Translate this page into:
The evolution of nerve transfer restoration of shoulder function
2 Medical School, University of Birmingham, Birmingham, UK
Corresponding Author:
Dominic M Power
Hand and Peripheral Nerve Unit, Queen Elizabeth Hospital Birmingham, Mindelsohn Way, Birmingham B15 2TH
UK
dominic.power@uhb.nhs.uk
| How to cite this article: Power DM, Parthiban S, Nassimizadeh M, Jimulia D, Turner L, Jones R. The evolution of nerve transfer restoration of shoulder function. J Musculoskelet Surg Res 2019;3:47-52 |
Abstract
Loss of shoulder abduction and external rotation reduces the working space for the upper limb and hand. Paralysis may follow C5 nerve root avulsion, upper trunk rupture or isolated injuries to the suprascapular and axillary nerves. Motor nerve transfer surgery involves a direct transfer of an expendable motor branch from a muscle in the vicinity of the paralyzed muscle and direct transfer with microsurgical end-to-end coaptation to the nerve to the denervated muscle close to its motor point. Reinnervation is rapid and robust. The technique was described for the restoration of deltoid function more than a century ago but was not adopted into wide spread use until the past two decades. This article explores the various options of nerve transfer surgery to restore function of shoulder function and reviews the evidence. Refinements in the procedure have resulted with the current algorithm for management, which will be described with its rationale and a review of clinical outcomes.Introduction
Nerve transfer surgery has provided a reliable method for restoration of motor function to muscles left paralyzed from a neurological injury. A motor fascicle from within an intact nerve between branch points (fascicular transfer) or a motor branch from a muscle in the vicinity of a functionally more important paralyzed muscle (nerve transfer), maybe microsurgically coapted end-to-end close to the motor point of the denervated muscle. The donor nerve is harvested distally and the recipient motor branch proximally to allow a direct tension free coaptation.[1] Neural regeneration is rapid and targeted, enhanced through strong neurotrophic stimulation from the denervated muscle. Reinnervation is usually achieved in 3 months with muscle tenderness on palpation, flickers of contraction between 3 and 6 months and functional contraction by 12 months. Neural plasticity enables the independent function of the donor and recipient, even when the donor function is preserved through selective fascicle transfer. The process of strengthening and plasticity is variable for different patients and different nerve transfers but is usually complete within 2 years.
Nerve transfer has gained traction as a reconstruction technique in cases of irreparable nerve injury. Following C5 nerve root avulsion, there is the loss of axillary nerve and supraspinatus nerve function resulting in paralysis of shoulder abduction and external rotation. There is no option to repair the C5 root other than spinal cord reimplantation, which does not give meaningful motor recovery. Nerve transfers to the supraspinatus and axillary nerve provide a means for reinnervation and the results are such that surgeons will consider nerve transfer surgery as the primary technique in upper trunk ruptures and isolated injury to the axillary and suprascapular nerves rather than direct anatomical repair of the injured nerve with graft interposition. This is particularly useful as salvage when proximal reconstruction of the upper trunk has failed, the primary nerve injury is extensive, the surgical bed at the site of nerve injury is scarred or the patient presents too late for reliable proximal reconstruction to be successful. This paradigm shift has driven further exploration of the techniques with the aim of further enhancing the outcomes for patients with shoulder paralysis through refinements.
The focus of this report is on describing the various options for nerve transfer surgery around the shoulder, the potential benefits and reviewing the evidence base. The algorithm for management in a specialist peripheral nerve injury service is presented [Figure - 1].
