Translate this page into:
The ulnar digital artery perforator flap for little finger defects: Using the abductor digiti minimi as a landmark – Surgical technique
*Corresponding author: J. Terrence Jose Jerome, Department of Orthopaedics, Hand and Reconstructive Microsurgery, Olympia Hospital and Research Centre, Trichy, Tamil Nadu, India. terrencejose@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jerome JTJ. The ulnar digital artery perforator flap for little finger defects: Using the abductor digiti minimi as a landmark – Surgical technique. J Musculoskelet Surg Res. 2024;8:420-5. doi: 10.25259/JMSR_226_2024
Abstract
This surgical technique article outlines the planning and harvesting methods for the ulnar digital artery perforator (UDAP) flap, using the abductor digiti minimi as a landmark for flap elevation. This approach demonstrates a reliable perforator and offers a wide range of coverage for little finger reconstruction, both on the palmar and dorsal sides. The UDAP flap is technically straightforward and easily accessible and results in minimal donor site morbidity, making it a highly viable option for little finger defects. The technique’s simplicity and effectiveness represent a significant advancement in reconstructive surgery for the little finger.
Keywords
Abductor digiti minimi
Little finger
Perforator flap
Reconstructive surgery
Ulnar digital artery
Volar defects
INTRODUCTION
Numerous techniques have been proposed to address the little finger palmar defects, each with its own set of advantages and limitations.[1-9] Skin grafts, while straightforward, require a suitable wound bed without exposed bones or tendons and often result in suboptimal cosmetic results. Various free flaps have been employed to cover ulnar defects.[1-9] However, these flaps often leave notable donor-site defects, necessitate the sacrifice of a major artery, and may require additional procedures for thinning or reshaping.
Local flaps, such as the cross-finger flap and the reverse ulnar hypothenar flap, have also been utilized. The drawbacks are the need for a second surgery and sacrificing the volar digital artery of the little finger. Local perforator flaps have recently been preferred due to their reliability, thinness, and reduced donor-site morbidity. These flaps leverage the reliable vascular network of the hypothenar region, where consistent perforator vessels are likely to be present.
This study focuses on using a pedicled perforator flap from the ulnar digital artery to reconstruct soft-tissue defects on the volar aspect of the little finger. Specifically, it presents the abductor digiti minimi muscle as a landmark for perforator identification, which may be considered a standard and effective method for locating perforators. The aim was to detail the planning and harvesting techniques and to demonstrate the range of coverage achievable with this flap.
Anatomical details of the ulnar digital artery perforator (UDAP) flap
The hypothenar region, known for its rich vascular network, has garnered significant attention as a potential donor site for both local and free flaps aimed at covering hand defects. Several studies have investigated and documented the vascular supply in this area, providing a foundation for its use in reconstructive surgery.
Research has identified the hypothenar region as a reliable donor site due to its consistent vascular supply, particularly from the ulnar digital artery.[1-9] Plancher et al.[1] highlighted its use in failed carpal tunnel syndrome, demonstrating the viability of this area for flap harvest. In addition, Kinoshita et al.[2] and Kojima et al.[3] confirmed the utility of the subcutaneous pedicle and reverse pedicle flaps in the hypothenar region.
Specifically, Omokawa et al.[4] identified the constant vascular supply from the ulnar digital artery, which provides a reliable and consistent blood supply, making it an excellent candidate for the development of perforator flaps.
The UDAP flap is designed based on perforators that emerge from the ulnar digital artery, ensuring a robust and dependable blood flow. These perforators allow for the creation of a flap that is thin, pliable, and well-suited for covering defects in the volar aspect of the little finger, providing both functional and esthetic benefits with minimal donor site morbidity.
INDICATION AND CONTRAINDICATIONS
The UDAP flap is ideal for reconstructing various defects. It is particularly effective for post-burn contracture defects, providing an excellent solution for restoring damaged areas resulting from burns.[5-7] In addition, it can be used to cover traumatic defects, offering reliable coverage for wounds caused by injury. The flap is also suitable for reconstruction following Dupuytren’s contractures’ release, helping restore function and appearance. Furthermore, it provides reliable coverage for amputation stumps of the little finger.
The presence of a painful neuroma may be considered as a contraindication. Inadequate subcutaneous fat padding is another contraindication, as insufficient fat may increase the risk of a painful scar or neuroma. Patients prone to significant edema and congestion may not be ideal candidates, as these issues can affect the viability of the flap. Finally, in cases of hand burns with multiple finger contractures and significant dorsal involvement, alternative flaps may be more suitable for reconstruction.
