Traumatic gluteus maximus femoral insertion tear
*Corresponding author: Khalid A. Abduldaem, SBOS. Department of Surgery, Prince Mohammed Bin Abdulaziz National Guard Hospital, Ministry of National Guard-Health Affairs, Madinah, Saudi Arabia. khalidabduldaem@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Abduldaem KA, Alyousif HA, Almuslami AY. Traumatic gluteus maximus femoral Insertion tear. J Musculoskelet Surg Res. 2024;8:166-71. doi: 10.25259/JMSR_210_2023
Abstract
With hip fracture dislocation, there is a wide variety of injuries, and one of the least and rarely to be seen is a gluteus maximus femoral insertion tear. We report this case to encourage further sharing of similar cases, establish a treatment protocol, and avoid such potential complications. We present this rare case of a 36-year-old male, a victim of a severe motor vehicle collision, who presented with a head contusion, right gluteus maximus femoral insertion tear, right hip dislocation with closed posterior wall acetabulum fracture, intra-articular incarcerated fragment, and multiple fractures. After the reduction of his hip and splinting of his concomitant fractures and optimization of the general condition, he underwent open reduction internal fixation of the posterior acetabulum wall. Intraoperatively, he found to have a rupture of gluteus maximus and short external rotators for which he had gluteus maximus direct repair to its insertion and partial repair for his severely damaged external rotators. The patient developed a surgical site infection post operation, treated by multiple sessions of irrigation and debridement and culture-based intravenous venous antibiotics for six weeks. At the 7-month outpatient clinical follow-up, the patient function was able to mobilize with a limping gait using a cane and extreme limitation of his abduction, external rotation, and extension due to the development of heterotopic ossification, which could be due to prolonged intensive care unit admission due to head injury or hip external rotators rupture or multiple surgeries that he underwent. This rare finding of gluteus maximus ruptur is the first of a kind in our institute, and such a finding to be considered before treatment of such severe injuries and questioning the need for magnetic resonance imaging for traumatic hip dislocations plus prophylactic treatment of heterotopic ossification to optimize the functional outcome post-operative.
Keywords
Acetabulum fracture
Gluteus maximus
Hip dislocation
Incarcerated fragment
Tendon rupture
INTRODUCTION
The hip is a ball-and-socket joint that is inherently stable due to its bony geometry and strong ligaments allowing it to resist significant increases in mechanical stress. Anatomic components contributing to the hip’s stability include the depth of the acetabulum, the labrum, the joint capsule, muscular support, and surrounding ligaments.[1] The gluteus maximus is the largest hip muscle and the main extensor. It has the least reported cases of traumatic injury regarding its size and strength. Traumatic hip dislocation represents approximately 5% of all traumatic joint dislocations with posterior dislocations of the hip being 85% of all cases. These are frequently associated with severe concomitant injuries due to the massive impact forces involved.[2] We encountered a rare case of posterior hip fracture dislocation with gluteus maximus femoral insertion tear in addition to other stabilizer injuries as intraoperative findings. These findings might be interpreted as part of a high-energy trauma reflecting on the outcome and prognosis of the patient’s condition.
We present here the management and short-term outcome of this injury. Despite a proper management approach to this complex case, the outcome might still be unsatisfactory. The literature on this topic is poor, and we hope more cases will be shared to initiate treatment protocols for traumatic gluteus maximus tendon rupture and hip external rotator tendons rupture with concomitant acetabulum fracture and its rehabilitation.
CASE REPORT
A 36-year-old healthy male patient, a known smoker, one pack per day, presented as a case of a frontal impaction with ejection from the car. He was the driver with a speed of 110 km/h. His car rolled over, and he was ejected from the car and then another car ran over him at this moment, and he lost consciousness.
The patient was evaluated in the emergency department and the required early management and splinting for his orthopedic injuries was utilized and then admitted directly to the intensive care unit. He was unstable vitally and agitated with a Glasgow Coma Scale of 9/15. Hemodynamic stabilization was achieved with a massive transfusion and inotropic support.
