Translate this page into:
Wagner technique for the treatment of recurrent femoral neck active unicameral bone cyst in a child: Expanding the indications
2 Department of Orthopedics, AlRazi Hospital, Kuwait Institute for Medical Specializations, Kuwait City, Kuwait
3 College of Medicine, University of Hail, Hail, Saudi Arabia
4 Department of Orthopedics, King Fahad General Hospital, Almadinah Almunawwarah, Saudi Arabia
Corresponding Author:
Abdullah M Alqaseer
Department of Orthopedics, AlRazi Hospital, Kuwait Institution for Medical Specializations, Kuwait City
Kuwait
dr.alqaseer@gmail.com
| How to cite this article: Aljuhani WS, Alqaseer AM, Alobaidi SA, Mohammed Aziz FA, Alshammari AN. Wagner technique for the treatment of recurrent femoral neck active unicameral bone cyst in a child: Expanding the indications. J Musculoskelet Surg Res 2020;4:156-159 |
Abstract
Unicameral bone cysts (UBCs) are common benign bone tumors in skeletally immature individuals. UBCs are considered active when found in close proximity to the growing physis. An active UBC of the femoral neck raises unique management challenges. This is due to its location in an area known to be high risk for complications if fractured, such as avascular necrosis and varus malunion. Transfixing the femoral neck physis while aiming to stabilize the fracture poses a risk of growth arrest. This risk is minimized when employing smooth Kirschner wires. Here, we present the case of a 5-year-old male with a recurrent active UBC in the left femoral neck complicated with a pathological fracture in which stabilization was achieved utilizing the Wagner technique of multiple Kirschner wires. To our knowledge, this technique has not been described in the treatment of such pathology.
Introduction
Unicameral bone cysts (UBCs) were first described as a distinct pathological entity by Mikulicz in 1906.[1] UBC is a very common benign bone tumor among children and adolescents.[2] UBCs, also commonly referred to as simple bone cysts, represent 3% of all benign bone tumors in patients younger than 20 years of age.[3] Among this population, 80% of all UBCs are found.[4] A UBC is considered latent when a bone of more than 5 mm separates it from the nearest physis and active if bone separation in <5 mm.[5] However, Haidar et al. defined a latent UBC as being at least 2 cm away from the physis and showed it to be a significant factor in the decrease rate of recurrence.[6] UBCs are managed using various treatment options. These include but are not limited to observation, injection of agents (such as steroids, bone marrow aspirate, demineralized bone matrix, or bone substitutes), and surgical intervention, which usually consists of curettage with or without internal fixation.[7] A proximal femoral active UBC carries a unique challenge for which a strong construct is needed to stabilize the fracture or impending fracture of the UBC with minimal violation of the physis to decrease the chance of growth arrest.
Wagner technique was described and reported for stabilizing intertrochanteric osteotomies to correct coxa vara in children. This technique was not reported in the literature as a method for the fixation of active femoral neck UBC with pathological fracture. Because of the studied benefits, this technique was utilized in the current case to minimize the risk of growth plate arrest.
