Translate this page into:
Neglected anterior Monteggia lesion with a displaced intra-articular medial condyle fracture in a child: A rare and challenging association
Corresponding Author:
Tamer A El-Sobky
Department of Orthopaedic Surgery, Division of Pediatric Orthopaedics, Faculty of Medicine, Ain-shams University, Abbasia, Cairo
Egypt
tamersh@hotmail.com
| How to cite this article: El-Sobky TA, Samir S, Aly AS. Neglected anterior Monteggia lesion with a displaced intra-articular medial condyle fracture in a child: A rare and challenging association. J Musculoskelet Surg Res 2017;1:49-52 |
Abstract
Monteggia fracture dislocation refers to a dislocation of the proximal radioulnar joint together with an ulnar fracture. Bado described four types of Monteggia lesions. Type I is the most common, where the radial head is dislocated anteriorly. Misdiagnosis of pediatric Monteggia fracture dislocations is fraught with potentially serious functional complications and treatment challenges. This is especially true in the event of late presentation and association with a simultaneous ipsilateral skeletal comorbidity. We present the case of a child with an extremely rare neglected type I Monteggia fracture dislocation associated with a displaced intra-articular medial humeral condyle fracture. We aim to demonstrate the radioclinical outcome of surgical management of this child and to offer possible mechanisms of injury found upon fracture characteristics and biomechanics. The patient was managed by a characteristic open surgical technique that offered satisfactory functional and radiologic outcomes on the short-term despite late presentation. We established correlations between the proposed injury mechanism, imaging abnormalities, and intraoperative findings that aided in management implementation.
Introduction
The relatively uncommon Monteggia fracture represents a radial head dislocation with a concomitant ulnar fracture.[1] The ulnar fracture is usually radioclinically apparent. The radial head dislocation may be missed if radiographs are inadequate. Appropriately assessing the nature of this injury in a timely fashion is crucial to prevent unrecoverable complications.[1] Pediatric Monteggia fractures are stigmatized by a considerable incidence of misdiagnosis.[1] Although unusual, publications showed pediatric Monteggia fracture dislocations to occur concomitantly with other injuries such as distal humeral fracture,[2],[3],[4],[5],[6],[7] lateral condyle fracture,[8],[9] distal radial fracture,[10],[11],[12] Galeazzi fracture,[13] and olecranon fracture.[14] Only one publication reports the association of pediatric Monteggia fracture dislocation with medial humeral condyle fracture (MHCF).[15] Nevertheless, it reports a fresh fracture dislocation that was managed successfully by closed reduction. We aim to demonstrate the radioclinical outcome of surgical management of a boy with neglected anterior Monteggia fracture dislocation associated with a severely displaced intra-articular MHCF. We intend to offer possible injury mechanisms founded upon fracture characteristics and biomechanics.
Case Report
A 3-year and 8-month-old boy presented to our outpatient clinic 4 weeks after falling on the right upper limb from a donkey back riding. He was initially offered a posterior slab after elbow radiographs at another hospital. The initial radiographs were unavailable at presentation. On examination, the radial head was palpable at the anterolateral elbow. Passive range of elbow flexion ranged from 50° to 80° (arc = 30°). Forearm rotation showed painful passive restriction of supination and full pronation. The neurovascular status was intact. The patient received orthogonal elbow and full forearm radiographs and elbow computerized tomography (CT) scans with three-dimensional reformat. The right forearm radiographs depicted a united greenstick fracture with minimal anterior angulation at the junction of the distal and middle 1/3rd of the ulna, anterior radial head dislocation with inferior, anterior, and lateral displacements of an MHCF [Figure - 1] and [Figure - 2].
