-Fix | 12.3 | 5.7 | 10 | 5 | |||||||
| Aly and Amin[18] | 23 | 17 | 6 | Hinged Ex-Fix | 6.8 | 6.3 | NA | 4 | |||||||
| Sudesh et al.[19] | 14 | 11 | 3 | Hinged Ex-Fix | 11.3 | 3.2 | NA | 1 | |||||||
| Singh et al.[20] | 12 | 8 | 4 | Hinged Ex-Fix | 9.8 | 2.7 | NA | 4 | |||||||
| Kim[21] | 7 | 5 | 2 | Hinged Ex-Fix | 9.1 | 6.7 | 7 | 3 | |||||||
| Luzo et al.[25] | 18 | 13 | 5 | Hinged Ex-Fix | 8.5 | NA | NA | 3 | |||||||
| Abo El-Fadl[22] | 20 | 11 | 9 | Non-hinged Ex-Fix | 9.8 | 2.2 | NA | 5 | |||||||
| Aguado-Maestro et al.[23] | 13 | 9 | 4 | Hinged Ex-Fix | 11.9 | 1.8 | 5 | 4 | |||||||
F: Female, M: Male, NA: Not available, Ex-Fix: External fixator

- Flow of the preferred reporting items for systematic reviews and meta-analyses followed.
Study characteristics
The 17 studies were spread over nine countries. Egypt had the highest number of studies, five; Brazil, India, Spain, and Turkey had two studies each, while Palestine, Korea, Netherlands, and the US had one study each. The study design was prospective cohort (n = 11 or 64.7%), clinical trial (n = 3) with ambispective, retrospective cohort, and case report (n = 1 each). The condition of patients was either LCPD (64.7%) or late-onset LCPD (35.3%). The total number of participants was 259, made up of 161 males (62.2%) and 64 females (24.7%), while two studies[11,16] did not report the sex of their participants, which counted for 34 patients (13.1%). The mean age of participants was 9.4 years. The mean follow-up time was 4.75 years. The most reported complication was pin-tract infection.
Clinical outcomes
Infection rate
The infection rate after HD was reported in 14 studies.[5,8-12,16-23] Of these 14 studies, four studies did not describe the exact number of patients who developed infections. The average infection rate on the pin-site or hip across the included studies was 31.6%, ranging between 0% and 75.9% (SD = 25.9%; 11 studies).[8,10,11,16,24,25] All 14 studies reported the number of patients who had to remove the device due to infection. The average rate of infection that required premature removal of the device was 2.4% (SD = 3.7), with a range between 0% and 11.1% among the 14 studies. The infection rates and the severity may differ between hip and femur. As some studies did not report the site of infection,[23] the comparison of the average infection rates between the hip and femur was not available in this review, highlighting the need to report the infection rates for each site in future studies.
Three studies used hydroxyapatite-coated (HA) pins. However, the Infection rate was not reported thoroughly to withdraw a valid conclusion[10,23,26]; Maxwell et al.[10] reported infection to be among the most common complications; however, the exact number was not mentioned. Sabharwal and Van Why[26] did not report the infection rate, and Aguado-Maestro et al.[23] reported one case to be complicated by infection. All other included studies did not specify the coating of the pins.
ROM
Results of the meta-analysis for the estimated changes in the ROM (degrees) in the post-distraction period compared to the pre-distraction period are shown in Figure 2. The pooled estimates showed significant changes for abduction (mean = 20.97°, 95% CI: 17.39, 24.55, I2 = 0%), flexion (mean = 24.48°, 95% CI: 19.47, 29.50, I2 = 20%), and internal rotation (mean = 12.24°, 95% CI: 8.06, 20.42, I2 = 71%). The meta-analysis results did not show significant changes in adduction, extension, and external rotation after the distraction. The I2 statistic was used to quantify heterogeneity, representing the percentage of variation among studies caused by heterogeneity rather than random chance. The degree of heterogeneity was categorized into the following categories: <30% (low), 30–49% (moderate), 50–79% (substantial), and >80% (considerable).[27] In our study, I2 ranged from 0% to 96%. Considerable heterogeneity was observed among studies included for the ROM for extension (I2 = 96%) and external rotation (I2 = 90%). Substantial heterogeneity was found for adduction (I2 = 79%) and internal rotation (I2 = 71%), while the heterogeneity for flexion was low (I2 = 20%). No significant heterogeneity was found for abduction (I2 = 0%).