Case Report
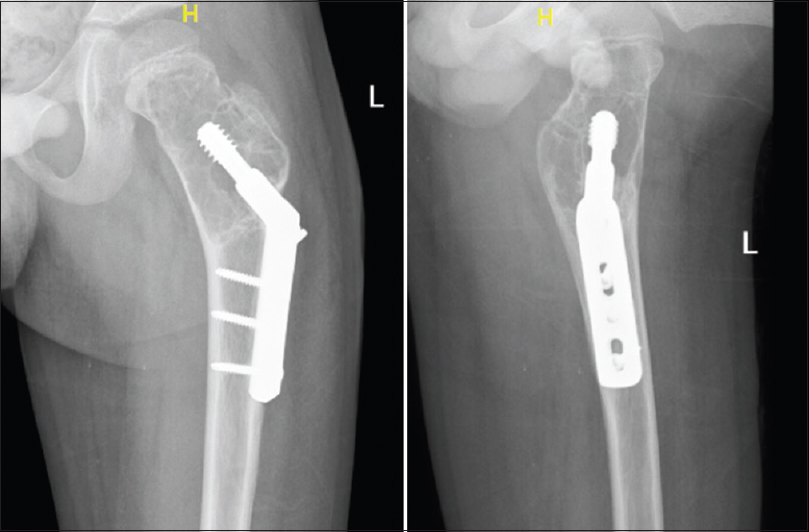
A 5-year-old male presented with pain in the left hip that prevented him from ambulating. He is known to have a bicuspid aortic valve with severe aortic valve stenosis. His examination was unremarkable except for guarding the left hip due to severe pain. A pelvic radiograph showed a centrally located lytic lesion within the left femoral neck, most likely representing UBC of the femoral neck complicated with a pathological undisplaced fracture of the femoral neck. Those findings were further confirmed with magnetic resonance imaging of the left hip [Figure - 1]. The patient was operated on with curettage, filling the defect with calcium phosphate bone substitute, and fixated with a pediatric dynamic hip screw (DHS) [Figure - 2]. Unfortunately, after 2 years of loss to follow-up, the patient presented again with severe hip pain limiting ambulation.
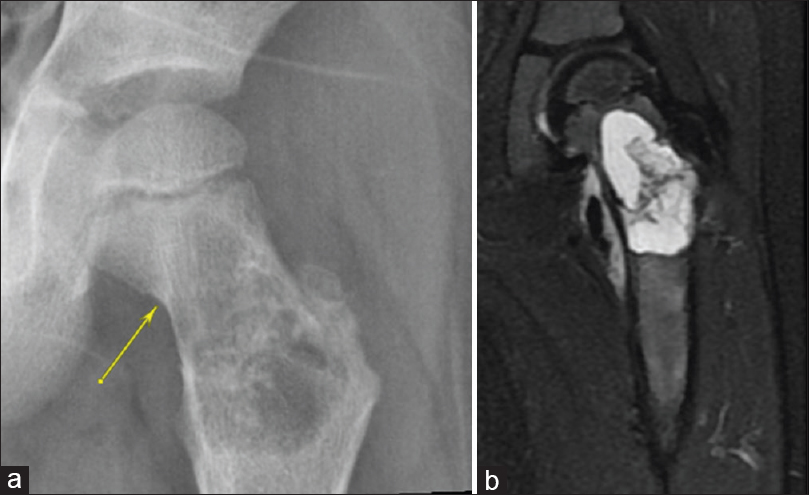 |
| Figure 1: (a) Anteroposterior view showing a central lytic lesion in the left femoral neck. The arrow indicates a fracture line through the cyst (b) Coronal T2 magnetic resonance imaging reconstruction of the left proximal femur showing homogeneous fluid-filled cyst of the left femoral neck |
 |
| Figure 2: Postoperative anteroposterior and lateral views radiograph of the left hip, showing the cavity filled with bone substitute and fixation by pediatric dynamic hip screw |
New radiographs of the left hip were requested and compared to the postoperative images and showed an expansile lytic proximal femoral lesion that had increased in size compared to the previous radiographs [Figure - 3]. Complete absorption of the bone graft was also noted. The minimal bone between the physis of the femoral neck and UBC suggested a still active UBC. A cortical breakthrough observed in the lateral aspect of the femoral neck, which was suggestive of a fracture line.
 |
| Figure 3: Two years postoperative images showing recurrence of the unicameral bone cyst with femoral neck fracture |
A computed tomography (CT) of the left hip was requested to confirm the existence of a pathological fracture and aid in surgical planning [Figure - 3]. The CT scan confirmed the suspicion of an undisplaced pathological fracture and showed the lesion extending to the physis with a thin layer of bone in between. The CT also showed that the pediatric DHS lag screw was floating in the middle of the cyst, with no bone purchase whatsoever. The patient was kept on strict nonweight-bearing orders and was admitted for cardiology clearance and operative intervention.