Clinical examination, orthogonal radiographs and whole body computed tomography (CT) were obtained and showed traumatic brain contusion, comminuted posterior acetabulum wall fracture with incarcerated intra-articular fragment (Thompson-Epstein Grade III), right anterior column non-displaced fracture, right sacrum (Denis 2), left superior rami fractures (Tile A1) and left iliac wing fracture [Figures 1-4], ipsilateral Gustilo type 3 A open tibia fracture, traumatic knee arthrotomy, and closed right proximal humerus fractures. Furthermore, he had other injuries in the chest, solid abdominal organs. The physical examination could not be performed appropriately at this stage, as the patient was fully sedated.
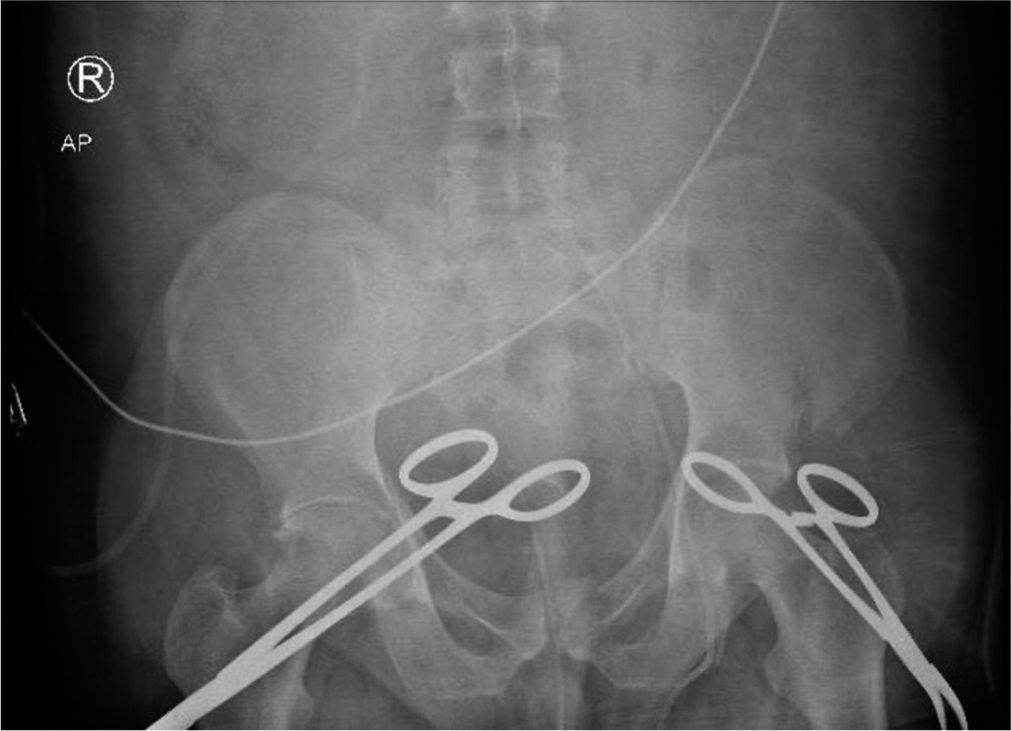
- Pelvis anterior posterior radiograph shows left iliac crest fracture, pelvic ring injury including left superior pubic rami fracture with possibility to involve symphysis pubis and right acetabulum posterior wall and column lines disruption with binder applied to the patient’s pelvis.
