Translate this page into:
The late diagnosis of nerve injuries following interscalene block and shoulder surgery
2 Department of Hand Surgery, Queen Elizabeth Hospital Birmingham, Birmingham, England, UK; Department of General Surgery, National University Health System, Singapore,
3 Department of Clinical Neurophysiology, Queen Elizabeth Hospital Birmingham, Birmingham, England, UK
4 Department of Critical Care and Anesthesia, Queen Elizabeth Hospital Birmingham, Birmingham, England, UK
5 Department of Hand Surgery, Queen Elizabeth Hospital Birmingham, Birmingham, England, UK
Corresponding Author:
Guang H Yim
Department of Plastic Surgery, Derriford Hospital, Derriford Road, Plymouth, PL6 8DH
UK
gyim@doctors.net.uk
| How to cite this article: Yim GH, Lin Z, Shirley CP, Isherwood P, Power DM. The late diagnosis of nerve injuries following interscalene block and shoulder surgery. J Musculoskelet Surg Res 2019;3:141-145 |
Abstract
Objectives: Interscalene blocks are commonly performed with the shoulder surgery, nerve injuries are reported to have the prevalence of 14% at 10 days postoperatively. While clinicians may be aware of the associated risk of nerve injury from either the surgery or the block, they may not recognize these nerve injuries. Our objectives were to determine factors contributing to injury and late referral. Methods: We searched our peripheral nerve injury database to identify a consecutive series of nerve injuries-associated with interscalene nerve block and the shoulder surgery. The identified cases were subject to clinical review and a review of the medical records including the consent form, anesthetic records, operation note, and the neurophysiology records. Results: Six cases of nerve injury were identified during a 24-month period. Half the patients experienced a delay of >6 months from injury to review, despite the documentation of persisting sensory and motor dysfunction. Regional anesthesia technique was not uniform. All patients required a specialist treatment from a regional peripheral nerve injury service. Conclusions: Clinicians should be aware that prolonged block duration is a feature of the potential nerve injury. The presence of a Tinel sign, autonomic dysfunction, and nerve pain in the distribution of the injured nerve are features suggesting nerve injury. Orthopedic surgeons should be able to recognize the nerve injury and seek early referral to the appropriate specialists. Where doubt exists, the patient should be referred for an urgent review by a peripheral nerve injury specialist.
Introduction
Interscalene block (ISB) of the brachial plexus using local anesthetic is an established technique that can be used instead of, or as an adjunct to general anesthetic for the upper limb surgery;[1] ISBs are particularly beneficial in managing postoperative pain. They can be either single-shot or continuous infusions,[2] with the latter providing an extended period of postoperative pain relief.[3] The ISB is commonly guided using ultrasound and/or nerve stimulation. Complications specific to ISB include phrenic nerve palsy,[4] central nervous system toxicity, pneumothorax, vascular injury,[5] Horner's syndrome,[6] bilateral block,[7] total spinal anesthesia,[8] vascular injection leading to seizure,[9] permanent neurological damage to the nerves or spinal cord,[10] and even death after unrecognized intrathecal placement.[11]
Nerve injury during the shoulder surgery without ISB is dependent on the procedure, the approach, and the experience of the surgeon. Surgical causes can be due to positioning, traction, arthroscopic ports, retraction, or direct surgical injury.[12] The incidence of neurological injuries for arthroscopic shoulder surgery ranges between 0.2% and 3%; with transient paresthesia reported in 10%–30% of procedures.[12] In the open shoulder surgery, nerve injuries are reported in 1%–2% of patients undergoing rotator cuff surgery, 1%–4% undergoing prosthetic arthroplasty, and 1%–8% undergoing surgery for anterior instability.[13] The majority of injuries are minor cutaneous nerve injuries and transient conduction block injuries to the brachial plexus, permanent neurological deficit rarely results.
