Translate this page into:
Upper limb spasticity surgery in adults: What we learned in 5 years of practicing it
2 University of Central Lancashire, Larnaca, Cyprus
3 Manchester Hand Centre, Salford Royal NHS Foundation Trust, Manchester, UK
4 Luton and Dunstable Hospital NHS Foundation Trust, Luton, UK
Corresponding Author:
Constantinos Kritiotis
Iasis Private Hospital, 8 Voriou Ipirou Street, 8036, Paphos
kritiotis@gmail.com
| How to cite this article: Kritiotis C, Tryfonidis M, Mishra A, Raja H. Upper limb spasticity surgery in adults: What we learned in 5 years of practicing it. J Musculoskelet Surg Res 2019;3:75-84 |
Abstract
We have been practicing surgical management of adult upper limb spasticity for the past 5 years. So far, we have evaluated 20 patients, and we have operated on nine patients with spasticity of the upper limb in Cyprus and the United Kingdom. We aim to present the setup and running of a new service, which is devoted to Surgery for Spasticity of the Upper Limb. We present our structure, organisational processes and service provision as well as our results in the nine cases that had surgical treatment as a part of their management (as well as our preferred techniques). We discuss our outcomes as well as our learning points from these cases. We also believe that selective neurectomy procedures can be very useful in the surgical management of upper limb spasticity. Tendon transfers to augment finger extension have a limited role and provide no significant benefits in adult spasticity cases. In addition, we found that the extensor carpi ulnaris transfer to extensor carpi radialis brevis has in our experience, reliable results regarding concentric wrist extension as well as easier rehabilitation. Furthermore, in severe cases, where no functional improvement is expected, joint fusions have a more predictable outcome. Spasticity reduction surgery does gain ground with the increase in survival of stroke patients as well as traumatic brain injury patients. Therefore, up to date methods for assessing, operating and evaluating postoperatively this category of patients need to be vigorously checked.Introduction
Spasticity of the upper limb due to a cerebrovascular incident (ischaemic, traumatic or haemorrhagic) may be a debilitating condition with multiple sequelae such as muscle tightness, joint stiffness, musculotendinous unit and/or joint contractures and joint deformities.[1] It may lead to the development of a number of troubling issues for patients, such as:
- Hygiene problems
- Functional abnormalities due to no use or spastic paralysis of the upper limb
- Posture derangement due to the abnormal positioning of the upper limb
- Pain.
Nonsurgical treatment methods may be used at the initial stages of spasticity development, usually in combination. These include regular physiotherapy, splinting with orthotic devices, muscle relaxant agents (such as Baclofen) or targeted botulinum toxin injections.[2],[10]
The surgical treatment for upper limb spasticity and its sequelae may be considered after at least 1 year has elapsed after the time of brain injury, after conservative treatment has failed and when no further neurological recovery is expected.[15] Surgical treatment options include (a) soft-tissue surgery such as muscle or tendon lengthening, tendon transfers[3] and selective[4] or hyperselective[5] neurectomies or (b) bone/joint surgery such as joint fusions or bone excisions,[1] such as proximal row carpectomy (PRC). There may be a need for a combination of a number of the above categories of surgical techniques. Operative treatment is irreversible, and the results are permanent. Operative treatment aims to decrease, eliminate or redirect muscle forces, mobilise stiff joints, restore balance to joints or stabilise joints, but it will not restore voluntary control to muscles or increase muscle force generation.[1] A similar concept of surgical treatment for upper limb spasticity is also used in cases of incomplete spinal cord injuries, but with a more advanced target of achieving a normalised pattern of grip as well as achieving an ergonomic manner of arm and shoulder work.[7]
Our main practice is based at the Republic of Cyprus, an island located in the Eastern Mediterranean. There are approximately 1000 acquired cerebrovascular incidents per year in the adult population. A significant percentage of those patients will go on to develop hemiplegic spasticity, which will alter their way of life. There is a great need for a holistic provision of spasticity care to these patients, including specialised upper limb surgical treatments when indicated, targeting towards improving the quality of life of these patients. The lead author also practices part time as a Consultant Hand Surgeon in the U. K. where he is involved in surgery of the spastic upper limb as well.
We present our experience and results in nine spasticity-reduction procedures that we carried out on nine patients, and we discuss our outcomes as well as our learning points from these cases. These patients were referred to our service either by rehabilitation doctors, physiotherapists or were self-referred.
Materials and Methods
Setup of service
Patients were either self-referred or referred by their rehab team. Assessments we carried out using an in-house protocol.