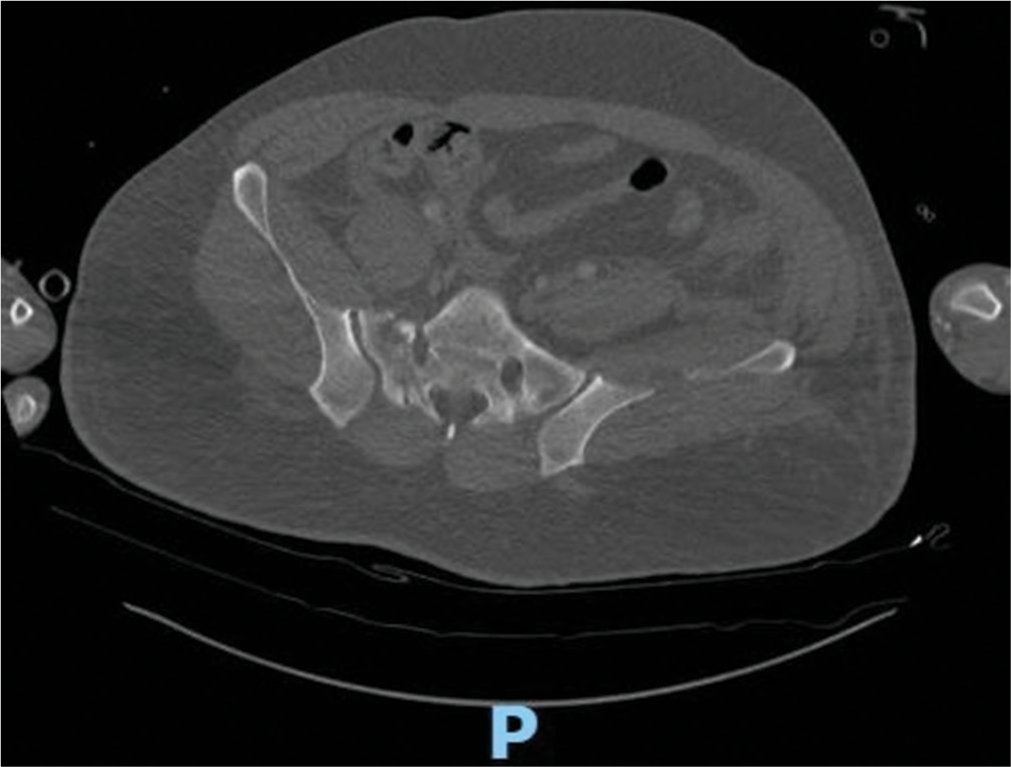
- Pelvis computed tomography axial cut shows right sacrum fracture Denis B and left ilium fracture.
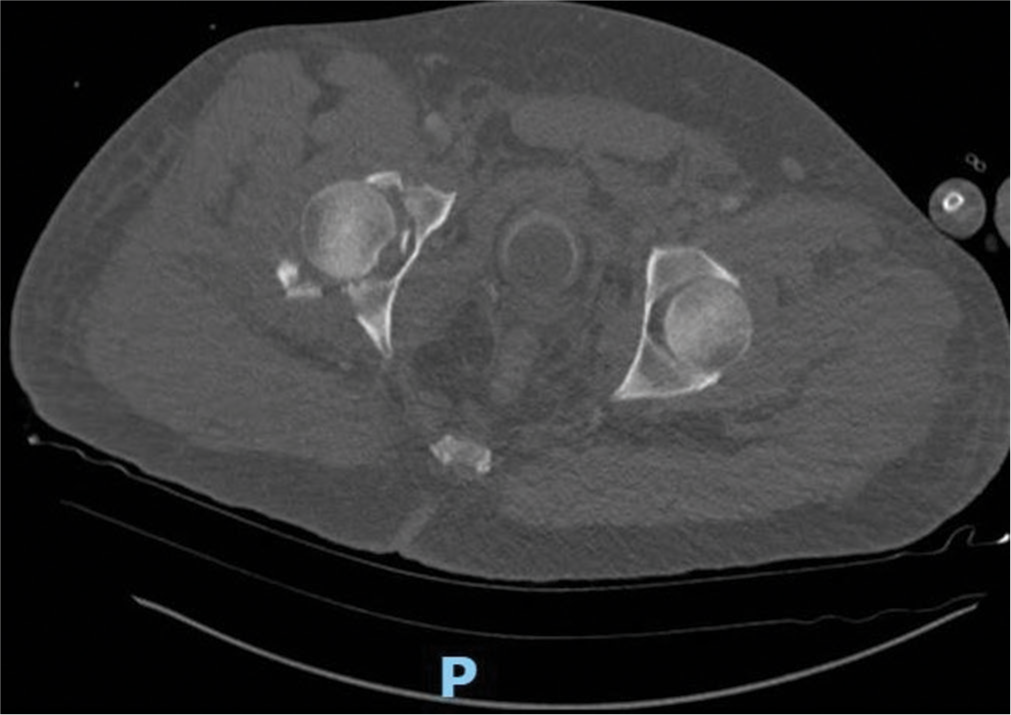
- Pelvis computed tomography axial cut shows right acetabulum fracture with incarcerated pieces of bone.