PRECISE MARKING
Use a hand-held Doppler to accurately identify and mark the UDAP before surgery to ensure precise flap design. For a distal-based flap, the perforators are identified close to the distal palmar crease. For a proximal-based flap, multiple large perforators are identified, and an intraoperative decision to sacrifice perforators depends on the flap mobility and arc of rotation to cover the defect.
ANESTHESIA AND PATIENT POSITIONING
The patient is positioned supine and undergoes surgery under supraclavicular brachial block anesthesia, with an upper arm tourniquet applied. Informed consent is diligently acquired from all patients, with active involvement of their relatives in the decision-making process. To ensure precision during the flap harvest, the procedure should be performed under magnification and tourniquet control.
SURGICAL TECHNIQUE
Flap design and preparation
The UDAP flap is planned over the ulnar aspect of the hypothenar eminence, specifically over the abductor digiti minimi muscle.
Incision and perforator identification
After preparing the defect, an incision is made over the volar aspect of the hypothenar eminence, directly over the abductor digiti minimi muscle [Video 1]. The perforators of the ulnar artery are then visualized both proximally and distally. Typically, a single large distal perforator is identified, which is usually located over the musculotendinous portion of the abductor digiti minimi.
Flap elevation
The flap can be raised either in a subfascial or suprafascial manner. Since this is a distal-based flap, the proximal perforators can be safely cauterized or ligated. The flap is dissected up to the distal perforator and then islanded on it. It is then rotated 180° to cover the defect. This flap can be made large enough to cover the entire volar aspect of the little finger up to the fingertip. The arc of rotation of the flap can extend to cover portions of the flexor region in the palm and the ulnar dorsum of the hand.
Donor site closure and post-operative care
The donor site can be closed primarily or, if needed, with multiple Z-plasties. Postoperatively, the finger is immobilized in a splint for 5–7 days. The splints are removed after one week, and sutures are removed at two weeks. For cases requiring longer immobilization, such as burn contractures, the immobilization period may be extended as necessary. A Kirschner wire may be used for three weeks, after which it is removed to begin therapy.
Illustrative case
A 14-year-old girl presented to us with a severe flexion contracture of her right little finger, significantly restricting her daily activities. She had sustained a burn injury at the age of 2, resulting in wounds over the volar aspect of the right little finger. Without treatment, the burns led to the development of a severe flexion contracture that progressively restricted her activities and affected the cosmetic appearance of her hand. Clinical examination revealed an inability to extend the little finger passively due to severe flexion contracture [Figures 1 and 2]. Radiographs showed a proximal interphalangeal joint flexion of more than 90°.

- Clinical picture of a 14-year-old girl with severe flexion contracture of the little finger following burns.

- Clinical picture showing a fixed flexion contracture of the little finger.
Considering the severity of the contracture and the need for extensive flap coverage, the UDAP flap was selected as a single-stage procedure. Before surgery, the UDAP was marked using a hand-held Doppler [Figure 3]. During the operation, the flexion contracture on the volar aspect of the little finger was released, exposing the flexor tendons and neurovascular bundles [Figure 4]. The little finger was straightened and maintained in position with a Kirschner wire.

- Doppler markings of the perforator guiding us to the distal perforator from the ulnar digital artery.

- The defect following contracture release, requiring the ulnar digital artery perforator flap.
The UDAP flap was elevated as a distal-based flap, with a consistently large perforator identified over the musculotendinous portion of the abductor digiti minimi [Figures 5 and 6]. The flap was, then, rotated 180° to cover the flexor defect on the little finger [Figure 7]. The donor site was closed primarily, and sutures were removed two weeks post-surgery. The little finger was immobilized with a splint for three weeks, after which the Kirschner wire was removed and physical therapy was initiated. At six weeks follow-up, the girl achieved a good range of motion in the little finger [Figures 8 and 9]. She returned to school and had a full range of movements at the final six-month follow-up.