Pre-operative assessments
We developed an in-house protocol for each patient [Table - 1], which includes the following:
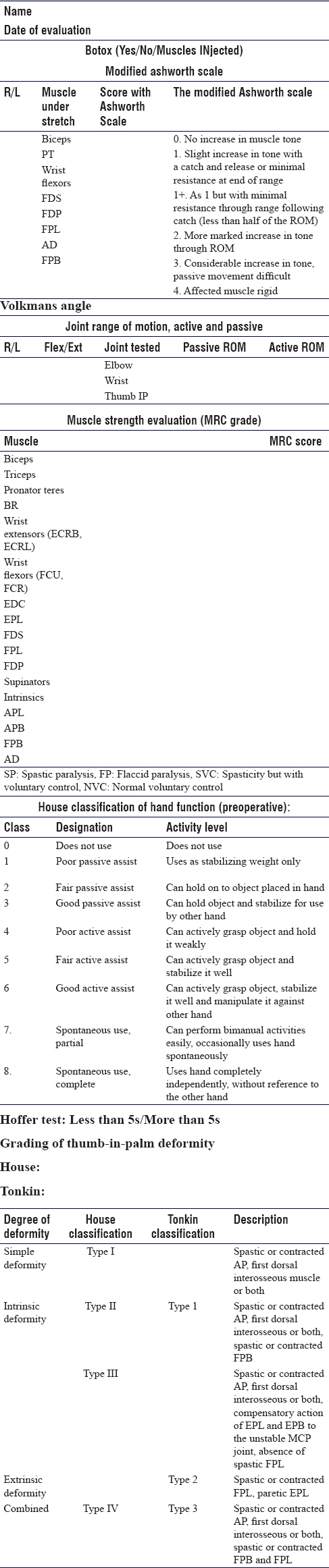
- Ashworth scale for spasticity
- The classification of thumb in palm deformity
- Medical Research Council grade of each muscle strength
- Hoffer test
- The evaluation of each individual muscle regarding its functionality (spastic, contracted, functional and flaccid).
Our outcomes regarding the functional improvement were measured using the House scale but as a part of continuing service development, we have introduced the Canadian Occupational Performance Measure (COPM),[8] which is a valuable tool in defining treatment priorities for individual patients and assessing the efficacy of intervention for that patient, both from a surgeon's and therapist's perspective as well as from the patient's perspective.
Description of some of the surgical techniques used
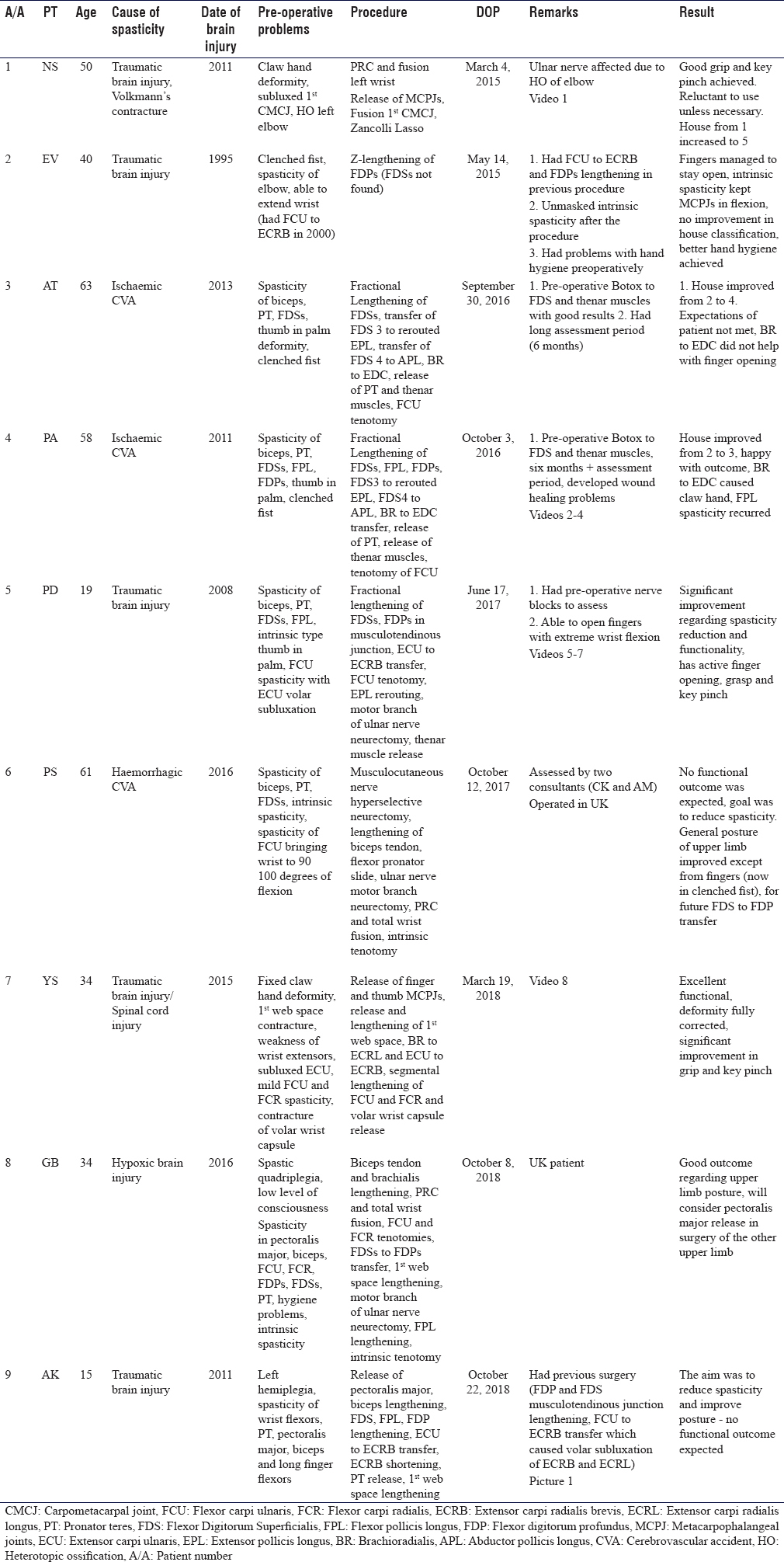
[Table - 2], [Table - 3], [Table - 4] provide a summary of the patient cases, description of the deformities tackled with surgical treatment and correction results following surgery. In the following paragraphs, we describe the main surgical techniques utilised for the patients' treatment. The techniques employed were mainly dependent on surgeons' preference, and this was based on training, experience and published literature when applicable.
The anaesthesia method in all the patients that we operated on was general anaesthesia with no peripheral nerve blocks.
All cases were operated as single stage, multilevel procedures.
Pectoralis major release
We employed a rather simple approach for spasticity of the pectoralis major. We carried out this procedure when abduction and external rotation of the shoulder could not be passively achieved. Spasticity of this muscle can cause adduction and internal rotation deformity of the shoulder. Clinically, spasticity of this muscle can be confirmed from the reduced external rotation of the shoulder in the abducted position, but most importantly, from the taut musculotendinous unit evident at the anterior axillary fold. In our approach, we use an L-shaped incision with the long limb of the L being directly over the taut pectoralis major tendon [Figure - 1]. We sharply elevate the skin flaps off the musculotendinous unit and then utilise a z-plasty to elongate it until a significant correction of the internal rotation and abduction deformity can be observed. We find this to be the simplest, less technically demanding and less time-consuming procedure that can be employed for spasticity of the shoulder muscles. Postoperatively, the patient has to have the upper limb in abduction during rest but no abduction splints are utilised. In our limited series, the one patient that we carried out this procedure on did not develop any hygiene or other problems in the region of his axilla.