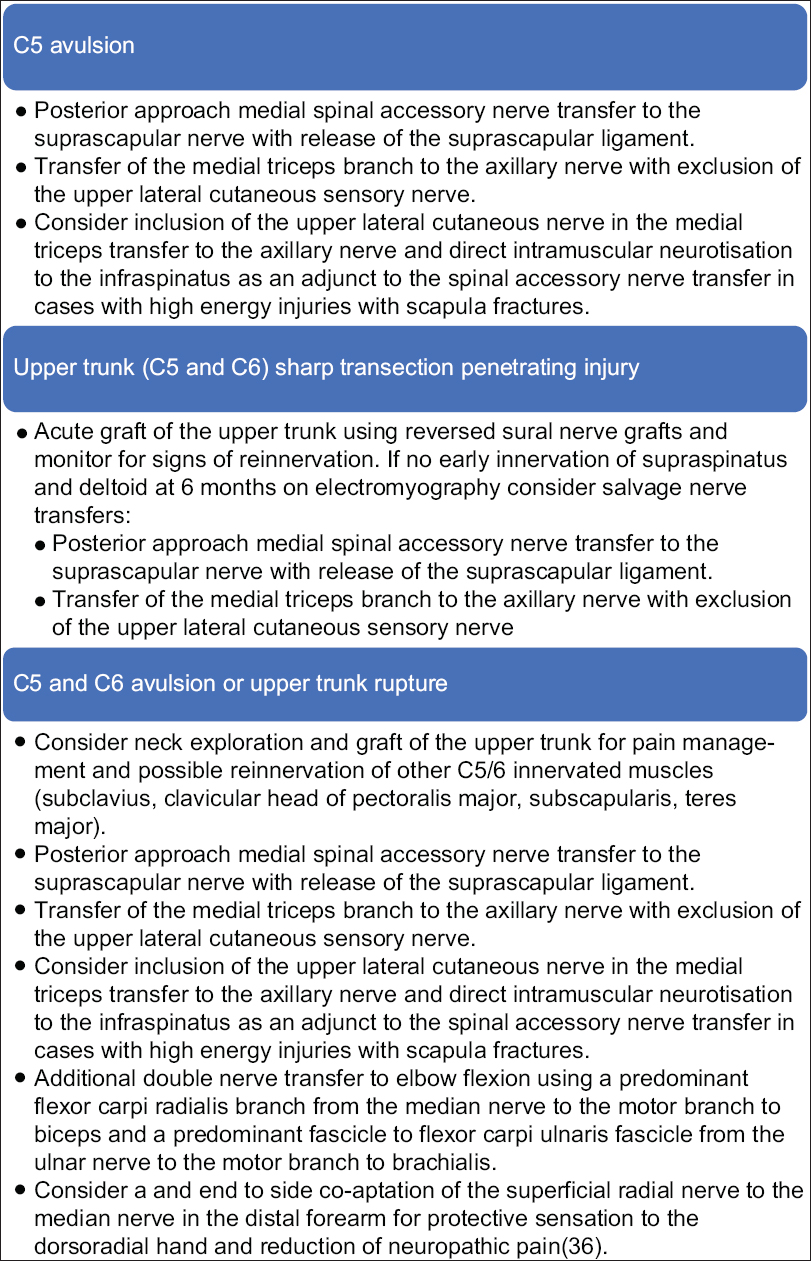 |
| Figure 1: Birmingham algorithm for nerve restoration surgery in the shoulder |
Anatomy
The suprascapular nerve (SSN) arises as a branch from the upper trunk in the posterior triangle of the neck and courses posterolaterally toward the scapular spine where it passes under the suprascapular ligament, through the suprascapular notch to the supraspinous fossa of the scapula. The first branch is the innervation to the supraspinatus, and this leaves the main nerve trunk immediately posterior to the notch. The remainder of the nerve passes laterally. Around the base of the spine of the scapula medial to the glenoid through the spinoglenoid notch to the infraspinous fossa where it supplies the infraspinatus.
The nerve is at risk of injury during traction due to contralateral neck flexion and shoulder girdle depression, typical of high-energy adult traumatic brachial plexus injuries. The supraspinatus and infraspinatus are rotator cuff muscles and are integral to shoulder function, stabilizing the humeral head in the glenoid and the supraspinatus depressing the head during the initiation phase of abduction with deltoid activation. The infraspinatus is a strong external rotator in the adducted position of the shoulder.