The risk of nerve injury due to ISB itself is commonly quoted at 1 in 10,000.[14] When the shoulder surgery is conducted with ISB, the all-cause complication rate has been reported to have a prevalence of 14% at 10 days postoperatively. At 6 months postoperatively, the prevalence of nerve injury reduces to 0.9%; long-term complications are reported as 0.4%.[5] Fredrickson and Kilfoylereported a 3.5% all-cause complication rate with symptoms in ten patients out of 659 resolving within 1 month and 13 resolving between 1 and 6 months.[15] Just over one-third of the neurological injuries were attributed to blocks in the Fredrickson's series while the majority of the high-transient neurological complications were attributed to nonblock-related causes.[15] In the more recent study, single-shot ISB demonstrated a persistent postoperative nerve symptom prevalence of 3.5% for symptoms lasting >5 days and a prevalence of 2.5% for symptoms lasting >6 months. The prevalence of postoperative nerve symptoms was higher in those who had a continuous ISB. Those with symptoms lasting >5 days and >6 months were 12% and 8.7%, respectively.[16] The variation in complication rates is also dependent upon how nerve injury is defined, the study design, the thresholds for reporting, and duration of follow-up.[17]
The West Midlands Peripheral Nerve Injury Service is a regional tertiary referral center for complex peripheral nerve disorders, based in the United Kingdom. Patients referred with nerve injury are assessed by the multidisciplinary team, data is collected prospectively and stored on a database. We observed a cluster of patients with a brachial plexus level nerve injury-associated with interscalene regional anesthesia. Our objectives were to determine factors contributing to injury, late recognition and then develop recommendations to reduce the morbidity.
Materials and Methods
The nerve service database identified 730 new patient episodes during a 2 year period, September 1, 2011–August 31, 2013, inclusive. We conducted a search for patients with a documented brachial plexus injury, iatrogenic injury, and ISB/regional anesthesia. No cases were excluded from the study. The cases were subject to clinical review, a review of the medical records including the consent form, anesthetic records, operation notes, and the neurophysiology records.
Results
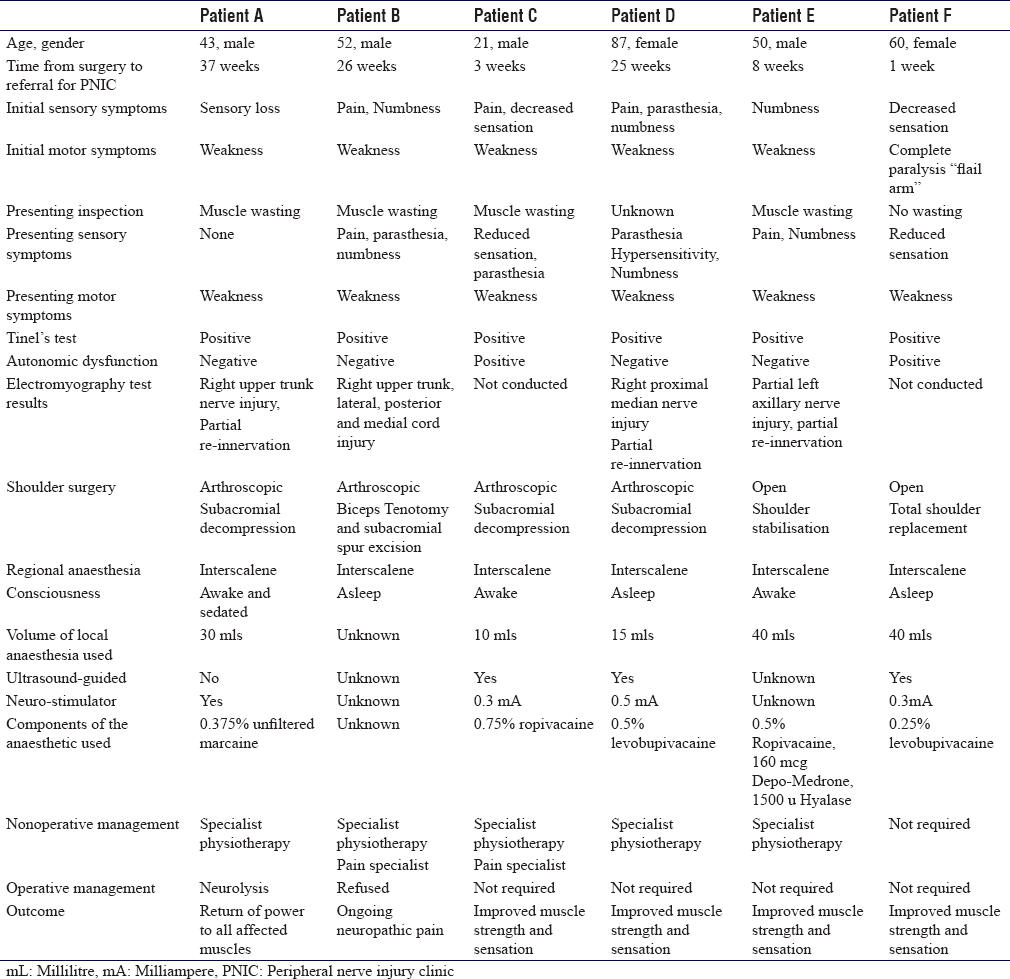
A total of six cases were identified. The characteristics of the six cases are presented in [Table - 1]. The mean age was 52 years with a range of 21–87 years. The operative procedures conducted were an open shoulder stabilization, a total shoulder replacement, and four arthroscopic procedures. Two cases of ISB were conducted with the patients awake, one case was sedated during the block, and three were asleep. All blocks were undertaken as a single-shot. Both ultrasound