- Computed tomography 3D reconstruction shows right acetabulum posterior wall fracture, left iliac bone fracture, and sacrum fracture.
On day six after admission, the patient’s general condition improved, a detailed physical examination was obtained, and the patient was found to have a right foot drop and restricted range of motion at the right hip, knee, and shoulder. A right knee magnetic resonance imaging (MRI) showed a right multi-ligament knee injury. A hip MRI was not done for the patient, as it is not a protocoled practice for acetabulum fractures.
On day seven, the patient was taken for surgery. He was positioned in a supine position on a radiolucent table. The procedure was started with excessive irrigation and debridement of the traumatic arthrotomy of the right knee, then spanning knee external fixation was applied transfixing the tibia fracture, then repositioning the patient to left lateral decubitus with adequate support and pillow between the thighs before approaching the patient. We had difficulty in positioning his knee in flexion in the presence of the transfixing external fixator. For that, the patient’s position was accepted in extension of both hip and knee.
The Kocher-Langenbeck hip approach was utilized in classic fashion. We noticed excessive subcutaneous fluid oozing, which might indicate fluid overload. The tensor fascia lata was incised in line with the femur shaft and proximally. The gluteus maximus was identified and separated layer by layer bluntly. The muscle was severely traumatized [Figures 5 and 6]. During deep layer dissection, we encountered unexpected findings including complete avulsion of gluteus maximus femoral insertion, tear of gluteus minimums belly, and insertional tear of short external rotators with flimsy and partial necrosis muscle fibers with entrapment along the posterior wall fragments. The labrum and hip capsule were torn, flipped, and impinged in the articular space. The sciatic nerve was found intact but contused. Surgical steps proceeded with debridement of the necrotic traumatized tissues, irrigation of the hip joint, and then a Schanz pin inserted in the greater trochanter to distract the hip joint and remove the incarcerated fragment. After several trials, the fragments were removed, and a total of four fragments from the posterior wall were identified and fixed by a posterior wall buttress plate, spring plate, and an anchor suture size of 5 mm to suture the bony capsular fragment to the main osteosynthesis structure.