Operative technique
A pediatric fracture table was employed with the patient in the supine position with his contralateral lower limb flexed and abducted. Traction was not used. At this time, an intraoperative radiograph was obtained, and it was determined that there was a displacement of the femoral neck fracture. A closed reduction was necessary to achieve an acceptable position. A lateral incision was made over the previous surgical scar. We utilized a subvastus lateral approach. The DHS was removed, and that was followed by curettage of the UBC's inner surface through the hole of DHS's lag screw. The cavity was then filled with BIO 1-QUICKSET®, an injectable self-hardening bone substitute. Under image-intensifier control and using a power tool, five 2.0-mm K-wires were inserted as parallel to each other as possible, keeping in mind not to penetrate the hip joint. Using two K-wire pliers, the K-wires were bent as close to the bone as possible. Then, two 2.5-mm holes were drilled from the anterior to the posterior aspect of the femur. The first hole was approximately 2 cm below the lesser trochanter, and the two holes were about 2 cm apart. Two cerclage wires were passed through the holes and tensioned around the bent K-wires until the K-wires were lying entirely on the lateral aspect of the femur [Figure - 4].
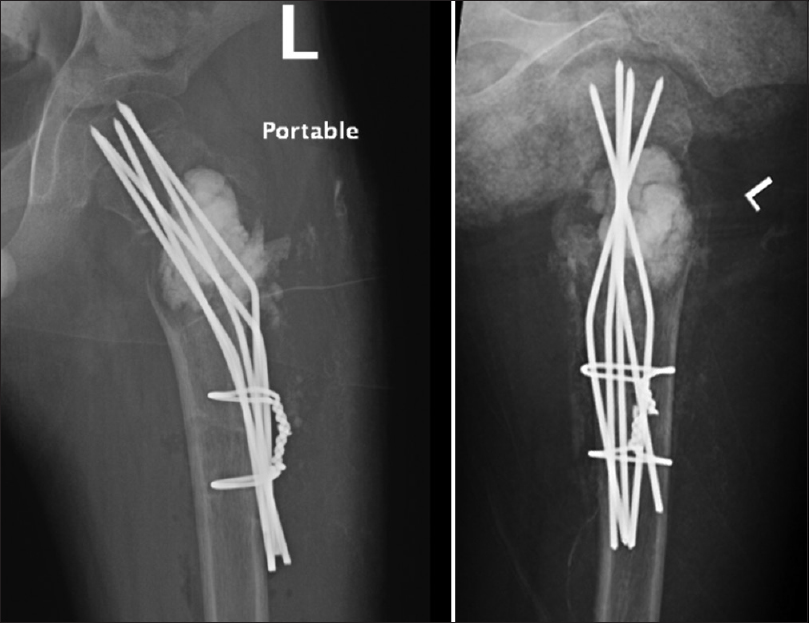 |
| Figure 4: Immediate postoperative views |
The patient was kept nonweight bearing postoperatively for 2 months. The signs of surgical site infection presented at the first follow-up in 2 weeks postoperatively, and it was successfully treated with a course of oral antibiotics. Follow-up radiographs at 2 months showed good bone healing, and the patient was able to bear weight with minimal discomfort and had a full range of motion of the left hip [Figure - 5] and [Figure - 6]. At 6 months, the patient had no new complaint and was walking without pain or limp, and there was no sign of recurrence or loosening on radiographs.