- (a) Forest plot of abduction pre- and post-distraction. (b) Forest plot of flexion pre- and post-distraction. (c) Forest plot of internal rotation pre- and post-distraction. SD: Standard deviation, IV: Inverse variance, df: Degrees of freedom, CI: Confidence interval, Tau: Kendall’s Tau is a tool to determine degree of association between two ordinal variables, Chi: Chi-square test to determine association of two nominal variables, P: Probability value, I2: Percentage of variation among studies caused by heterogeneity, Z: Standard score.
Pain
Of the 11 studies that reported events of pain pre- and postoperative, six showed a statistically significant difference in pain events in log odds. The pooled log odds ratio was 3.28 (95% CI: 2.31, 4.25) with P < 0.001. Four studies[8,9,21,23] reported pre-and post-operative pain scores showed that the mean difference was significant (P < 0.05), (mean 2.86, 95% CI: 2.5, 3.21) and was significant (P < 0.001) [Figure 3].
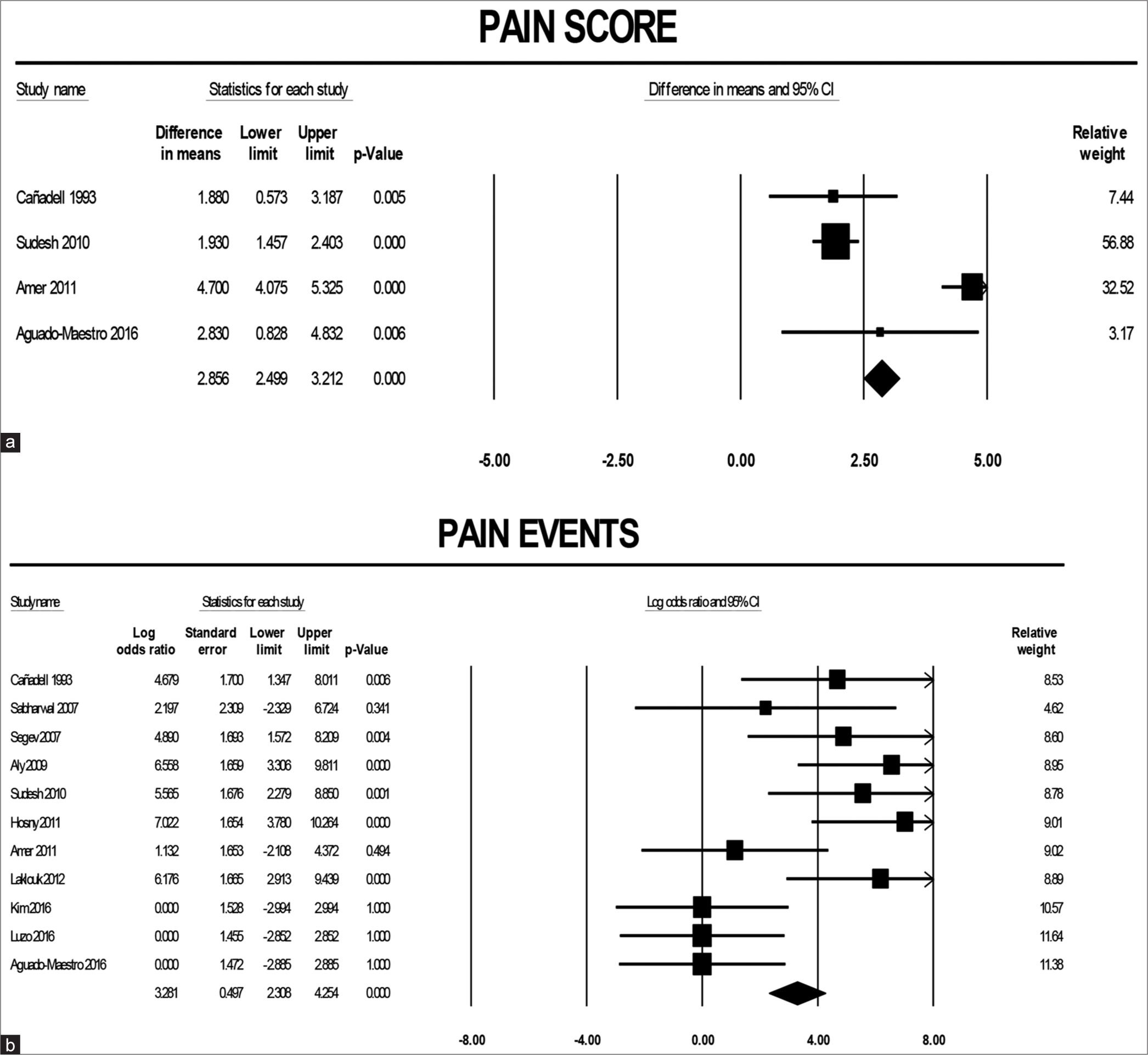
- (a) Sensitivity analysis of pre-and post-operative pain score. (b) Pooled log odds of pre- and post-operative pain event. CI: Confidence interval.
Radiological outcomes
Radiographic classifications of LCPD
We found that Herring, Catterall, and Stulberg classifications were used in the 16 included studies. The Herring classes were used in 10 studies and authors mostly used Herring classes to identify target patients for the treatment (i.e., distraction). However, only one study[20] compared the changes in Herring classes after the treatment for each patient. As a result, a quantitative combination of the changes in Herring classes after the treatment was unavailable for the included studies, which warrants future studies for summarizing the evidence. Similarly, most included studies used the Catterall and Stulberg classifications to target patients or assess the radiographic outcomes after the treatment. As each classification system has not been reported for both pre- and post-distraction periods among these studies, a meta-analysis using statistical estimates such as Kappa coefficients assessing the agreements of the classes after the treatment was not available for the included studies.