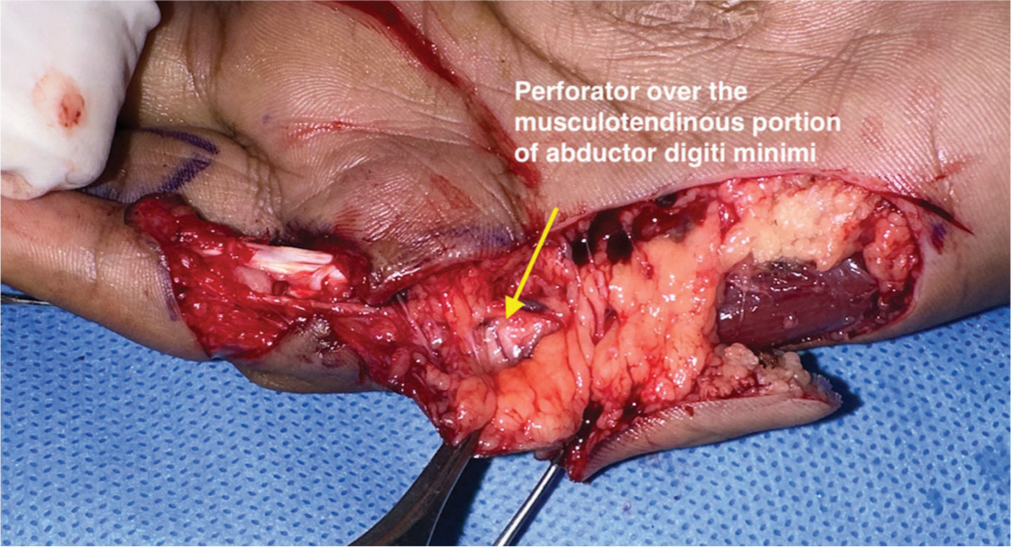
- Intraoperative picture showing a reliable distal perforator over the musculotendinous junction of the abductor digiti minimi.
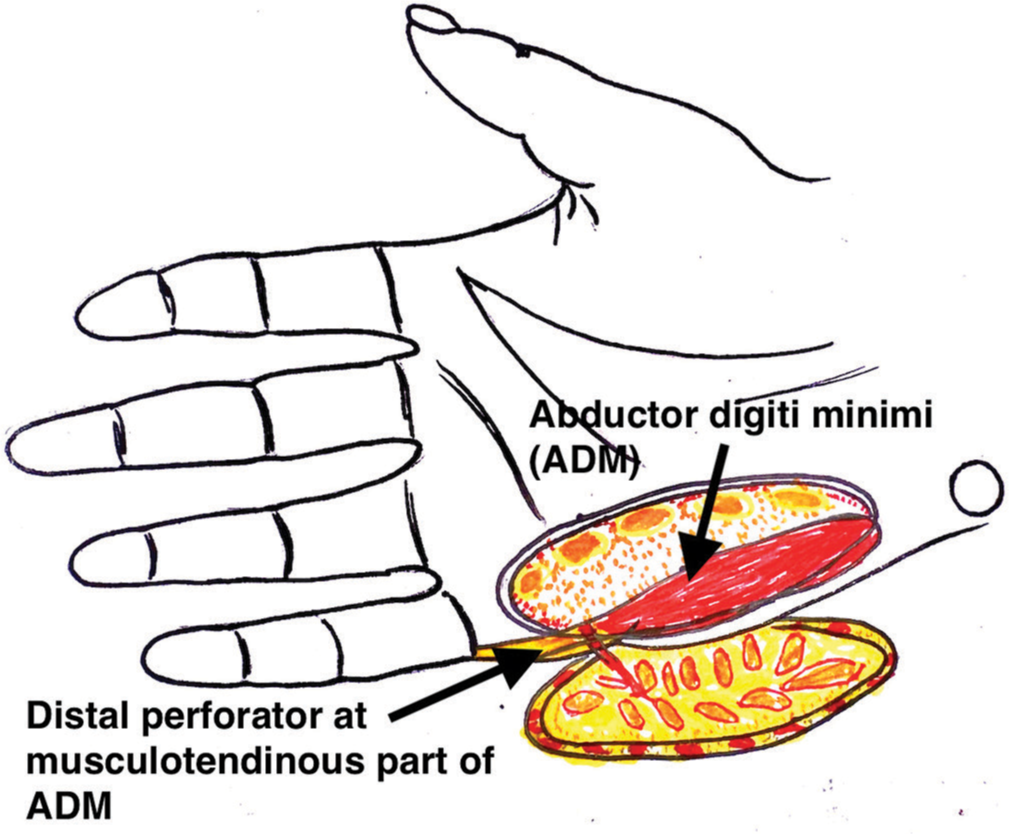
- Illustrative diagram of the flap showing the distal perforator located over the musculotendinous portion of the abductor digiti minimi.

- Immediate postoperative picture of the flap and little finger stabilized with a Kirschner wire to maintain deformity correction.

- Final follow-up picture with a well-settled flap over the flexor aspect of the little finger.