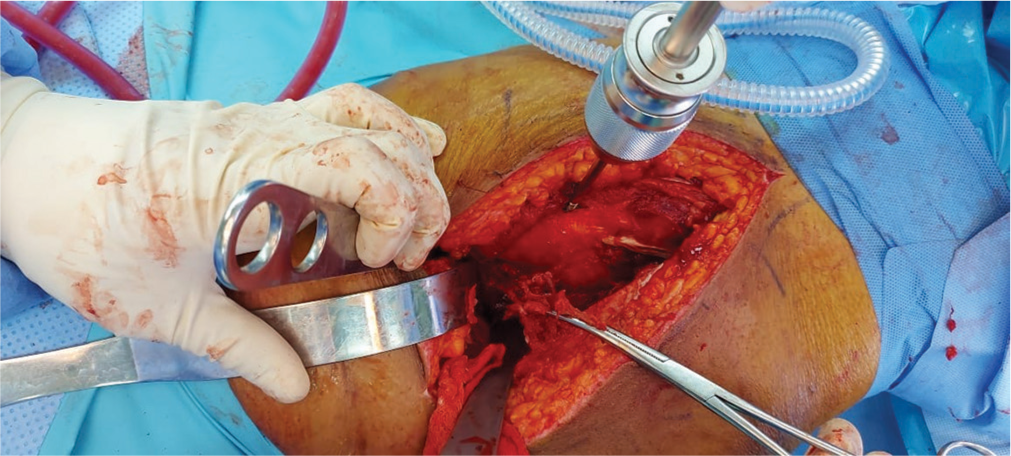
- Intraoperative image Kocher-Langenbeck approach to the right hip shows gluteus maximus tendon held in the forceps ruptured from its femoral insertion.
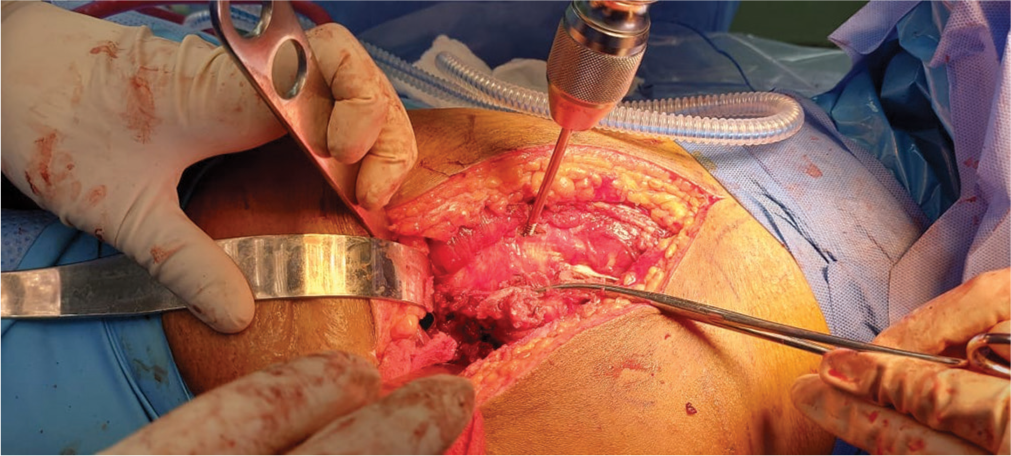
- Intraoperative image Kocher-Langenbeck approach to the right hip shows gluteus maximus tendon held in the forceps ruptured from its femoral insertion.
Copious amount of wash by normal saline and then debridement of necrotic tissue of short external rotators with reattachment of remnant tissues to its’ insertion, gluteus maximus tendon sutured to the femur at its’ footprint near to the origin of the vastus lateralis using vicryl suture size 2 mm. Drains were applied and water seal closure of the tensor fascia lata, followed by an approximation of the gluteus maximus muscle belly completed by the subcutaneous layer and skin closure.
The postoperative course with daily serial examinations showed the same as preoperative findings, with lower-limb power of 2/5 and intact sensation. Ankle foot orthosis was recommended and applied for the right foot drop, and physical therapy was started [Figure 7].