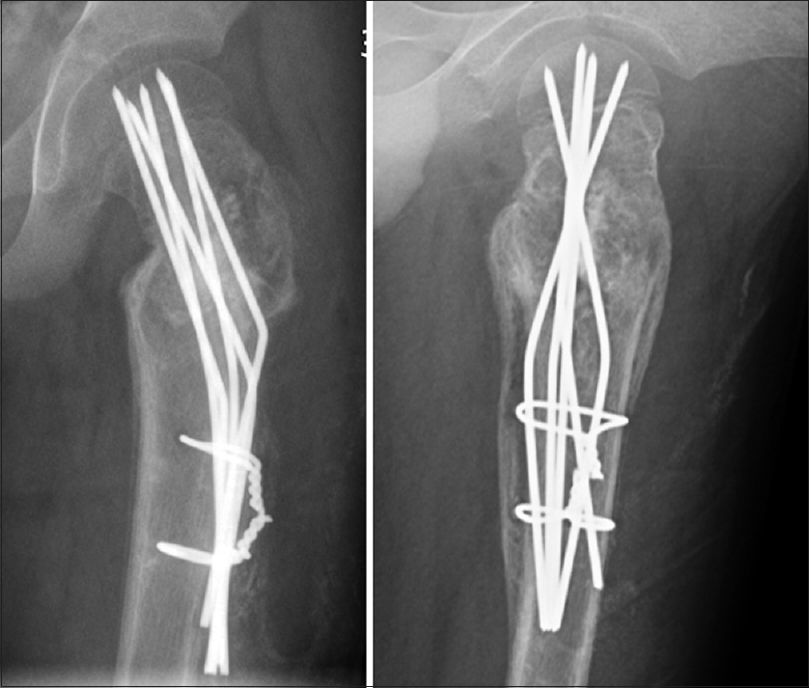 |
| Figure 5: Radiographs at 2 months after the surgery |
 |
| Figure 6: Clinical photographs at 2 months after the surgery |
Discussion
Our patient was diagnosed with having a recurrent active UBC with a fracture in the femoral neck. Given that he was a 5-year-old child, an attempt was made to achieve minimal injury to the growing physis. Transfixing the growth plate of the femoral neck with K-wires has been shown to carry a lower risk of growth arrest compared to other fixation modalities.[8],[9] A UBC of the proximal femur was even shown to cause coxa vara and avascular necrosis if not adequately treated.[10] Dormans described a classification system to guide the treatment of lytic lesions of the femoral neck. He classified type 2 benign lesions as those lying in close proximity to the physis and recommended fixation using K-wires.[11]
The fixation method used in this patient was first described by Wagner in 1978 when he used it to stabilize intertrochanteric osteotomies for the correction of coxa vara in children.[12] Widmann et al. studied over 17 valgus osteotomies using the Wagner technique, with an average age at surgery being 5.6 years, and the average follow-up was 4.5 years. Moreover, in their study, premature closure of the physis was observed in four of their 17 treated patients with the remaining hips physis remained open until the final follow-up.[13] They concluded that the Wagner technique is a stable fixation with minimal complications in treating patients suffering from coxa vara.[13] Because of the benefits, this technique was utilized in the current case to stabilize the already weakened femoral neck bone by the UBC with the minimal risk of growth plate arrest.
In our case, BIO 1-QUICKSET®, which is an injectable self-hardening bone substitute based on tricalcium phosphate (TCP), was used in both surgeries to fill the UBC cavity after curettage due to its high compressive strength and for its osteoinductive properties.[14] Many adjuncts were used in the literature in an effort to promote cyst healing and provide structural support by filling the cyst.[7] The UBC recurrence was shown by Zhang et al., to be related to the initial filing by the TCP, no recurrences were observed at 2 years of followup in cysts that were estimated to be filled 100% by TCP, which may partially explain the recurrence encountered after the first surgery.[15]
Conclusions
The clinical results indicate that using the Wagner multiple K-wire osteosynthesis technique is an option to stabilize an active UBC of the femoral neck in skeletally immature individuals. At the short-term follow-up, this fixation construct proved to be mechanically sound to allow for adequate cyst and bone healing. However, further studies are required with larger sample sizes and longer follow-up to confirm these findings.