- Final follow-up picture with the little finger extended and no donor site morbidity.
In the authors’ series of six patients, there were four cases of post-burn contracture, one case of post-traumatic contracture, and one non-healing wound. All flaps healed well without any complications or donor-site morbidity.
Pearls
Accurate identification and marking of the UDAP using a hand-held Doppler before surgery ensures precise flap design. Performing the flap harvest under tourniquet control allows for meticulous dissection in a bloodless field, reducing intraoperative complications. Keeping the perforator moist with lignocaine solution during dissection helps prevent vasospasm and ensures optimal blood flow. Careful circumferential dissection of the flap while preserving the fat pad around the perforator minimizes the risk of kinking and post-operative congestion. Ensuring a tension-free flap inset avoids traction injury to the perforator, with initial sutures placed by its side before suturing the distal end. In addition, suprafascial dissection can help reduce flap bulkiness and improve mobility. Cosmetic results are generally acceptable, with no significant functional problems reported at the donor site, though post-operative edema is common and may persist, requiring careful monitoring and management. The UDAP flap offers the advantage of a single-stage procedure, providing thin, pliable coverage with good color and texture match and minimal donor site morbidity.
Pitfalls
The small perforator is highly susceptible to spasms with minimal traction, requiring gentle handling and continuous moisture maintenance to prevent complications. Damage to the palmar digital artery during dissection can cause ischemia of the little finger, highlighting the need for meticulous surgical technique. Post-operative venous congestion is common but typically resolves without active intervention. Subfascial dissection can lead to a bulky flap that restricts finger mobility, so suprafascial dissection is often preferred for better functional outcomes.
Complications
While the author has not encountered complications with this technique, it is essential to acknowledge the potential risks. Reported complications include partial flap necrosis and flap failure.
DISCUSSION
Hwang et al., in an anatomical examination of 18 cadaveric hands, identified consistent cutaneous perforators (ranging from 1 to 3) originating from the ulnar artery approximately 20.0 ± 7.0 mm distal to the pisiform.[8] However, locating the perforators using measurements from the pisiform is challenging. Uchida et al. observed 3–7 branches (an average of five) stemming from the ulnar digital artery. They noted at least one perforator within 9 mm of the metacarpophalangeal (MCP) joint, which they used as an anatomical landmark.[7] However, the anatomy and location of the MCP joint can vary between individuals, making it difficult to identify the perforators based on the MCP joint clinically and intraoperatively.
Toia et al., in their study of 14 cadaveric hands, used the proximal edge of the A1 flexor pulley as a landmark and described three to six perforators originating from the ulnar digital artery of the little finger and one to two from the ulnar artery, with distances ranging from 0 to 0.5 cm from their landmarks.[9] However, there is a risk of injuring the perforator or the distal neurovascular bundle while identifying the A1 pulley to locate the perforator. This study did not assess the venous supply to the flap but recommended a cuff of adipose tissue around the pedicle to ensure venous flow [Table 1].
| Authors | Study | Flap | Cutaneous perforator of ulnar digital artery | Remarks |
|---|---|---|---|---|
| Hwuang et al.[8] | Cadaver | Proximal based flap | 2±0.7 cm from the pisiform | The study did not evaluate the venous supply to the flap |
| Uchida et al.[7] | Cadaver | Distal based flap | 9 mm proximal to MCP joint | The flap was based on perforators but raised on a subcutaneous pedicle. |
| Toia et al.[9] | Cadaver | Distal based flap | 0.7 cm from the proximal margin of the A1 pulley | Proximal margin of the A1 pulley has been reported to be a few millimeters distal to the distal palmar crease |
| Panse and Sahasrabudhe[10] | Cadaver and 3 patients | Distal based flap | 3–5 mm distal to the distal palmar crease | Perforators near the MCP joint, distal to the distal palmar crease, had a larger caliber on visual inspection, although diameter has not been recorded |
| Winsauer et al.[11] | 17 patients | Both distal and proximal based flap | The proximal edge of the flap should be positioned at least 1.5 cm distal to the pisiform bone, and the distal edge of the flap should align with the level of the astrological “marriage” line, | This positioning helps to maximize the coverage area while maintaining optimal blood flow and minimizing the risk of flap failure. |
| Our study | 6 patients | Distal based | Musculotendinous junction of abductor digiti minimi | The distal palmar creases may serve as landmarks for the deeper neuro-vascular structures, but variations exist. |
MCP: Metacarpophalangeal joint
In a preliminary report, Panse and Sahasrabudhe described 3–4 perforators that arose from the ulnar digital artery, with the most distal perforator located 3–5 mm distal to the distal palmar crease.[10] Due to individual anatomical variations, the distal palmar crease cannot reliably serve as a landmark for locating the UDAP.[11,12]
Our study identified a consistent perforator over the musculotendinous portion of the abductor digiti minimi, proposing this as a reliable landmark for distal-based perforator flap elevation in little finger defects. Relying solely on measurement values and reference points such as the MCP joint, A1 pulley, or distal palmar crease can be problematic due to individual anatomical variations. Instead, the abductor digiti minimi muscle, which culminates in a tendon at the musculotendinous region, consistently reveals a larger and safer perforator from the ulnar digital artery, making it a dependable guide for flap elevation.