The deltoid muscle is supplied by the axillary nerve, which branches from the posterior cord in the infraclavicular brachial plexus. The deltoid innervation arises from the posterior division of the upper trunk (C5) and so is completely lost in a C5 avulsion injury or upper trunk (C5–6) rupture, but also in isolated injury to the axillary nerve, which may be avulsed from the posterior cord or ruptured within the quadrilateral space during shoulder dislocation or the displacement of proximal humeral fractures.[2] The axillary nerve provides innervation to the deltoid and teres minor muscles with sensory innervation to the skin over the shoulder (the upper lateral cutaneous nerve of the arm).[3] The anterior and middle parts of the deltoid are supplied by the anterior branch of the axillary nerve and the posterior part of the deltoid has dual innervation from both the posterior and anterior branches of the axillary nerve in 89.1% of cases.[4] Leechavengvongs et al.[4] described a variation in the mapping of the axillary nerve to the deltoid muscle, with some individuals having a single innervation to the posterior part of the deltoid (2.3% from anterior branch only and 8.5% from posterior branch only). These anatomical variations are important to consider when reviewing the outcomes of different nerve transfer techniques for deltoid reinnervation.[5]
The deltoid is the prime shoulder abductor with central fibers important for power, anterior fibers contributing to forward flexion and posterior fibers to shoulder retropulsion. The teres minor arises from the lateral scapula and inserts over the lower facet of the greater tuberosity on the lateral humeral head. It lies in close proximity to the lower border of the infraspinatus and is a strong external rotator, particularly in the abducted shoulder. The sensory innervation of the axillary nerve and the nerve supply to the teres minor both arise from the posterior branch of the axillary nerve [Figure - 2].
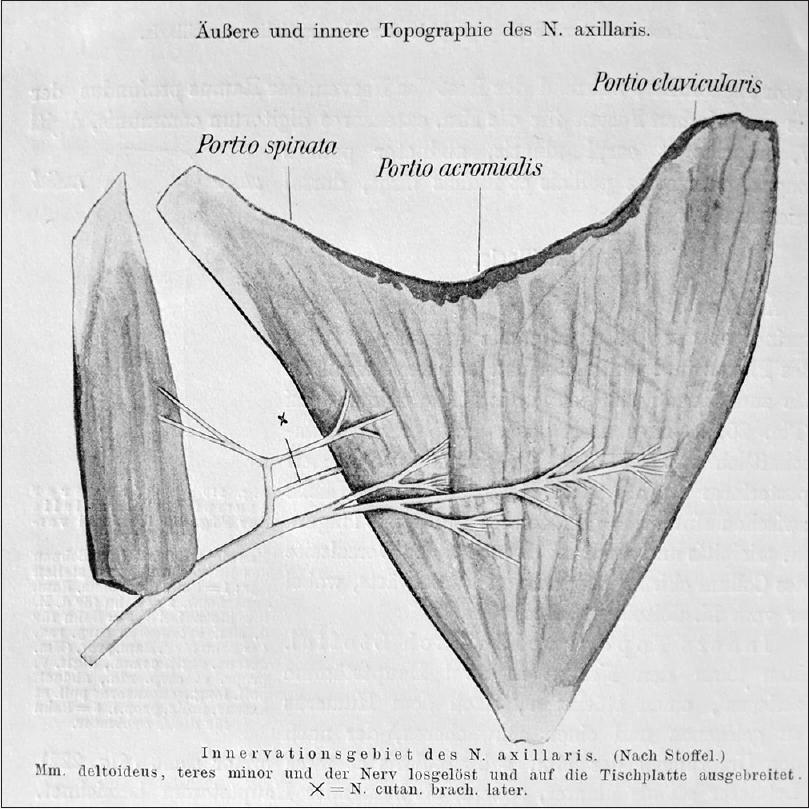 |
| Figure 2: Axillary nerve innervation of deltoid. Image taken from Orthopadische Operations, 1913[6] |
Historical Review
Tuttle is credited with one of the early descriptions of nerve transfer for restoration of function following a brachial plexus injury.[7] Part of the 4th cervical nerve was transferred to the spinal accessory nerve. Nerve stimulation was unavailable and the donor nerve would have contained both sensory and motor fibers.