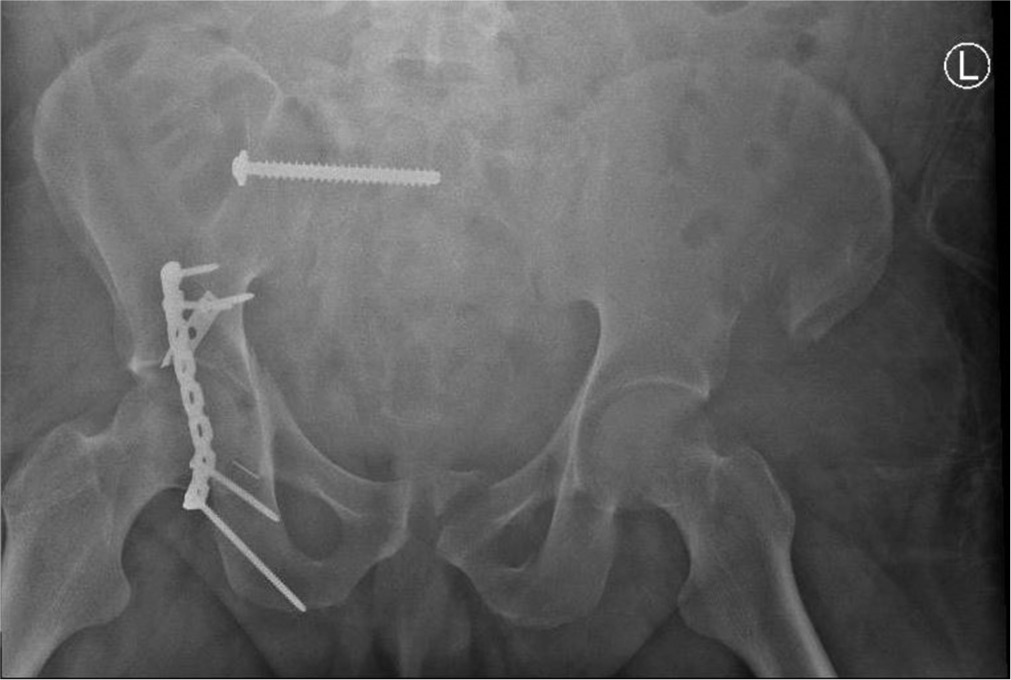
- Postoperative AP pelvis radiograph shows fixation of the right sacrum screw and right hip posterior wall with spring plate, buttress plate, and capsular fixation to the ischium through anchor suture.
In the fourth week post-operation, the patient started to develop spikes of fever, and the laboratories showed elevated levels of C-reactive protein (220), erythrocyte sedimentation rate (99), and white blood count (18,000) and the CT scan finding showed localized collection in the right gluteal medius muscle.
The patient was taken for irrigations, debridements, and three tissue and bone cultures with intraoperative findings showed a 1 cm short segment of surgical wound dehiscence, subcutaneous superficial serous collection around 30 mL, and some devitalized tissues with pale-colored gluteus maximus that was not contractile with electrocautery. The results of cultures were positive for Klebsiella pneumonia and Pseudomonas aeruginosa treated according to drug sensitivity by intravenous and ciprofloxacin for six weeks as advised by infection control. Wound condition and inflammatory markers improved after debridement and antibiotics course as the infectious disease department.
The patient was discharged home after his vitals and inflammatory markers normalized around four months after hospitalization with follow-up at the outpatient clinic four weeks after discharge. He was seen at the outpatient clinic. His examination showed limitation of hip extension and abduction range of motion, possibly due to hip muscle weakness or no compliance with physiotherapy, knee stiffness or lack of motion.
The patient was referred to physiotherapy for an aggressive rehabilitation program and instructed to comply with regular follow-up monthly for assessment of progression.
The last follow-up was seven months after the initial injury. The patient came walking with limping (short, flexed leg and foot drop). He had no significant pain, and no extension hip range of motion; his flexion was 20–80° and flexion power of 4/5, rotation of almost 20–25° with a power of 3/5, and abduction/adduction range of 20° power of 4/5. The foot drop remained the same, and there was significant improvement in peroneal sensation distribution.
His radiographs showed a healed fracture with extensive heterotopic ossification [Figure 8].