and nerve stimulators were used in three cases, nerve stimulation only was used in one, and there was no documentation in two cases. The mean volume of local anesthetic infiltrated was 27 mL with a median volume of 30 mL, range (10–40 ml). The choice of local anesthetic varied with 0.25%–0.5% levobupivacaine, 0.75% ropivacaine, and a mix of 0.5% ropivacaine, Depo-Medrone, and hyalase being used. The patients presented to the peripheral nerve injury service at a mean and median of 16.5 weeks postoperatively, range of 1–37 weeks. All patients had symptoms of the upper limb weakness, five had reduced sensation or numbness, three had paresthesia, and two had the symptoms of pain. These symptoms were present at the initial follow-up in the majority of cases. All patients had a positive Tinel's test over the site of the nerve injury which corresponded to the area of the ISB. Neurolysis was offered, if there was an absence of progression of Tinel's sign past the site of nerve injury. One patient underwent neurolysis in combination with specialist physiotherapy leading to a return of power to all affected muscles. The second patient was offered neurolysis but refused and underwent physical therapy and specialist pain intervention. Unfortunately, they continued to be affected by neuropathic pain. The other patients had evidence of an advancing Tinel's, which indicated nerve healing and were offered nonsurgical treatment. One patient required both specialist physiotherapy and pain specialist intervention leading to improved muscle strength and sensation. Two patients improved with specialist physiotherapy only. One patient's symptoms resolved with no intervention.
Discussion
Despite standard precautions, neurological injury can occur in the shoulder surgery with the reported procedure-dependent incidence of 0.2%–8%.[18] While there is a relative paucity of high-level randomized controlled studies addressing the benefits and potential complications of ISB,[19] the ISB is an established part of the treatment for patients undergoing shoulder surgery.
The main themes to highlight are the mean and median delay of 16.5 weeks from injury to review by the peripheral nerve injury service. Despite this delay in recognition and referring of the patients with complex brachial plexus injury, all patients had early documented evidence of at least one of the three cardinal signs of a degenerative nerve injury: pain, autonomic dysfunction, or a positive Tinel's sign at the site of the injury.
Review of the anesthetic charts demonstrated no standardisation of ISB technique, despite experience indicating standardisation improves success[5] and also reduces complication rates.[15] We observed a wide variation in local anesthetic volumes, local anesthetic types, and needle approach. There was also no system in place to flag up the early neurological complications.