Adolf Stoffel, an orthopedic surgeon, was working in Mannheim, Germany in the early 1900s. He had a major interest in peripheral nerve surgery for spasticity and paralysis. He co-authored a textbook, Orthopadische Operationshere on contemporaneous techniques in orthopedic surgery with Professor Oskar Vulpius, his mentor in Heidelberg. In the chapter “Operationen am Nervensystem” Adolf Stoffel details a number of innovative reconstructive techniques including triceps to axillary nerve transfer through an anterior approach in the axilla.[6] The textbook was published in 1911 in Germany and never translated into English, most likely due to the outbreak of World War 1. Effectively, this pioneering reconstructive technique was lost and it was almost a century later that the concept of nerve transfer from triceps to deltoid was revisited.
Reconstruction of the brachial plexus was considered to be futile with patients offered tendon transfers and shoulder arthrodesis until renewed interest in autologous nerve grafting with the advent of operating microscopes, instrumentation, and microsurgical sutures becoming more widely available in the 1960s. Tendon transfers often result in adhesive scar formation that restricts muscle and tendon gliding. Nerve transfers, however, generally leave the muscles undisturbed, thus reducing scare formation.[8]
Restoration of shoulder stability and movement was critical to useful upper limb function with isolated upper plexus injury.[9],[10] The limitations of nerve grafting include failed neural regeneration and co-contraction, particularly when multiple functions are restored through a single nerve root. In 1972, Kotani et al.[11] reported using the spinal accessory nerve as a source of motor axons for nerve transfer in brachial plexus surgery. During the neck exploration, the undamaged lateral branch of the spinal accessory nerve could be transferred directly to the denervated SSN for shoulder stability and some function in the supraspinatus and the infraspinatus. The technique could be performed in C5 avulsion and also in cases where the C5 root was ruptured and other roots avulsed such that only the C5 was available for grafting to more important distal functions. The success of the technique encouraged wide uptake and consideration of alternative targets including the musculocutaneous nerve.[12],[13] Direct reinnervation of a key paralyzed muscle with an undamaged donor nerve produced such reliable results that peripheral nerve surgeons started looking at additional donor and recipient options. The modern era of motor nerve transfer surgery had begun.
The next major advance was in using fascicles from within the ulnar nerve at the mid-humeral level to transfer directly to the motor branch to biceps. Christophe Oberlin described his technique in 1994 with later clinical case series and modifications reporting excellent results with both single and double fascicle transfers for elbow flexion.[14],[15],[16],[17],[18],[19] The opportunity for restoration of biceps beyond 6 months in a nonrecovering obstetric brachial plexus injury radically changed the outcome for high-grade injuries and the wider surgical perception of nerve transfer surgery as a viable reconstructive strategy in complex peripheral nerve injury paralysis management.
Somsak Leechavengvongs trained under Oberlin and based on the improved results of a double transfer for elbow flexion, explored the concept of a double nerve transfer for shoulder abduction as an adjunct to spinal accessory nerve transfer. He described a posterior approach to the axillary nerve and reinnervation using the long head of the triceps branch from the radial nerve. The anterior division of the axillary nerve was selected for the target to avoid wasted reinnervation of the cutaneous sensory nerve, which arises from the posterior division while allowing reinnervation of the whole of the deltoid in the majority of cases.[4],[20],[21] The concept of a double nerve transfer with the lateral spinal accessory nerve to the SSN and long head of triceps transfer to the anterior axillary nerve became the default reconstruction for C5 avulsion injuries and was successful in functional restoration.
The timing of nerve transfer was examined by Fu and Gordon in 1995,[22],[23] building on the work of Holmes and Young[24] and demonstrating that reinnervation of a chronically denervated muscle with a freshly axotomized nerve conferred advantages over a chronically axotomized donor, and early reinnervation of a denervated muscle provided even greater advantages. These observations emphasized the benefits of early diagnosis, referral, and reconstruction in brachial plexus injuries.
A systematic review of outcomes in brachial plexus reconstruction by Merrell et al.[12] demonstrated reliable abduction restoration with the double transfer technique; however, shoulder external rotation was poorly reported and often limited in terms of the range of motion, strength, and endurance.