Other radiographic outcomes
Radiographic outcomes other than the disease classifications were reported in a few studies. For example, the epiphyseal quotient at the last follow-up was reported in two studies.[5,24] Sharp transverse acetabular inclination was used in two studies[5,24] but only for the pre-distraction period.
Epiphyseal index
Among the included studies, three were combined in the meta-analysis for the epiphyseal index.[21,22,24] The effect estimates from 4 study groups were synthesized as one study[22] had two intervention groups. Results of the pooled average change in the epiphyseal index indicated significant increases after distraction (mean = 4.58, 95% CI: 0.05, 9.11, I2 = 89%) [Figure 4]. The I2 (89%) indicated considerable heterogeneity among the included studies for epiphyseal index.

- Forest plot of epiphyseal index comparison between pre- and post-distraction. SD: Standard deviation, IV: Inverse variance, df: Degrees of freedom, CI: Confidence interval, Tau: Kendall’s Tau is a tool to determine degree of association between two ordinal variables, Chi: Chi-square test to determine association of two nominal variables, P: Probability value, I2: Percentage of variation among studies caused by heterogeneity, Z: Standard score.
Publication bias
Potential publication bias was inspected using funnel plots. The funnel plots for the ROMs for abduction, adduction, flexion, extension, internal rotation, and external rotation indicated no publication bias after sensitive analysis. Furthermore, the funnel plot for the epiphyseal index did not indicate publication bias. However, cautious interpretation is advised due to the few studies included [Figure 5].

- Funnel plots for publication bias.