Declaration of patient consent
The authors certify all appropriate patient consent forms were obtained. In these forms, the patient's parents gave consent for the use of his images and other clinical information to be reported in the publication. The patient's parents understand that his name and initials will not be published, and all efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
WSA, AMA, SAA, FAA, and ANA conceived and designed the study, conducted research, provided research materials, and collected and organized the data. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | von Mikulicz J. Cystic Degeneration of the Bones, Verhandl. d. Gesellsch. deutsch. Naturforsch. u. Aerzte 1906;76:107. [Google Scholar] |
| 2. | Marotexau P. Bone diseases of children. Philadelphia: Lippincott; 1979. p. 388-90. [Google Scholar] |
| 3. | Boseker EH, Bickel WH, Dahlin DC. A clinicopathologic study of simple unicameral bone cysts. Surg Gynecol Obstet 1968;127:550-60. [Google Scholar] |
| 4. | Wilkins RM. Unicameral bone cysts. J Am Acad Orthop Surg 2000;8:217-24. [Google Scholar] |
| 5. | Rougraff BT, Kling TJ. Treatment of active unicameral bone cysts with percutaneous injection of demineralized bone matrix and autogenous bone marrow. J Bone Joint Surg Am 2002;84:921-9. [Google Scholar] |
| 6. | Haidar SG, Culliford DJ, Gent ED, Clarke NM. Distance from the growth plate and its relation to the outcome of unicameral bone cyst treatment. J Child Orthop 2011;5:151-6. [Google Scholar] |
| 7. | Donaldson S, Wright JG. Recent developments in treatment for simple bone cysts. Curr Opin Pediatr 2011;23:73-7. [Google Scholar] |
| 8. | Rizk AS. Transfixing Kirshner wires for fixation of intertrochanteric valgus osteotomies in management of pediatric coxa vara. J Orthop Traumatol 2017;18:365-78. [Google Scholar] |
| 9. | Seller K, Wild A, Westhoff B, Raab P, Krauspe R. Radiological evaluation of unstable (acute) slipped capital femoral epiphysis treated by pinning with Kirschner wires. J Pediatr Orthop B 2006;15:328-34. [Google Scholar] |
| 10. | Sung AD, Anderson ME, Zurakowski D, Hornicek FJ, Gebhardt MC. Unicameral bone cyst: A retrospective study of three surgical treatments. Clin Orthop Relat Res 2008;466:2519-26. [Google Scholar] |
| 11. | Dormans JP, Pill SG. Fractures through bone cysts: Unicameral bone cysts, aneurysmal bone cysts, fibrous cortical defects, and nonossifying fibromas. Instr Course Lect 2002;51:457-67. [Google Scholar] |
| 12. | Wagner H. Femoral osteotomies for congenital hip dislocation. In: Acetabular dysplasia: Skeletal dysplasia in childhood. Germany: Springer-Verlag; 1978. p. 85-105. [Google Scholar] |
| 13. | Widmann RF, Hresko MT, Kasser JR, Millis MB. Wagner multiple K-wire osteosynthesis to correct coxa vara in the young child: Experience with a versatile 'tailor-made' high angle blade plate equivalent. J Pediatr Orthop B 2001;10:43-50. [Google Scholar] |
| 14. | Trenholm A, Landry S, McLaughlin K, Deluzio KJ, Leighton J, Trask K, et al. Comparative fixation of tibial plateau fractures using alpha-BSM, a calcium phosphate cement, versus cancellous bone graft. J Orthop Trauma 2005;19:698-702.t. [Google Scholar] |
| 15. | Zhang T, Price CT, McCarthy JJ, Nguyen J, Noonan KJ. The use of triphasic bone graft for the treatment of pediatric bone cysts: Experience at 2 Institutions. Orthopedics 2018;41:e705-12. [Google Scholar] |
Fulltext Views
4,886
PDF downloads
485