 |
| Figure 1: Incision used for pectoralis major release |
Biceps lengthening
In our series of patients, we employed the commonly used Z-lengthening technique of the biceps tendon.[9] We used it in three patients, none of whom had functional elbow flexion.
Brachioradialis to extensor digitorum communis transfer
This technique was used in two ischaemic stroke patients. The patient pre-operative upper limb function was clinically assessed with the elbow in resisted active flexion and neutral position. In this technique, the brachioradialis is elevated from its attachment to the radial styloid and mobilised all the way to the elbow, to increase its excursion up to 4 cm. It is then weaved in the extensor digitorum communis (EDC) in a side-to-side fashion and secured with 2.0 running Ethibond suture. Tension is set with the tenodesis effect. In our series, it failed to lead to the expected outcome (which was to augment the opening of the hand), although there may be a role in cerebral palsy patients with a very weak EDC.[10]
Total wrist fusion with proximal row carpectomy
In two patients, we used the AO locking wrist arthrodesis plate (short bend), and in a third patient, we used the Medartis locking plate (straight wrist arthrodesis plate). In all patients, we also performed a PRC. We use the standard technique as advocated by AO. In all patients, the fusion improved the posture and stability of the wrist. This technique should be considered in non-functional hands and in patients with severe contracture of the wrist joint, where a tendon transfer will not adequately power enough the radial wrist extensors.[11]
1st Carpometacarpal joint fusion
This technique is used in patients with instability of the joint and can also be used in patients with severe thumb-in-palm deformity. In this technique, the articular surfaces of the 1st carpometacarpal joint (CMCJ) are prepared, and a locking 2.0 t-plate can be used. The joint is fused in about 30° of extension and 30° of abduction so as for the thumb tip to pinch against the middle phalanx of the index. It can be combined with 1st web space lengthening. We believe that it has a place in elderly, post-ischaemic stroke patients as well.