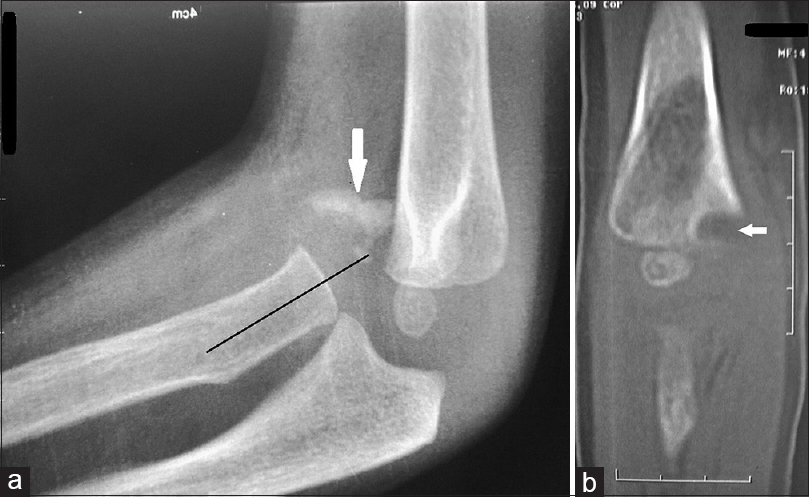 |
| Figure 1: Imaging of the right elbow. (a) Radiographs of the right elbow 5 weeks postinjury. The line drawn marks the malalignment of the radiocapitellar line indicating anterior dislocation of the radial head. Note the anteriorly displaced and rotated medial condyle fracture fragment (arrow). (b) Coronal computed tomography image depicting an anteromedial defect of the metaphyseal/physeal region of the medial condyle. Note that the coronal image represents the anteromedial portion of the distal humerus as the radius (dislocated anteriorly) and capitellar ossification center (anteriorly located) are visualized. The bony defect demonstrated represents part of the coronoid fossa while the traumatic lesion is shown far medially (arrow) |
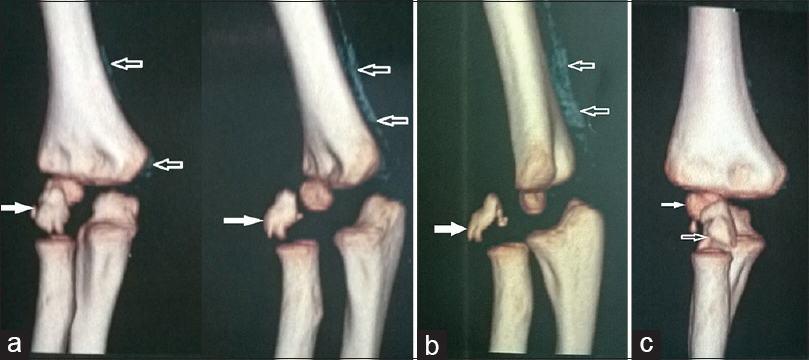 |
| Figure 2: Computed tomography scan of the right elbow with three-dimensional reconstruction. (a and b) Note that the medial condyle metaphyseal fracture fragment is displaced inferiorly, anteriorly, and laterally to its normal position (solid arrows). Fragment rotation is depicted. A periosteal reaction is seen along the medial aspect of the distal humerus (hollow arrows). (c) The displaced medial condylar fragment (hollow arrows) in relation to the capitellum (solid arrow) is depicted |
Surgical technique
We employed an anterolateral approach to the elbow to relocate the radial head. We carried dissection along the medial border of brachioradialis. The radial nerve was identified proximally at the level of the elbow and followed distally until it branched into posterior interosseous nerve at the upper border of the supinator that was reflected subperiosteally from the ulnar border. We dissected fibrous adhesions around the radial head and excised the intra-articular MHCF fragment. Annular ligament (AL) remnants interposed within the radiocapitellar joint and obstructing relocation were debrided. A transverse opening-wedge posterior-apexed proximal ulnar osteotomy was executed, radial head relocated in 90° of elbow flexion and transfixed by two transarticular Kirschner (K)-wires in neutral forearm rotation [Figure - 3]. We did not perform ulnar osteotomy fixation nor AL reconstruction. We applied a posterior slab in 90° flexion for 4 weeks after which gradual assisted active flexion-extension range of motion (ROM) exercises were instituted. At 6 weeks postoperatively, the K-wires were removed and physiotherapy was continued including ROM at the elbow and forearm rotation.