The underlying reason we conducted a review of the cases was due to our observation of higher than the expected rate of persisting nerve injuries from the shoulder surgery with ISBs. There is inconsistency in the reporting of the incidence of permanent nerve injury in the published literature.[20] Previous large-scale reviews found that the identification of a direct causation link with surgery or anaesthesia is often not possible[5],[16] and in reality, it is likely to be multifactorial.[15],[21] Although in our series, all patients had a positive Tinel's test over the site of the nerve injury, which corresponded to the area of the ISB. This indicated that injury due to ISB was more likely to the cause rather than from the surgery. We noted the controversial practice of ISBs being conducted with patients under general anesthesia or sedated. This was despite consensus recommendations that ISB should not be routinely conducted with the patient under general anesthesia or following deep sedation.[1],[22],[23] The late recognition of perioperative nerve injury and lack of a robust system to capture postprocedure brachial plexus nerve injuries should cause concern for both anesthetists and surgeons. A retrospective review demonstrated that 29% of neurological injuries proceeding to medico-legal claims only became apparent after their discharge.[24]
There is published evidence that ISB anaesthesia when performed correctly is beneficial.[25] Although the ISB has specifically been associated with a statistically significant increased incidence of postoperative neurologic symptoms and contributed to 6 out of 12 cases with neurological symptoms that persisted >6 months.[16] There are currently efforts to find alternatives to ISB with either supraclavicular blocks[26] or suprascapular blocks.[27] Particularly, as the most contemporaneous estimation of prolonged nerve injury for single-shot ISB is 2.5% and for continuous ISB is 8.7% in a best-case scenario. At present, the authors recommend ISB should be performed only by trained anaesthetists who are experienced in this technique and adhere to published guidance on safe practice and documentation of the intervention.[28] The majority of patients who undergo ISB anesthesia will experience no long-term neurological sequelae,[5] however, a robust follow-up mechanism to capture the patients with the ongoing neurological deficit is beneficial and recommended.[29] Local follow-up pathways could be created with a delegation of responsibility to direct contact in the clinic if patients flag up issues of prolonged block or indirectly by telephone around 3 days into postoperative period.
Following shoulder surgery with ISB regional anaesthesia any patient with a history of a prolonged duration of block >48 h should be examined systematically to ascertain whether there is any residual neurological deficit. Conduction block may result in neurological dysfunction due to oedema or segmental demyelination. Full-resolution is to be anticipated by 3 months from the injury. Axonal injury with Wallerian degeneration is manifested with neuropathic pain, a positive Tinel's sign on percussing over the site of nerve injury and autonomic abnormalities with vasomotor and sudomotor dysfunction in the affected limb. All patients with a documented nerve injury should be referred to a regional specialist nerve injury service for further assessment. Neurolysis may assist axonal regeneration following axonopathy and may prevent deepening of a persistent conduction block injury. The British Orthopedic Association's Standards for Trauma 5 guidelines on peripheral nerve injury management provide further guidance on this complex issue.[30]
Of relevance for clinicians who conduct, review, and audit regional anaesthesia a medico-legal review of complications relating to ISB by Liang[29] recommended that documentation should include records of the length and type of the needle used, the nerve stimulator type and settings, strength and location of muscle contractions, the number of attempts, the presence or absence of paresthesia, and what was done about it. These recommendations are on top of the factors that should be routinely documented for all regional block which includes documenting premedication, asepsis, patient positioning, consciousness, sedation, the type of monitoring, ultrasound technique, and depth of the catheter placement.[31] The lists above are not exhaustive but are an aid to implementing to an appropriate documentation standard.
It is pertinent to orthopedic surgeons that while the majority are not anaesthetically trained, they are the “face” of the care given; any postdischarge anesthetic complications will be observed and managed initially by the surgeon. Therefore, orthopedic surgeons are well-positioned to promptly diagnose these complications. Should anaesthetists have concerns it would be beneficial to inform the surgical team, but if surgeons detect complications, it would be courteous to inform anaesthetists also. Clinicians of all specialties and grades should be mindful of nerve injury complications and how to manage them according to their local protocol. We accept that there are limitations from the small scale of our study and the lack of denominator from which to estimate the incidence or prevalence. While some may propose a prospective trial, we are pragmatic and feel that the available evidence from prospective clinical registries remains the most sensible way to balance the numbers needed to detect significant events versus the dilemma of who would fund such a large trial.
Conclusions
Our series demonstrated that nerve injuries were recognized late. Despite the late recognition, we were able to facilitate the improvement and resolution in the majority of cases through multidisciplinary specialist input. While, we are unable to attribute an incidence rate, contemporary evidence suggests that ISB is associated with statistically significant rates of nerve injury. There are efforts to seek alternative blocks, but in the meantime, we advocate vigilance for nerve injury if ISBs are used in conjunction with the shoulder surgery.