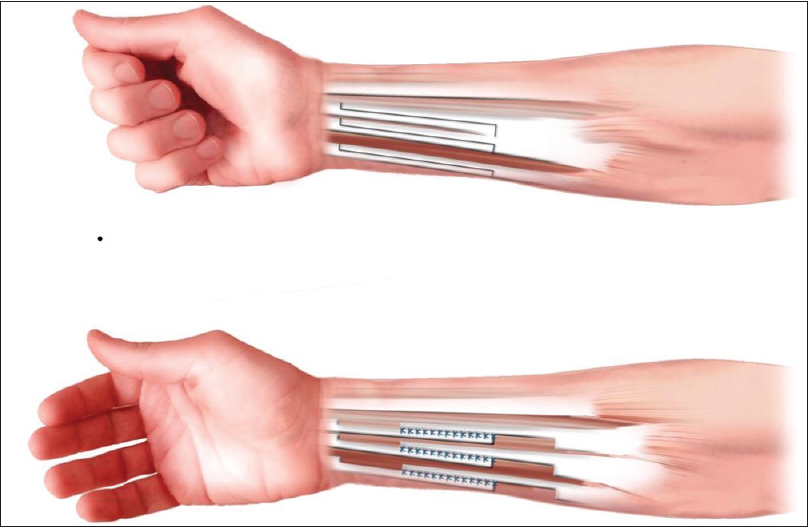
Extensor carpi ulnaris to extensor carpi radialis brevis transfer for wrist extension
This is our preferred method for achieving active wrist extension in spasticity patients. Usually, in spasticity patients, the extensor carpi ulnaris (ECU) is displaced volarly and despite being active, can contribute to the flexion deformity of the wrist [Figure - 2]. One can identify the patients with the subluxed ECU from the hyperflexed and ulnarly deviated wrist. In this technique, the ECU is divided proximal to the subsheath in the Distal Radioulnar Joint; its muscle belly is mobilised and then weaved to the extensor carpi radialis brevis (ECRB).[14] This follows usually a segmental lengthening of both the flexor carpi ulnaris (FCU) and the flexor carpi radialis as well as release of the volar wrist capsule. We aim to keep the wrist in neutral when setting the tension and then the side-to-side weave is completed with a 2.0 Ethibond suture.[14] We believe it to be more predictable than the FCU to ECRB as the FCU is often found contracted. In addition, we do believe that rehabilitation will be easier as both donor and recipient are extensors and hence in-phase.
 |
| Figure 2: Wrist in flexion and ulnar deviation. In this spasticity pattern, the extensor carpi ulnaris can be found subluxed volar to the midline, contributing to the flexion deformity of the wrist |
Pronator teres release
The pronator teres (PT) is spastic in the vast majority of spasticity patients. We prefer to use an incision over the radial aspect of the mid-forearm. The PT tendon insertion to the radius is identified in the interval between the brachioradialis and the extensor carpi radialis longus (ECRL), and it is sharply elevated with a 15-blade and periosteal elevator from the radial shaft. Then, the forearm is gently supinated until full supination is confirmed and the PT is retracted. We recommend release of the PT in all spasticity patients as we believe it to be a significant trigger of spasticity, although further research needs to be carried out to strengthen this point.