The focus shifted to improving the outcome of the shoulder in terms of external rotation. The potential problems with the lateral spinal accessory nerve transfer to the SSN using an anterior approach include denervation of the lateral trapezius, an important elevator of the shoulder girdle, a long reinnervation distance, to the target muscle, the potential for reinnervation proximal to a concomitant SSN rupture or continuity lesion at the suprascapular notch and failure to decompress the suprascapular ligament, which could impede neural regeneration. In addition, reinnervation of two muscles in a single nerve trunk favors the proximal muscle due to shorter denervation period and stronger neurotrophic stimulation.[25],[26],[27],[28] These possible explanations for poor external rotation restoration after nerve transfer to the SSN have served to further the technical refinements of nerve transfer from the spinal accessory nerve (XI) to the SSN and the posterior approach using the medial branch of the spinal accessory nerve is favored with evidence of superior results[25],[29] [Table - 1]. Despite these refinements, in a proportion of patients there remains no useful function in the infraspinatus. Baltzer et al.[27] defined electromyographic reinnervation in 85% of 51 patients with useful function achieved in only 31%. A possible explanation could be additional damage to the infraspinatus branch of the SSN at the spinoglenoid notch sustained at the time of injury that goes unrecognized. Further refinements are suggested with a recent cadaveric study by Power[30],[31] demonstrating a transfer to the infraspinatus using the reinnervated upper lateral cutaneous branch of the axillary nerve as a conduit for direct transfer to the infraspinous branch of the SSN or for direct intramuscular neurotization as an adjunct in cases where the SSN has been reinnervated, but the outcome is uncertain.

This procedure is performed at the time of a concomitant triceps to axillary nerve transfer in a C5 injury. Wyles et al.[32] have recently described a technique for selective reinnervation of the infraspinatus branch of the SSN from the triceps. The efficacy of these refinements of the nerve transfer to SSN must be evaluated in clinical studies.
Susan Mackinnon described a surgical technique for simultaneous medial triceps branch transfer to the axillary nerve and medial spinal accessory transfer to the SSN through a posterior approach.[29] The rationale is that the medial triceps branch is longer than the long head of triceps branch and that transfer to the axillary nerve allows reinnervation of the whole of the deltoid as well as the teres minor, providing a more reliable restoration of external rotation than excluding the posterior division of the axillary nerve. The upper lateral cutaneous nerve is excluded to avoid wasted motor axon reinnervation of the sensory branch. The sensory branch is co-apted distally, end to side to the radial nerve sensory fascicles to improve sensory recovery to the upper arm and reduce deafferentation pain. Wolfe et al. published an anatomical study, which found a significant correlation between axon count and clinical success. They found that a donor to recipient axon ratio of <0.7:1 to be associated with a reduction in clinical success.[33],[34] A study by Khair et al.[35] found an equivalent number of motor axons between the long head of triceps branch (2302 axons) and the medial head of triceps branch (2198 axons) in their cadaveric study. Combined with the superior results of the posterior spinal accessory to suprascapular nerve, this approach provides reliable results for both shoulder abduction and external rotation.
There are additional advantages to using the medial triceps branch as a donor nerve for the axillary nerve [Table - 2]. The length is sufficient that coaptation can be performed close to the deltoid muscle facilitating rapid reinnervation and allowing for reconstruction where the axillary nerve is ruptured in the quadrangular space. Transfer can always be made without graft and can bypass a damaged segment of the axillary nerve. In cases of axillary nerve avulsion, the length is sufficient for direct intramuscular neurotization. Khair et al.[35] published an anatomical study, which supported the use of the medial triceps branch, with its greater swing distance compared to the long head of the triceps branch. They also found that the nerve to the long head of triceps transfer often required the release of the teres minor while the medial branch of triceps could be coapted to the axillary nerve without further resection of muscle.