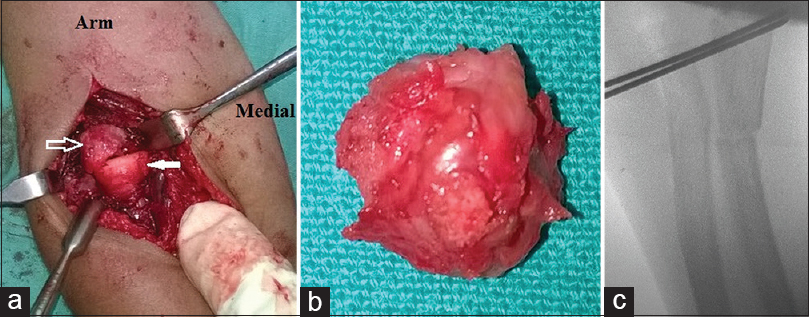 |
| Figure 3: Intraoperative images of the anterolateral approach to right elbow. (a) Note the close proximity of the medial condylar fracture fragment (hollow arrow) and the radial head epiphysis (solid arrow). (b) The medial condylar fracture fragment after excision. (c) Transfixing K-wires across the proximal radioulnar articulation. Note the proximal ulnar osteotomy |
Postoperative assessment
Postoperatively, the patient developed a complete posterior interosseous nerve palsy. The lesser fingers and thumb recovered in 1 month and 5 months, respectively. We used the Mayo Elbow Performance Score to assess elbow function.[16] Our patient exhibited complete pain relief, a flexion arc of 90° (35°‘125°), a stable elbow, and no difficulty in executing daily activities, categorizing his Mayo elbow performance score as excellent. The forearm possessed a 30° arc around neutral rotation. Postoperative CT scans and radiographs depicted normalization of radiocapitellar alignment at 1-year follow-up [Figure - 4].
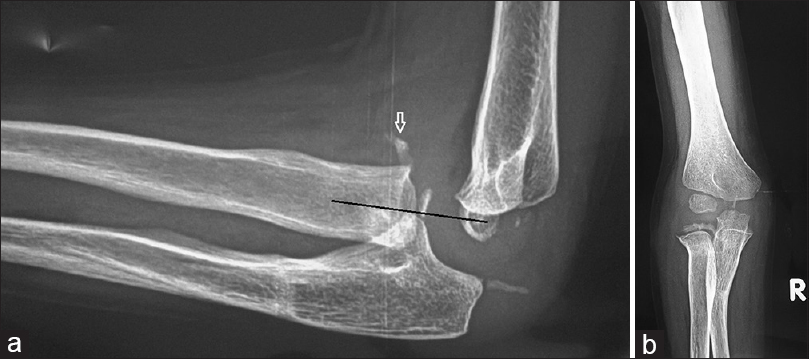 |
| Figure 4: Radiographs at 1-year follow-up. Note the restored radiocapitellar relationship in lateral (a) and anteroposterior (b) planes. Note the remodeling of ulnar osteotomy in the sagittal plane (a) and mild residual angulation in the coronal plane (b). Note the ossification of the proximal radial epiphysis (a and b) that was unapparent at the time of presentation. Note a minor flake of extracapsular ectopic bone formation in the lateral view (arrow) (a). This flake is also appreciated just medial and overlapping with the ossification center of the proximal radius in the anteroposterior view (b) |
Discussion
Kilfoyle classified the rare isolated pediatric MHCFs. Type I is a nondisplaced, nonarticular fracture through the medial condylar metaphysis extending distally to the physis. Type II is a nondisplaced fracture but extends through the articular surface of the medial condylar epiphysis. Type III fracture involves displacement and rotation of the distal condylar fracture fragment.[15],[17] The MHCF pattern of our patient was wholly metaphyseal. Nonetheless, it was displaced and did not involve the entire medial condyle as described in Type I Kilfoyle.[15],[17]
Mechanism of injury
Knowledge of elbow injury mechanisms is crucial to a comprehensive diagnosis and management.[5],[6],[8] We propose that the mechanism of injury in our patient was caused by a fall onto a hyperextended elbow with a pronated forearm that forced the arm into hyperpronation. A hyperextended and assumingly valgus inclination of the elbow created a posterior and laterally directed force that eventually caused the anteromedial portion of the medial condyle to fracture by tensile failure and displace laterally, anteriorly, and inferiorly. We speculate that this relatively small fragment gained intra-articular access through an anterior capsular rent or avulsion. Continuation of the trauma force caused the ulna to fracture and the radial head to dislocate anteriorly from the capitellum in a simultaneous fashion. The valgus force produced at the hyperextended elbow was facilitated by a presumably shoulder abduction at the time of ground impact. The resisted flexion and supination caused by the biceps/brachialis and forearm supinator/extensors, respectively, contributed to the pathomechanics. Additionally, a pronated forearm entails internal rotation of the radius with respect to the ulna and brings the proximal radius close to MHCF. This may explain the close proximity of the MHCF to the anteriorly dislocated radial head demonstrated radiographically and intraoperatively [Video 1]: Mechanism of injury]. The proposed injury mechanism in our patient seems applicable on Monteggia fracture variants Type I [3],[5] and IV,[2],[6] with concomitant supracondylar humeral fractures. A similar mechanism is proposed for Monteggia fractures Type III and concomitant lateral condyle fracture with the exception of a varus elbow inclination.[8],[9] We suggest that a medial epicondyle (ME) avulsion theory is an unlikely scenario in our patient due to; (a) rarity of occurrence in the patient's age group, (b) the intra-articular fragment was devoid of any musculoligamentous attachments, (c) the ME was unossified, (d) ME fractures usually have insignificant metaphyseal components, (e) elbow stability to valgus stress was demonstrated.[18],[19]