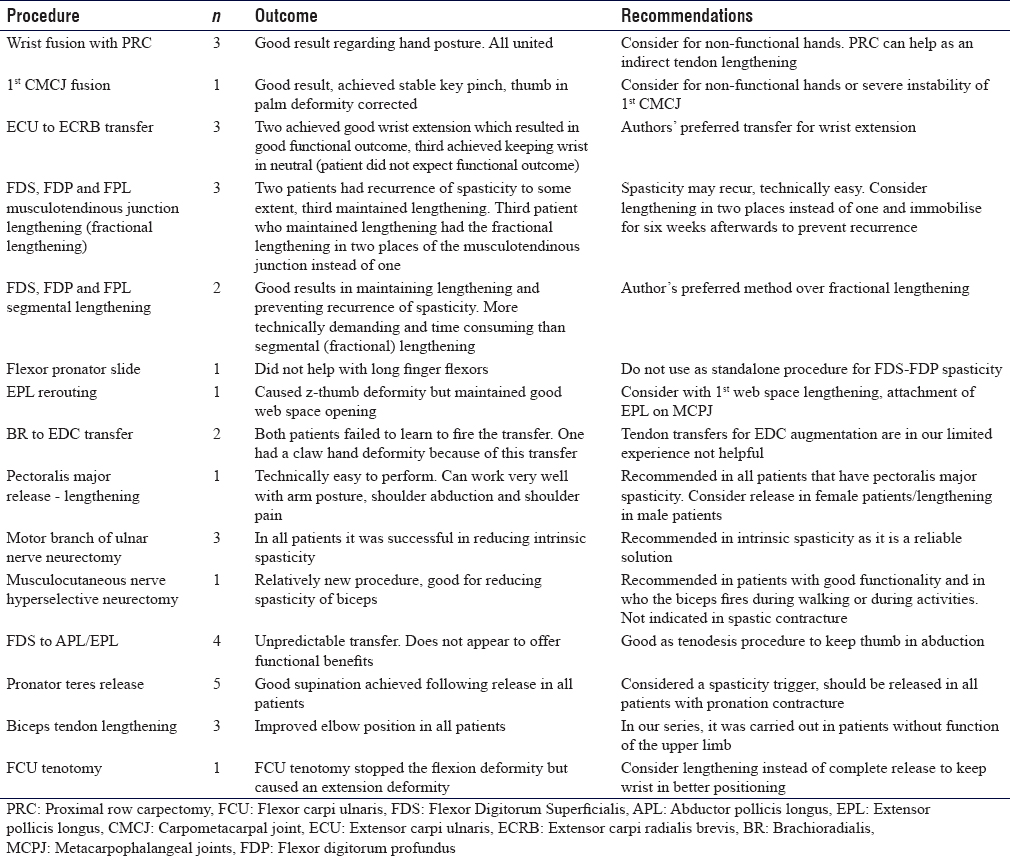
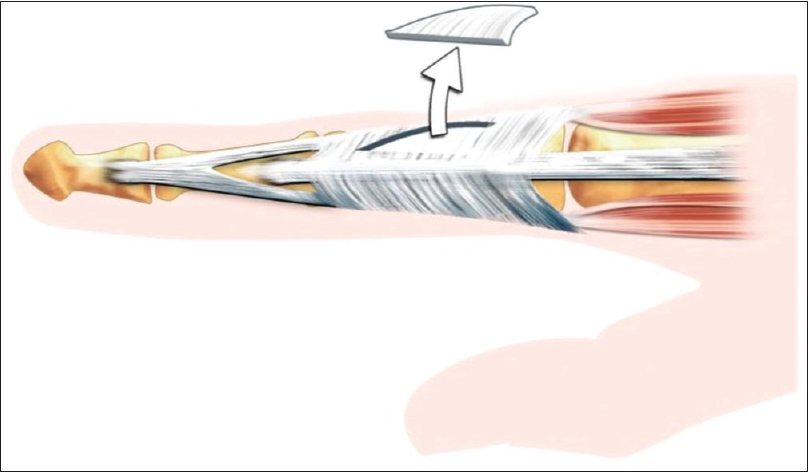
Long flexor tendon lengthening
We employed two methods in our series. The first method was the musculotendinous junction lengthening (or otherwise known as 'shark attack'). In this method, the tendon is cut in its origin, and then the finger is stretched, thus elongating the muscle/tendon unit. The other is to perform Z-lengthening of the flexor tendons and then a side to side repair [Figure - 3], reproduced by permission[7]]. This method is more technically demanding and more time consuming than the 'shark attack' however, it has a lower rate of spasticity sequelae recurrence than the shark attack.
 |
| Figure 3: Segmental lengthening of long finger flexors (image reproduced with permission from Carina Reinholdt) |
Motor branch of ulnar nerve neurectomy
In this technique, a standard Guyon's canal decompression is used in the hypothenar area of the palm, between the hook of the hamate and the pisiform.[6] Care must be taken not to mistakenly enter the carpal tunnel instead of the Guyon's canal. Following that, the ulnar artery is gently retracted and protected and the adductor fascia is divided. Then, the motor branch of the ulnar nerve is identified as it crosses around the hook of the hamate. It is divided with electrocautery at this level. We believe that this is a very reliable technique when there is significant intrinsic spasticity as well as adductor and 1st dorsal interosseous spasticity. We use this technique in total non-functional contracture of both the intrinsic muscles as well as the adductor pollicis.