Risk of bias
The risk of bias was assessed using the Office of Health Assessment and Translation tool.[28] Among the 17 studies, the overall risk of bias in eleven studies (64.7%) was probably high.[5,8,9,16,17,18,21-24,26] The risk of bias in the rest of the six studies was probably low [Appendix 1].[10-12,19,20,25]
DISCUSSION
To date, there is no consensus on the management protocol for patients with LCPD.[1-4] Management options can be summarized mainly into three primary categories: Symptomatic treatment, nonsurgical containment, and surgical containment.[1,2] The main aim is to prevent or minimize the occurrence of deformity of the femur head and incongruence of the affected hip, thus maintaining hip ROM.[1,5] Surgical options include femoral varus osteotomy, Salter osteotomy, lateral shelf acetabuloplasty, and recently HD.[1,5]
This meta-analysis’s results support HD’s effectiveness in treating LCPD patients. The positive changes observed in ROM and epiphyseal index were significantly superior post-operatively compared to pre-operative values. HD is proven to be effective in reducing pain as well. Based on pre-operative and post-operative visual analog pain scores, the mean difference improved significantly in four studies.[8,9,19,23] A further analysis comparing reported pain events preoperatively and post-operatively showed fewer pain events using the log odds (P < 0.01) after the operation. The negative finding observed was the occurrence of infection, with a percentage of 31.6%. However, most of these were pin-tract infections, which rarely led to removing the external device or some of its elements.
HD acts by decreasing both weight-bearing forces and muscle forces acting upon the hip joint by means of bridging the external fixator. This external fixator works by distracting the pelvis from the proximal femur, allowing unloading of the joint by separation of the articular surfaces and bearing some of the forces coming from weight-bearing and muscles. Some external fixator devices are provided with hinges, allowing for ROM continuity. The overall decrease of the pressure acting upon the joint eventually allows for joint cartilage healing and regeneration by restoring normal vascularity and nourishment. This procedure could help halt or postpone progression toward more invasive surgical interventions such as arthrodesis or total hip replacement.[6,7]
When compared to conventional surgical methods, the advantages of HD include its easy technique, less surgical morbidity, short hospitalization period, provision of sustained hip containment, and safeguarding sphericity of the femoral head. Furthermore, allowing controlled hip motion can be considered an additional advantage of hinged external fixators. HD with an external fixator can bridge the zone of pathology around the hip, leaving some room for potential future intervention, if needed, by leaving the surgical field intact.[5,11]
Limitations
Poor reporting of some relevant findings in the included studies limited the data synthesis to more useful meta-analyses. The lack of control groups among the included studies restricted the analysis capability of making more meaningful comparisons. Heterogeneity was relatively present between studies for which the random-effect model was adopted in meta-analysis. However, heterogeneity of the quality of the included studies could not be fully addressed. Published studies were not consecutive in terms of publication date and had differences in the level of evidence, making it difficult to draw scientifically significant conclusions. The most critical limitation of this meta-analysis was the number of included studies.
CONCLUSION
HD showed favorable outcomes in treating LCPD patients regarding hip mobility, pain, and radiographic parameters. As with other external fixation devices, recurrent pin-tract infection was common and rarely led to device removal or re-operation. More comparative high-quality studies are required to determine the superiority of HD over other treatment modalities.
Authors’ contributions
All authors contributed to the study’s conception and design. GA and HA: Material preparation, data collection, and analysis. GA and FA: The first draft of the manuscript. All authors commented on previous versions of the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required, as there are no patients in this study.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Conflicts of interest
There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Legg-calvé-perthes disease overview. Orphanet J Rare Dis. 2022;17:125.
- [CrossRef] [PubMed] [Google Scholar]
- Legg calve perthes disease In: Stat pearls. Treasure Island, FL: Stat Pearls Publishing; 2022.
- [Google Scholar]
- Arthrodiastasis in the management of perthes disease: A systematic review. J Pediatr Orthop B. 2020;29:550-5.
- [CrossRef] [PubMed] [Google Scholar]
- Hinged distraction of the hip joint in the treatment of perthes disease: Evaluation at skeletal maturity. J Pediatr Orthop B. 2012;21:386-93.