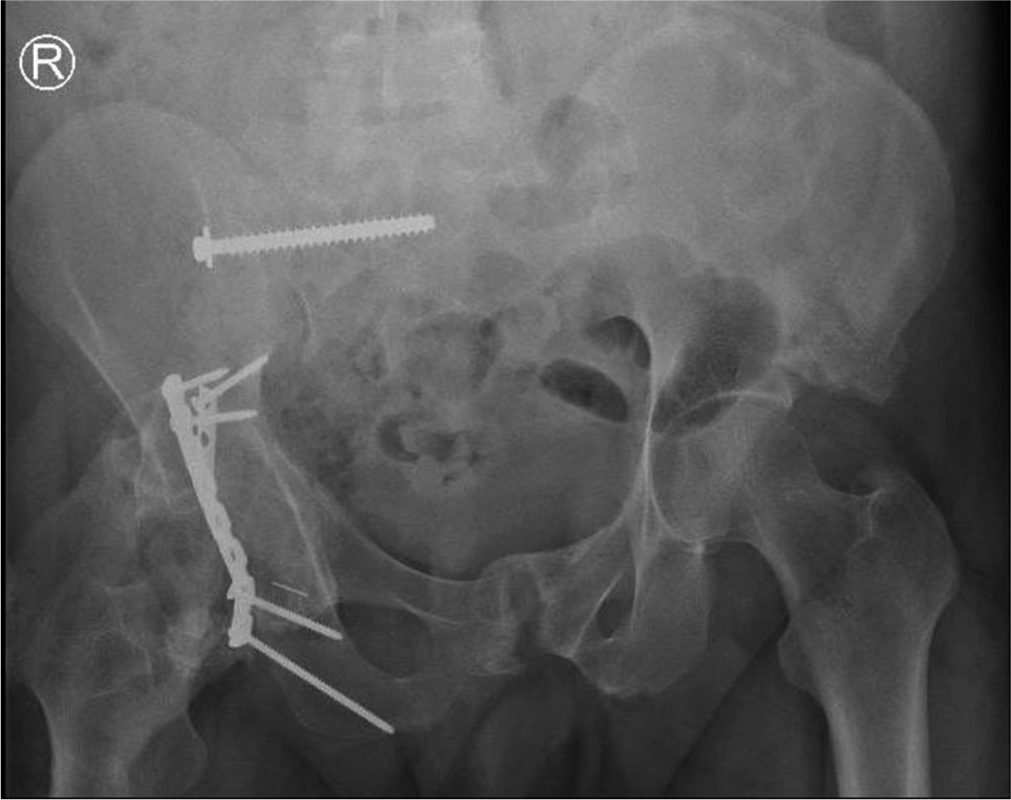
- The last visit seven months post fixation AP pelvis radiograph shows healed fractures of the left ilium, pubic rami, and symphysis pubis, healed right acetabulum posterior wall fracture with extensive heterotopic ossification.
The risks and benefits of heterotopic excision were offered to the patient. He agreed to proceed with surgical intervention after six months if the bone scan result and laboratory investigations were within normal limits.
DISCUSSION
After reviewing the literature on EMBASE, PubMed, and Google Scholar, we found limited literature on gluteus maximus tendon tear injuries. In a case reported by Alradwan and Youssef,[3] the patient complained of significant functional disability as well as severe pain after the gluteus maximus tear. The tear was partial and underwent surgical repair. The patient tolerated the surgery well, and the postoperative physiotherapy protocol was to protect weight-bearing and range of motion of the affected hip and knee and avoid extension for six weeks. After that, he started active extension. In their case, the tear was simple and not complicated with traumatic hip dislocation, posterior wall fracture with multiple fractures, and prolonged hospitalization, which may affect the surgical outcome as in our case.