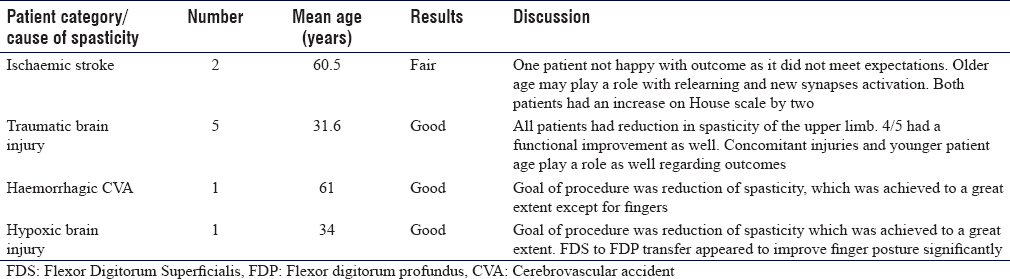
Intrinsic release
When we have patients with significant contracture of the intrinsics, we use a lazy-s incision over the dorsum of the finger, and we excise a triangular piece containing the lateral band and the oblique fibres, as advocated by Reinholdt and Fridén [Figure - 4], reproduced with permission].[15]
 |
| Figure 4: Technique used for intrinsic spasticity (image reproduced with permission) |
Post-operative evaluation
We evaluate all patients with the House scale. As mentioned above, with the development of the service, we introduced also the COPM. In addition, all patients have pre-operative and post-operative video evaluations to assess the improvement [Video 1],[Video 2],[Video 3],[Video 4],[Video 5],[Video 6],[Video 7],[Video 8].
Discussion
Patient groups and our recommendations
Patients with spasticity of the upper limb are a very challenging and constantly increasing population. In our population, we found that the demands for surgical treatment in upper limb spasticity are increasing with the spread of knowledge and surgical skills. We operated on four main categories of patients: (1) post-traumatic brain injuries, (2) patients following ischaemic stroke, (3) patients following haemorrhagic stroke and (4) patients following hypoxic stroke [Table - 4]. We did not include children with cerebral palsy in our study.
The majority of patients (five patients) that we operated on were sequelae from post-traumatic brain injuries. All patients required a number of consultation sessions, both not only for the surgeon to establish the patients' condition, disabilities, demands and expectations, but also for the patients and families to be counselled on the purpose of each proposed procedure, potential benefits and to agree on realistic target for surgical treatment. Pre-operative botulinum toxin injections or peripheral nerve blocks should be used to distinguish muscles with spastic contracture from muscles that have an increased tone but no contracture (and could be therefore used for a tendon transfer, like the FCU). The two ischaemic stroke patients received botulinum toxin injections approximately 6 months before their procedures to the FCU, Flexor Digitorum Superficialis (FDS) and thenar eminence. Patient PD received peripheral nerve block of the ulnar nerve (both in the cubital tunnel and the Guyon's canal) to evaluate his response to a possible motor branch ulnar nerve neurectomy [Video 6] and [Figure - 5].
 |
| Figure 5: Patient PD following peripheral nerve block injections of the ulnar nerve. Notice the improved posture of the thumb and the finger metacarpophalangeal joints |
In this patient series, we observed that patients following traumatic brain injuries composed the most varied population regarding their disability. The concomitant injuries (untreated fractures and dislocations, heterotopic ossification, spinal cord and brachial plexus injuries) have a significant impact on the way the deformity appears and therefore must be taken into consideration before the surgical procedure. In addition, the severity of the brain injury, even though it was not studied in our series, does appear to play a part in the severity of the spasticity. In our series, the best outcomes (both regarding function and spasticity reduction) were observed in this category of patients, and therefore, their younger age and possibilities for neurological recovery do play a significant part. Because of all these reasons, the spasticity pattern is different in each of these patients.
Ischaemic stroke patients should be considered a different category. They belong to a more senior age group (usually in their 7th decade of life), and they usually have significant comorbidities. Both patients with ischaemic stroke in our series suffered from a similar pattern of spasticity [Video 2]. More specifically, they had spasticity of the PT, the FCU and the long finger flexors (predominantly), as well as spasticity of the thenar muscles. No intrinsic spasticity was noted in any of the two patients. Both had totally absent EDC. Both were able to grasp but not to release. The results in our series were good regarding the reduction of spasticity but not regarding functional improvement, although on the House scale, they gained two points. Therefore, we recommend surgery for post-ischaemic stroke patients only when they had spasticity related hygiene problems or posture problems of the upper limb.[16] In addition, even though the idea of an augmenting tendon transfer for digital opening may sound tempting, due to the fact that these patients are difficult to retrain and also because they may have paretic intrinsics, it is not something that we would recommend.
Patients with massive haemorrhagic strokes may appear either with spastic hemiplegia or quadriplegia. Again, for this category of patients, we recommend surgery only for the purposes of reduction of spasticity. We do not recommend surgery for functional improvement, and any operative treatment should aim for a better posture of the upper limb, both for hygiene and daily care purposes.
Patients with hypoxic brain injury (e.g., post a prolonged cardiac arrest) have a diffuse pattern of brain injury and very often suffer from spastic quadriplegia. Again, we would not recommend surgery for functional improvement but rather for the reduction of spasticity and a better posture of the upper limb, which will help with the overall rehabilitation.