- [CrossRef] [PubMed] [Google Scholar]
- Joint distraction in treatment of osteoarthritis (II): Effects on cartilage in a canine model. Osteoarthritis Cartilage. 2000;8:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- The biological effect of continuous passive motion on the healing of full-thickness defects in articular cartilage. An experimental investigation in the rabbit. J Bone Joint Surg Am. 1980;62:1232-51.
- [CrossRef] [PubMed] [Google Scholar]
- Arthrodiastasis for late onset perthes' disease using a simple frame and limited soft tissue release: Early results. Acta Orthop Belg. 2011;77:472-9.
- [Google Scholar]
- Arthrodiastasis for stiff hips in young patients. Int Orthop. 1993;17:254-8.
- [CrossRef] [PubMed] [Google Scholar]
- Arthrodiastasis in perthes' disease. Preliminary results. J Bone Joint Surg Br. 2004;86:244-50.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison between innominate osteotomy and arthrodistraction as a primary treatment for legg-calvéperthes disease: A prospective controlled trial. Int Orthop. 2012;36:1899-905.
- [CrossRef] [PubMed] [Google Scholar]
- Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097.
- [CrossRef] [PubMed] [Google Scholar]
- R: A language and environment for statistical computing. 2020. Vienna, Austria: R Foundation for Statistical Computing; Available from: https://www.R-project.org [Last accessed on 2022 Sep 09]
- [Google Scholar]
- Review manager (rev man) version 5.4.1. 2020. The Cochrane Collaboration. Available from: https://training.cochrane.org/online-learning/core-software/revman/revman-5-download [Last accessed on 2024 Nov 03]
- [Google Scholar]
- Avascular necrosis of the femoral head in childhood: The results of treatment with articulated distraction method. J Pediatr Orthop. 2000;20:722-8.
- [CrossRef] [PubMed] [Google Scholar]
- Ilizarov fixator for treatment of legg-calvé-perthes disease. J Pediatr Orthop B. 1999;8:276-81.
- [CrossRef] [PubMed] [Google Scholar]
- Arthrodiatasis for the treatment of perthes' disease. Orthopedics. 2009;32:817.
- [CrossRef] [PubMed] [Google Scholar]
- Arthrodiastasis and surgical containment in severe late-onset perthes disease: An analysis of 14 patients. Acta Orthop Belg. 2010;76:329-34.
- [Google Scholar]
- Management of late onset perthes: Evaluation of distraction by external fixator-5-year follow-up. Adv Orthop. 2014;2014:135236.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of late-onset legg-calve-perthes disease by arthrodiastasis. Clin Orthop Surg. 2016;8:452-7.
- [CrossRef] [PubMed] [Google Scholar]
- Hinged versus fixed arthrodiastasis in late-onset Perthes' disease. Egypt Orthop J. 2018;53:367-72.
- [CrossRef] [Google Scholar]
- Hip arthrodiastasis in legg-calvé-perthes disease. Rev Esp Cir Ortop Traumatol. 2016;60:243-50.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of severe late-onset perthes' disease with soft tissue release and articulated hip distraction: Revisited at skeletal maturity. J Child Orthop. 2007;1:229-35.
- [CrossRef] [PubMed] [Google Scholar]
- Initial experience of use of an articulated external fixator in treating legg-calvé-perthes disease by means of arthrodiastasis during the active phase of the disease. Rev Bras Ortop. 2016;51:337-45.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanical failure of external fixator during hip joint distraction for perthes disease. J Orthop Sci. 2007;12:385-9.
- [CrossRef] [PubMed] [Google Scholar]
- Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (Grading of recommendations, assessment, development and evaluation (GRADE) working group)
- [Google Scholar]
- Handbook for conducting a literature-based health assessment using OHAT approach for systematic review and evidence integration: Institute of Environmental Health Sciences 2019.
- [Google Scholar]