Recommendations
Clinicians should be aware that prolonged block duration is a feature of potential nerve injury. The education of patients to recognize prolonged block duration and how to obtain prompt clinical review would facilitate earlier recognition. The presence of a positive Tinel's sign, autonomic dysfunction, and nerve pain in the distribution of the injured nerve are features suggestive of nerve injury. Orthopedic surgeons should be able to recognize nerve injury and seek an early referral to the appropriate specialists.
Ethical approval
No ethical approval was required for the preparation of this article.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Author's contribution
GHY contributed to the literature search, data analysis, manuscript preparation, manuscript editing, manuscript review, and is the guarantor. ZL contributed to design, data acquisition, data analysis, manuscript editing, and manuscript review. CPS contributed to the definition of intellectual content, data acquisition, manuscript editing, and manuscript review. PI contributed to the definition of intellectual content, literature search, manuscript editing, and manuscript review. DMP contributed to the concept, design, the definition of intellectual content, literature search, data analysis, manuscript editing, and manuscript review. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Ghaleb A. Anesthesia for shoulder surgery: A review of the interscalene block and a discussion of regional vs. general anesthesia. Open Anesthesiol J 2012;6:18-28. [Google Scholar] |
| 2. | Bowens C Jr., Sripada R. Regional blockade of the shoulder: Approaches and outcomes. Anesthesiol Res Pract 2012;2012:971963. [Google Scholar] |
| 3. | Fredrickson MJ, Ball CM, Dalgleish AJ. Analgesic effectiveness of a continuous versus single-injection interscalene block for minor arthroscopic shoulder surgery. Reg Anesth Pain Med 2010;35:28-33. [Google Scholar] |
| 4. | Urmey WF, Talts KH, Sharrock NE. One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesth Analg 1991;72:498-503. [Google Scholar] |
| 5. | Borgeat A, Ekatodramis G, Kalberer F, Benz C. Acute and nonacute complications associated with interscalene block and shoulder surgery: A prospective study. Anesthesiology 2001;95:875-80. [Google Scholar] |
| 6. | Seltzer JL. Hoarseness and Horner's syndrome after interscalene brachial plexus block. Anesth Analg 1977;56:585-6. [Google Scholar] |
| 7. | Cook LB. Unsuspected extradural catheterization in an interscalene block. Br J Anaesth 1991;67:473-5. [Google Scholar] |
| 8. | Dutton RP, Eckhardt WF 3rd, Sunder N. Total spinal anesthesia after interscalene blockade of the brachial plexus. Anesthesiology 1994;80:939-41. [Google Scholar] |
| 9. | Korman B, Riley RH. Convulsions induced by ropivacaine during interscalene brachial plexus block. Anesth Analg 1997;85:1128-9. [Google Scholar] |
| 10. | Benumof JL. Permanent loss of cervical spinal cord function associated with interscalene block performed under general anesthesia. Anesthesiology 2000;93:1541-4. [Google Scholar] |
| 11. | Yanovski B, Gaitini L, Volodarski D, Ben-David B. Catastrophic complication of an interscalene catheter for continuous peripheral nerve block analgesia. Anaesthesia 2012;67:1166-9. [Google Scholar] |
| 12. | Marecek GS, Saltzman MD. Complications in shoulder arthroscopy. Orthopedics 2010;33:492-7. [Google Scholar] |
| 13. | Boardman ND, Cofield RH. Neurologic complications of shoulder surgery. Clin Orthop 1999;(368):44-53. [Google Scholar] |
| 14. | Auroy Y, Benhamou D, Bargues L, Ecoffey C, Falissard B, Mercier FJ, et al. Major complications of regional anesthesia in France: The SOS regional anesthesia hotline service. Anesthesiology 2002;97:1274-80. [Google Scholar] |