The procedures that we used and our recommendations
As we presented above [Table - 3], we used joint fusions, tendon transfers, tendon releases, tendon lengthening, selective neurectomies and joint fusions[13] in our series. Based on our outcomes, we have the following recommendations:
Tendon transfers
We are very much in favour of the ECU to ECRB transfer.[17] In our experience, it works very well, and it is an easily trainable tendon transfer (extensor for extensor). Furthermore, as the ECU is in the majority of the patients dislocated volarly (and therefore acts as a flexor) the deforming force is converted to a correcting force. We also believe that it is a more reliable transfer than the FCU to ECRB (Green's transfer), as the FCU is frequently severely contracted with absent voluntary control. Further research needs to be carried out to strengthen this point, but in our series, all ECU to ECRB transfers worked well. Should the surgeon wish to use the FCU, either for powering the wrist extensors or the finger extensor, a meticulous pre-operative examination should be carried out and also, the use of a motion laboratory should be mandatory to distinguish the spastic contracted FCU from the FCU that has an increased tone. We do believe that further research needs to be carried out to evaluate the superiority of ECU to ECRB transfer over the FCU to ECRB transfer.
We believe that the brachioradialis to EDC is not a reliable transfer for ischaemic stroke spasticity patients as it may either not work or create a claw hand deformity [Figure - 6]. Our results with the use of this transfer were not satisfactory, despite meticulous pre-operative clinical examination and evident function of the brachioradialis. However, we would recommend it for augmentation of wrist extension by transferring it either to the ECRL or the ECRB. We did transfer it to the ECRL of a patient with very weak wrist extensors (we also transferred the ECU to the ECRB), and the patient went on to achieve a very good extension of the wrist [Video 8].
 |
| Figure 6: Secondary extension deformity of MCPJs post-brachioradialis to extensor digitorum communis transfer. This prevents the patient to wrap his hand around an object and achieve a stable grip |
The FDS III-IV to the Abductor Pollicis Longus and Extensor Pollicis Longus can in the worst scenario, create a good tenodesis for the thumb to keep it in abduction and extension; therefore, it can be considered in patients with severe thumb in palm deformity and no active EPL. However, care should be taken for possible wound healing problems (we had one in our series) if the transfer is very taut.
Finally, we recommend the FDS to FDP transfer for non-functional hands. In our practice, we buddy all the FDSs tendons and all the FDP tendons in one unit (making sure that the finger cascade is maintained) and then weave the FDS unit through the FDP in a side-to-side fashion.[12]
Tendon releases/lengthenings
We believe that a spastic pronator quadratus must always be released. However, for the remaining spastic muscles, we recommend instead of releasing them to lengthen them. This will lead to a more balanced appearance of the affected joint(s) and preserve function if these muscles are active (like the long finger flexors).
Joint fusions
In our series, we fused one 1st CMCJ and three radiocarpal joints. Two out of the three radiocarpal joints fusions had non-functional hands, and the aim of the surgery was a better posture of the upper limb. We always combine this procedure with a PRC. All three cases of radiocarpal fusion united and the patients were happy with the posture of their hand. One of them had a functional improvement as well. Surgeons must take into account the fact that severity of the long finger flexors spasticity will cause the fingers to dig in the palm when the wrist is fused in the extended position. We therefore recommend fusion in neutral position (using a straight wrist fusion plate)[11] and in non-functional hands to perform also an FDS to FDP transfer.[13]
The 1st CMCJ fusion was carried out in a traumatic brain injury patient with a traumatic dislocation of the 1st carpometacarpal joints, which was left untreated [Video 1]. It resulted in him getting a stable pinch and better posture of the hand. When carried out, we recommend also complementing it with a 1st web space lengthening.
Selective neurectomies
We only performed one motor branch of the ulnar nerve neurectomy in the Guyon's canal in a traumatic brain injury patient with severe spasticity of the intrinsics and the adductor pollicis.[4] Before performing the neurectomy, we did a peripheral nerve block of the ulnar nerve in the Guyon's canal to assess the functional improvement. We were very satisfied with the outcome as the patient did not develop a claw hand deformity and was able to perform a gross grip following the procedure [Video 6] and [Video 7]. Therefore, we believe that the indication for the motor branch of the ulnar nerve neurectomy is severe spasticity of the intrinsic muscles of the hand which may not improve by lengthening alone.
We also carried out a musculocutaneous nerve neurectomy in a post-haemorrhagic stroke patient with a severely contracted biceps (on which we also carried out a Z-lengthening of the biceps tendon).[5] We believe that this neurectomy has a role in an upper limb with a functional biceps to reduce the tone of the affected biceps and allow for function. However, we believe that it is not needed in patients who have a spastic and contracted biceps as it will not release the contracture. In these patients, with contracted non-functional biceps, we strongly recommend the Z-lengthening of the biceps tendon.