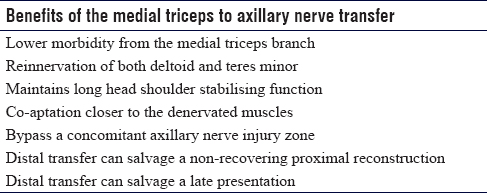
The use of the long head of the triceps branch as a donor's nerve is fundamentally flawed. In cases of a complete C5 lesion, the only muscle providing any stability of the shoulder to prevent inferior subluxation of the humeral head is the long head of triceps because it crosses the shoulder joint with origin at the infraglenoid tuberosity of the scapula. It is also a biarticular muscle providing proprioceptive feedback and positional control during elbow flexion. In the forward flexed shoulder position, the long head stabilizes the shoulder joint posteriorly. The long head of the triceps nerve should not, therefore, be sacrificed. The medial triceps function is for powerful extension from the deep flexed elbow position and provides proprioceptive control in this position. Following harvest of the medial branch, patients regain deep flexion control within 6 weeks of transfer due to adaptive changes in the residual triceps head. During the reinnervation phase following medial triceps transfer to the axillary nerve, it is possible to demonstrate the preserved long head function relocating the shoulder joint when extending the extended shoulder against resistance.
Bertelli and Ghizoni have described using the medial triceps branch for reinnervation of the anterior division of the axillary nerve through an anterior approach in 2014.[36] The advantages reported include the concomitant biceps and brachialis reinnervation through the same incision in C5 and C6 combined injuries, the length of the donor nerve, the inclusion of the branch to the anconeus (which although not specified in the report by Mackinnon,[29] is typically included in the posterior approach) and the ability to transfer without release of the teres major tendon, which was sometimes necessary in the transfer of the long head branch of triceps to the anterior division of the axillary nerve described by Leechavengvongs et al.[20],[21] It does not comment on the challenge of potentially reinnervating proximal to an injured segment of axillary nerve nor the added reinnervation distance. The technique described is almost identical to that first described by Adolf Stoffel in 1913, a century earlier. There is no proven advantage of this approach to the other modifications previously described.
Conclusion
Nerve transfer surgery has provided predictable results in otherwise nonreconstructable nerve root avulsion injuries to the brachial plexus. The reliable results have resulted in wider exploration in other nerve injuries that would conventionally have been reconstructed with grafts. Refinement of the techniques has continued to improve the functional results, but care should be taken when comparing outcomes of different techniques to ensure that similar indications, the timing of surgery, patient demographics, and comparable techniques are being presented. Defining a core outcome dataset for such reconstruction cases would enhance systematic review of outcomes. The posterior approach to the XI to SSN transfer has distinct advantages over the anterior approach and combined with a medial triceps branch transfer to the axillary nerve restores useful power of abduction and external rotation in the majority of cases, probably through facilitating moderately useful function in two synergistic muscles for each function, resulting in a greater proportion of Medical Research Council muscle Grade 4 function results than would be expected for single nerve transfers.
The pioneering work of Adolf Stoffel described the transfer modifications re-described by Bertelli et al. more than a century later. As peripheral nerve surgeons at the forefront of surgical innovation, we must ensure that we are also scholars of history.
Ethical approval
No ethical approval was required for the publication of this review.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Author's contributions