| 15. | Fredrickson MJ, Kilfoyle DH. Neurological complication analysis of 1000 ultrasound guided peripheral nerve blocks for elective orthopaedic surgery: A prospective study. Anaesthesia 2009;64:836-44. [Google Scholar] |
| 16. | Sites BD, Taenzer AH, Herrick MD, Gilloon C, Antonakakis J, Richins J, et al. Incidence of local anesthetic systemic toxicity and postoperative neurologic symptoms associated with 12,668 ultrasound-guided nerve blocks: An analysis from a prospective clinical registry. Reg Anesth Pain Med 2012;37:478-82. [Google Scholar] |
| 17. | Bruce BG, Green A, Blaine TA, Wesner LV. Brachial plexus blocks for upper extremity orthopaedic surgery. J Am Acad Orthop Surg 2012;20:38-47. [Google Scholar] |
| 18. | Rashid A, Abdul-Jabar H, Lam F. Nerve injury associated with shoulder surgery. Curr Orthop 2008;22:284-8. [Google Scholar] |
| 19. | Hughes MS, Matava MJ, Wright RW, Brophy RH, Smith MV. Interscalene brachial plexus block for arthroscopic shoulder surgery: A systematic review. J Bone Joint Surg Am 2013;95:1318-24. [Google Scholar] |
| 20. | Weber SC, Jain R. Scalene regional anesthesia for shoulder surgery in a community setting: An assessment of risk. J Bone Joint Surg Am 2002;84-A: 775-9. [Google Scholar] |
| 21. | Watts SA, Sharma DJ. Long-term neurological complications associated with surgery and peripheral nerve blockade: Outcomes after 1065 consecutive blocks. Anaesth Intensive Care 2007;35:24-31. [Google Scholar] |
| 22. | Beecroft CL, Coventry DM. Anaesthesia for shoulder surgery. Contin Educ Anaesth Crit Care Pain 2008;8:193-8. [Google Scholar] |
| 23. | Neal JM, Bernards CM, Hadzic A, Hebl JR, Hogan QH, Horlocker TT, et al. ASRA practice advisory on neurologic complications in regional anesthesia and pain medicine. Reg Anesth Pain Med 2008;33:404-15. [Google Scholar] |
| 24. | Lenters TR, Davies J, Matsen FA 3rd. The types and severity of complications associated with interscalene brachial plexus block anesthesia: Local and national evidence. J Shoulder Elbow Surg 2007;16:379-87. [Google Scholar] |
| 25. | Hadzic A, Gadsden J, Shariat AN. Local and nerve block techniques for analgesia after shoulder surgery. Anaesthesia 2010;65:547-8. [Google Scholar] |
| 26. | Guo CW, Ma JX, Ma XL, Lu B, Wang Y, Tian AX, et al. Supraclavicular block versus interscalene brachial plexus block for shoulder surgery: A meta-analysis of clinical control trials. Int J Surg 2017;45:85-91. [Google Scholar] |
| 27. | Hussain N, Goldar G, Ragina N, Banfield L, Laffey JG, Abdallah FW, et al. Suprascapular and interscalene nerve block for shoulder surgery: A systematic review and meta-analysis. Anesthesiology 2017;127:998-1013. [Google Scholar] |
| 28. | Bishop JY, Sprague M, Gelber J, Krol M, Rosenblatt MA, Gladstone J, et al. Interscalene regional anesthesia for shoulder surgery. J Bone Joint Surg Am 2005;87:974-9. [Google Scholar] |
| 29. | Liang BA, Ediale KR. Shouldering the evidence burden: Conflicting testimony in a case of interscalene block. J Clin Anesth 2005;17:131-3. [Google Scholar] |
| 30. | British Orthopaedic Association Standards in Trauma 5 Peripheral Nerve Injury. British Orthopaedic Association; 2012. Available from: https://www.boa.ac.uk/wp-content/uploads/2014/12/BOAST-5.pdf. [Last accessed on 2018 Oct 22]. [Google Scholar] |
| 31. | Gadsden J. Monitoring and Documentation. The New York School of Regional Anesthesia; 2013. Available from: http://www.nysora.com/regional-anesthesia/foundations-of-ra/3217-monitoring-and-documentation.html. [Last accessed on 2014 Jul 09]. [Google Scholar] |
Fulltext Views
8,014
PDF downloads
1,702