Conclusion
We have presented our early experience and results in a newly established service in the Republic of Cyprus for spasticity surgery for the upper limb in adults. The benefits as well as pitfalls of various techniques were analysed, and recommendations based on our experience were discussed. We did learn a lot of lessons during this process, and as our experience grows, our results will hopefully, continue to improve.
Lessons learned are the following:
- Use Patient-Recorded Outcome Measures (such as the COPM) to standardise and record outcomes
- Further research needs to be carried out on the relation of the mechanism of brain injury and the subsequent spasticity pattern
- We also recommend researching and publishing guidelines which will guide surgical treatment, based on:
- Type of brain injury
- Spasticity pattern, which will involve
- Spastic/contracted muscles
- Muscles with increased tone
- Active/functional muscles.
Ethical consideration
We have obtained the written consent of the patients for the publication of their outcomes and their photographic material. Our institutions gave us the approval to proceed with this publication.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Author's contribution
CK conceived and designed the analysis, collected and analysed the data and wrote the paper. MT participated in data collection and co-wrote the paper. AM and HR contributed in data collection. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Mikalef P, Power D. The rationale of operative treatment for spasticity of the upper limb. MOJ Orthop Rheumatol 2018;10:300-3. [Google Scholar] |
| 2. | Simpson DM, Patel AT, Alfaro A, Ayyoub Z, Charles D, Dashtipour K, et al. OnabotulinumtoxinA injection for poststroke upper-limb spasticity: Guidance for early injectors from a Delphi panel process. PM R 2017;9:136-48. [Google Scholar] |
| 3. | Fitoussi F, Bachy M. Tendon lengthening and transfer. Orthop Traumatol Surg Res 2015;101:S149-57. [Google Scholar] |
| 4. | Fouad W. Management of spastic hand by selective peripheral neurotomies. Alexandria J Med 2011;47:201-8. [Google Scholar] |
| 5. | Leclercq C, Gras M. Hyperselective neurectomy in the treatment of the spastic upper limb. Phys Med Rehabil Int 2016;3:1075. [Google Scholar] |
| 6. | Buffenoir K, Rigoard P, Ferrand-Sorbets S, Lapierre F. Retrospective study of the long-term results of selective peripheral neurotomy for the treatment of spastic upper limb. Neurochirurgie 2009;55 Suppl 1:S150-60. doi: 10.1016/j.neuchi.2008.04.003. [Google Scholar] |
| 7. | Wangdell J, Reinholdt C, Fridén J. Activity gains after upper limb surgery for spasticity in patients with spinal cord injury. J Hand Surg Eur Vol 2018;43:613-20. [Google Scholar] |
| 8. | Wangdell J, Fridén J. Rehabilitation after spasticity-correcting upper limb surgery in tetraplegia. Arch Phys Med Rehabil 2016;97:S136-43. [Google Scholar] |
| 9. | Mital MA. Lengthening of the elbow flexors in cerebral palsy. J Bone Joint Surg Am 1979;61:515-22. [Google Scholar] |
| 10. | Pinzur MS, Wehner J, Kett N, Trilla M. Brachioradialis to finger extensor tendon transfer to achieve hand opening in acquired spasticity. J Hand Surg Am 1988;13:549-52. [Google Scholar] |
| 11. | Neuhaus V, Kadzielski JJ, Mudgal CS. The role of arthrodesis of the wrist in spastic disorders. J Hand Surg Eur Vol 2015;40:512-7. [Google Scholar] |
| 12. | Hosalkar H, Pandya NK, Hsu J, Keenan MA. What's new in orthopaedic rehabilitation. J Bone Joint Surg Am 2011;93:1367-74. [Google Scholar] |
| 13. | Pomerance JF, Keenan MA. Correction of severe spastic flexion contractures in the nonfunctional hand. J Hand Surg Am 1996;21:828-33. [Google Scholar] |
| 14. | Fridén J, Tirrell TF, Bhola S, Lieber RL. The mechanical strength of side-to-side tendon repair with mismatched tendon size and shape. J Hand Surg Eur Vol 2015;40:239-45. [Google Scholar] |
| 15. | Reinholdt C, Fridén J. Selective release of the digital extensor hood to reduce intrinsic tightness in tetraplegia. J Plast Surg Hand Surg 2011;45:83-9. [Google Scholar] |
| 16. | Keenan MA. Management of the spastic upper extremity in the neurologically impaired adult. Clin Orthop Relat Res 1988; (233):116-25. [Google Scholar] |
| 17. | Trehan SK, Little KJ. Technical pearls of tendon transfers for upper extremity spasticity. Hand Clin 2018;34:529-36. [Google Scholar] |
Fulltext Views
7,099
PDF downloads
1,768