Our study offers easily identifiable landmarks to facilitate the design and elevation of the UDAP flap. However, it should be noted that we did not provide evidence demonstrating the superiority of our marking method over previously described techniques. Further, research is necessary to validate the effectiveness and reliability of these landmarks in clinical practice.
CONCLUSION
The ulnar digital artery perforator (UDAP) flap presents a reliable and effective option for reconstructing soft tissue defects in the little finger. Its consistent perforator location over the abductor digiti minimi muscle provides a dependable landmark for flap harvest. This flap offers several advantages, including a single-stage procedure, thin and pliable coverage, minimal donor site morbidity, and favorable cosmetic outcomes. However, surgeons should be aware of potential pitfalls such as perforator spasm, digital artery injury, and postoperative venous congestion.
While further research is needed to validate the superiority of the proposed landmark over existing techniques, the UDAP flap represents a valuable tool in the reconstructive surgeon’s armamentarium for addressing little finger defects. By understanding its anatomy, indications, contraindications, and surgical nuances, surgeons can effectively utilize this flap to achieve optimal functional and aesthetic results for their patients.
ETHICAL APPROVAL
The Institutional Review Board has waived the ethical approval for this study.
DECLARATION OF PATIENT CONSENT
The author certifies that he has obtained all appropriate patient consent forms. In the form, the patient’s parents have given their consent for the patient’s images and other clinical information to be reported in the journal. The parents understand that the patient’s name and initials will not be published, and due efforts will be made to conceal his/her identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
Video available on:
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Recalcitrant carpal tunnel. The hypothenar fat pad flap. Hand Clin. 1996;12:337-49.
- [CrossRef] [PubMed] [Google Scholar]
- Sub-cutaneous pedicle hypothenar island flap. Ann Plast Surg. 1991;27:519-26.
- [CrossRef] [PubMed] [Google Scholar]
- Reverse vascular pedicle hypothenar island flap. Handchir Mikrochir Plast Chir. 1990;22:137-44.
- [Google Scholar]
- A reverse ulnar hypothenar flap for finger reconstruction. Plast Reconstr Surg. 2000;106:828-33.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular anatomy of the integument In: Blondeel PN, Morris SF, Hallock GG, Neligan PC, eds. Perforators flaps anatomy, technique and clinical applications. Vol 1. St. Louis: Quality Medical Publishing Inc; 2006. p. :11-36.
- [Google Scholar]
- How large can a pedicled perforator flap be? Plast Reconstr Surg. 2012;130:195e-6.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical study of the perforators from the ulnar palmar digital artery of the little finger and clinical uses of digital artery perforator flaps. Scand J Plast Reconstr Surg Hand Surg. 2009;43:90-3.
- [CrossRef] [PubMed] [Google Scholar]
- Hypothenar flap based on a cutaneous perforator branch of the ulnar artery: An anatomic study. J Reconstr Microsurg. 2005;21:297-301.
- [CrossRef] [PubMed] [Google Scholar]
- The little finger ulnar palmar digital artery perforator flap: Anatomical basis. Surg Radiol Anat. 2013;35:737-40.
- [CrossRef] [PubMed] [Google Scholar]
- The ulnar digital artery perforator flap: A new flap for little finger reconstruction-A preliminary report. Indian J Plast Surg. 2010;43:190-4.
- [CrossRef] [PubMed] [Google Scholar]
- Pedicled hypothenar perforator flap: Indications and clinical application. J Plast Reconstr Aesthet Surg. 2016;69:843-7.
- [CrossRef] [PubMed] [Google Scholar]
- Can palmar creases serve as landmarks for the deeper neuro-vascular structures? Surg Radiol Anat. 2014;36:495-501.
- [CrossRef] [PubMed] [Google Scholar]