Cormier et al.,[4] a retrospective data collection from orthopedic surgeons practicing in France and listed in the 2002 French Society for Orthopedic Surgery directory as regularly performing hip surgery reported six cases of gluteus maximus tear, five of them after total hip replacement, and one after a fall. All the cases were symptomatic with pain and weakness and diagnosed intraoperatively. They underwent surgical repair with excellent outcomes post-operation. This retrospective article is based on a survey emailed to involved surgeons with no precise data on the postoperative protocol as well as no intraoperative data for type and the site of the tear, whether it was a muscle fiber or an insertional tear.
Kara et al [5] reported one case of an elderly man complaining of traumatic gluteus maximus tear and sciatica after a fall. The patient was treated conservatively with rest, analgesics, and immobilization, efficiently relieving his symptoms. In this case, they did not mention the tear pattern, size, and physical therapy, which was insufficient to compare with our case.
Trauma could be identified by its direction, magnitude, and effect. Hip dislocation is rarely involving gluteus maximus tendon tear. Mayer et al.[6] reviewed the MRI findings of 15 patients with traumatic hip dislocations. No injuries to the hip abductor tendons were described. These studies corroborate the rarity of the associated lesions described in the current report.
Moorman et al.[7] described the mechanism and clinical and radiographic findings of eight American football players, who sustained a traumatic posterior hip subluxation.
They found abductors, short external rotator injuries, fractures, and sciatic nerve palsy. There were no documented cases of gluteus maximus tendon tear or avulsions in their series.
Diagnosis of gluteus maximus tendon tear might be difficult before surgical inspection with a need for proper instrumentation and training to deal with a variety of injuries. Although the treatment might be achievable, unfortunately, with the huge amount of energy causing trauma, healing might be associated with a difficult pathway ranging from dehiscence to infection and possible irreversible nerve injury or heterotopic ossification.
Further, attention in radiological studies before operative planning and readiness of all needed setups might help improve severely traumatized patients’ results. The patient and his relative must be explained about the extent of the injury and the expected prognosis.
CONCLUSION
Traumatic gluteus maximus tear with posterior hip dislocation is rarely reported injury in the literature. Considering the severity of the trauma with possible hip muscle tear, smoking, and prolonged hospitalization can lead to further complications.
It is a must to instruct and advise the patient postoperatively to be strictly compliant with physiotherapy sessions. Indomethacin or a small radiation dose is advised to decrease the risk of heterotrophic ossification in severely traumatized patients.
Further, attention in radiological studies before operative planning and readiness of all needed steps will help to improve the results and increasing the awareness of such pathology can help with early detection and management of gluteus maximus tear and prevent complications.
ACKNOWLEDGMENT
We want to acknowledge the Department of Orthopedics in KSMC for their support in the process of writing, reviewing, and publishing this paper.
AUTHORS’ CONTRIBUTIONS
HAA contributed to designing the study outlines. AYA did the literature review, primary draft writing, and re-writing the final draft. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICS APPROVAL
The Institutional Review Board approval is not required.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Surgical exposures in orthopaedics: The anatomic approach In: Illustrations by Hugh A. Thomas. Description (5th ed). Philadelphia, PA: Wolters Kluwer; 2016.
- [Google Scholar]
- Gluteus maximus partial tear: A case report. J Musculoskelet Surg Res. 2022;6:238-41.
- [CrossRef] [Google Scholar]
- Gluteus tendon rupture is underrecognized by French orthopedic surgeons: Results of a mail survey. Joint Bone Spine. 2006;73:411-3.
- [CrossRef] [PubMed] [Google Scholar]
- Gluteus maximus muscle tear as a rare cause of hip pain and sciatica. J Emerg Med. 2015;49:705-6.
- [CrossRef] [PubMed] [Google Scholar]
- MRI as a reliable and accurate method for assessment of posterior hip dislocation in children and adolescents without the risk of radiation exposure. Pediatr Radiol. 2015;45:1355-62.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic posterior hip subluxation in American football. J Bone Joint Surg Am. 2003;85:1190-6.
- [CrossRef] [PubMed] [Google Scholar]