DMP conceived the aims of this review and gave input into the planning of the article and production of the final draft. SP wrote the initial and final draft. MN provided the image and gave input into the final draft. DJ, LT and RJ all gave input in the final draft and assisted with the literature searches. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Ray WZ, Mackinnon SE. Management of nerve gaps: Autografts, allografts, nerve transfers, and end-to-side neurorrhaphy. Exp Neurol 2010;223:77-85. [Google Scholar] |
| 2. | Rea P. Upper limb nerve supply. Essential Clinically Applied Anatomy of the Peripheral Nervous System in the Limbs. London: Elsevier; 2015. p. 41-100. [Google Scholar] |
| 3. | Tubbs RS, Oakes WJ, Blount JP, Elton S, Salter G, Grabb PA, et al. Surgical landmarks for the proximal portion of the axillary nerve. J Neurosurg 2001;95:998-1000. [Google Scholar] |
| 4. | Leechavengvongs S, Teerawutthichaikit T, Witoonchart K, Uerpairojkit C, Malungpaishrope K, Suppauksorn S, et al. Surgical anatomy of the axillary nerve branches to the deltoid muscle. Clin Anat 2015;28:118-22. [Google Scholar] |
| 5. | Okazaki M, Al-Shawi A, Gschwind CR, Warwick DJ, Tonkin MA. Outcome of axillary nerve injuries treated with nerve grafts. J Hand Surg Eur Vol 2011;36:535-40. [Google Scholar] |
| 6. | Vulpius O. Orthopadische Operations. Stuttgart: Ferdinand Enke; 1913. [Google Scholar] |
| 7. | Tuttle HK. Exposure of the brachial plexus with nerve-transplantation. J Am Med Assoc 1913;61:15. [Google Scholar] |
| 8. | Tung TH, Mackinnon SE. Nerve transfers: Indications, techniques, and outcomes. J Hand Surg Am 2010;35:332-41. [Google Scholar] |
| 9. | Bhandari PS, Maurya S. Recent advances in the management of brachial plexus injuries. Indian J Plast Surg 2014;47:191-8. [Google Scholar] |
| 10. | Chuang DC, Lee GW, Hashem F, Wei FC. Restoration of shoulder abduction by nerve transfer in avulsed brachial plexus injury: Evaluation of 99 patients with various nerve transfers. Plast Reconstr Surg 1995;96:122-8. [Google Scholar] |
| 11. | Kotani P, Matsuda H, Suzuki T. Trial surgical procedures of nerve transfer to avulsion injuries of plexus brachialis. Orthop Surg Traumatol 1972:348-50. [Google Scholar] |
| 12. | Merrell GA, Barrie KA, Katz DL, Wolfe SW. Results of nerve transfer techniques for restoration of shoulder and elbow function in the context of a meta-analysis of the English literature. J Hand Surg Am 2001;26:303-14. [Google Scholar] |
| 13. | Allieu Y, Cenac P. Neurotization via the spinal accessory nerve in complete paralysis due to multiple avulsion injuries of the brachial plexus. Clin Orthop Relat Res 1988;237:67-74. [Google Scholar] |
| 14. | Oberlin C, Béal D, Leechavengvongs S, Salon A, Dauge MC, Sarcy JJ, et al. Nerve transfer to biceps muscle using a part of ulnar nerve for C5-C6 avulsion of the brachial plexus: Anatomical study and report of four cases. J Hand Surg Am 1994;19:232-7. [Google Scholar] |
| 15. | Loy S, Bhatia A, Asfazadourian H, Oberlin C. Ulnar nerve fascicle transfer onto to the biceps muscle nerve in C5-C6 or C5-C6-C7 avulsions of the brachial plexus. Eighteen cases. Ann Chir Main Memb Super 1997;16:275-84. [Google Scholar] |
| 16. | Mackinnon SE, Novak CB, Myckatyn TM, Tung TH. Results of reinnervation of the biceps and brachialis muscles with a double fascicular transfer for elbow flexion. J Hand Surg Am 2005;30:978-85. [Google Scholar] |
| 17. | Liverneaux PA, Diaz LC, Beaulieu JY, Durand S, Oberlin C. Preliminary results of double nerve transfer to restore elbow flexion in upper type brachial plexus palsies. Plast Reconstr Surg 2006;117:915-9. [Google Scholar] |
| 18. | Oberlin C, Ameur NE, Teboul F, Beaulieu JY, Vacher C. Restoration of elbow flexion in brachial plexus injury by transfer of ulnar nerve fascicles to the nerve to the biceps muscle. Tech Hand Up Extrem Surg 2002;6:86-90. [Google Scholar] |
| 19. | Ray WZ, Pet MA, Yee A, Mackinnon SE. Double fascicular nerve transfer to the biceps and brachialis muscles after brachial plexus injury: Clinical outcomes in a series of 29 cases. J Neurosurg 2011;114:1520-8. [Google Scholar] |
| 20. | Witoonchart K, Leechavengvongs S, Uerpairojkit C, Thuvasethakul P, Wongnopsuwan V. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part I: An anatomic feasibility study. J Hand Surg Am 2003;28:628-32. [Google Scholar] |
| 21. | Leechavengvongs S, Witoonchart K, Uerpairojkit C, Thuvasethakul P. Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part II: A report of 7 cases. J Hand Surg Am 2003;28:633-8. [Google Scholar] |
| 22. | Fu SY, Gordon T. Contributing factors to poor functional recovery after delayed nerve repair: Prolonged denervation. J Neurosci 1995;15:3886-95. [Google Scholar] |
| 23. | Fu SY, Gordon T. Contributing factors to poor functional recovery after delayed nerve repair: Prolonged axotomy. J Neurosci 1995;15:3876-85. [Google Scholar] |
| 24. | Holmes W, Young JZ. Nerve regeneration after immediate and delayed suture. J Anat 1942;77:63-96.1. [Google Scholar] |
| 25. | Souza FH, Bernardino SN, Filho HC, Gobbato PL, Martins RS, Martins HA, et al. Comparison between the anterior and posterior approach for transfer of the spinal accessory nerve to the suprascapular nerve in late traumatic brachial plexus injuries. Acta Neurochir (Wien) 2014;156:2345-9. [Google Scholar] |
| 26. | Terzis JK, Kostas I, Soucacos PN. Restoration of shoulder function with nerve transfers in traumatic brachial plexus palsy patients. Microsurgery 2006;26:316-24. [Google Scholar] |
| 27. | Baltzer HL, Wagner ER, Kircher MF, Spinner RJ, Bishop AT, Shin AY, et al. Evaluation of infraspinatus reinnervation and function following spinal accessory nerve to suprascapular nerve transfer in adult traumatic brachial plexus injuries. Microsurgery 2017;37:365-70. [Google Scholar] |
| 28. | Pruksakorn D, Sananpanich K, Khunamornpong S, Phudhichareonrat S, Chalidapong P. Posterior approach technique for accessory-suprascapular nerve transfer: A cadaveric study of the anatomical landmarks and number of myelinated axons. Clin Anat 2007;20:140-3. [Google Scholar] |
| 29. | Colbert SH, Mackinnon S. Posterior approach for double nerve transfer for restoration of shoulder function in upper brachial plexus palsy. Hand (N Y) 2006;1:71-7. [Google Scholar] |
| 30. | Power D. Combined Transfer of the Medial Triceps Branch to the Infraspinatus Branch of the Suprascapular Nerve and the Axillary Nerve for Restoration of Shoulder Abduction and External Rotation in a Partial C5 Lesion Following Decompressive Foraminotomy: Cadaveric and Clinical Case Study. Presented at the Royal Society of Medicine; 2014. [Google Scholar] |
| 31. | Power D. Combined nerve transfer for shoulder abduction and external rotation in upper brachial plexus palsy: An anatomical study. Presented at British Society for Surgery of the Hand, 2014. [Google Scholar] |
| 32. | Wyles CC, Maldonado AA, Wagner ER, Houdek MT, Lachman N, Spinner RJ, et al. Proposed surgical technique to facilitate targeted reinnervation of the infraspinatus: A cadaveric feasibility study. Clin Anat 2019;32:131-6. [Google Scholar] |
| 33. | Schreiber JJ, Byun DJ, Khair MM, Rosenblatt L, Lee SK, Wolfe SW, et al. Optimal axon counts for brachial plexus nerve transfers to restore elbow flexion. Plast Reconstr Surg 2015;135:135e-41e. [Google Scholar] |
| 34. | Tötösy de Zepetnek JE, Zung HV, Erdebil S, Gordon T. Innervation ratio is an important determinant of force in normal and reinnervated rat tibialis anterior muscles. J Neurophysiol 1992;67:1385-403. [Google Scholar] |
| 35. | Khair MM, Schreiber JJ, Rosenblatt L, Byun DJ, Lee SK, Wolfe SW, et al. Axon counts yield multiple options for triceps fascicular nerve to axillary nerve transfer. J Hand Surg Am 2016;41:e405-10. [Google Scholar] |
| 36. | Bertelli JA, Ghizoni MF. Nerve transfer from triceps medial head and anconeus to deltoid for axillary nerve palsy. J Hand Surg Am 2014;39:940-7. [Google Scholar] |
Fulltext Views
5,322
PDF downloads
2,226