Management strategy
We excised the MHCF fragment as relocation and fixation into its anteromedial bed were inaccessible through the implemented anterolateral approach. We believe that the excised metaphyseal fragment would have inconsequential effects on physeal growth and joint stability. Not fixing the ulna reduced operative time and trauma.
In general, there is no consensus on the best treatment protocol for neglected pediatric Monteggia lesions. A recent systematic review demonstrated that the most common treatment modality was the open reduction with ulnar osteotomy and AL reconstruction, followed by open reduction and ulnar osteotomy.[1] Missed pediatric Monteggia injuries have also been treated by acute [20] and gradual [21],[22] angulation and elongation of the ulna to allow for reduction of the radial head. These authors did not undertake open reduction of the radial head, nor AL reconstruction, nor temporary fixation of the radial head with a transarticular wire.[20],[21],[22] They achieved satisfactory radioclinical results. We used open reduction as the radial head was irreducible under anesthesia and chiefly because of the severely displaced intra-articular MHCF fragment. Nonetheless, our technique was in concordance with the previous authors,[20],[21],[22] with regard to not undertaking AL reconstruction.
A systematic review showed that the use of transcapitellar pin stabilization of the reduced radial head is a common practice despite unsettled radioclinical gains.[1] We believe that transcapitellar pin stabilization is fraught with chondrolysis, joint stiffness, and intra-articular wire breakage. We, therefore, used transarticular proximal radioulnar K-wire fixation. That rigid stabilization technique negated the need to reconstruct the AL and the fixation of the ulnar osteotomy. We are unaware of any studies that do not fix the ulnar osteotomy. In our case, sagittal alignment was maintained to complete union. Since the direction of the radial head dislocation was uniplanar and sagittal (anterior), the loss of ulnar reduction in the coronal plane did not impact function nor radiocapitellar alignment. Nevertheless, we do not recommend not fixing the ulnar osteotomy routinely.
A systematic review reported that posterior surgical approaches of Kocher's and Boyd's are most commonly used for the radial head open reduction.[1] In contrast, the anterolateral approach was more suited to our patient because of the anterior direction of the dislocation. Furthermore, the displaced intra-articular MHCF would have been largely inaccessible by the posterior approaches. Shillington et al. reported an MHCF and an ipsilateral anteriorly dislocated radial head without an ulnar fracture.[17] Kim et al. published the only report of a combined Monteggia fracture dislocation and MHCF in a child.[15] Although our study seems similar to that of Kim et al., substantial differences with regard to treatment planning and potential outcomes exist. We were confronted with a late-presenting Monteggia lesion and a concomitant intra-articular MHCF. In contrast to Kim et al.,[15] who used percutaneous fixation of the MHCF and closed reduction of the radial head, our case necessitated an open procedure for all components of the deformity. Kim et al. recorded a full ROM in the elbow and forearm.[15] Our patient suffered a restriction in ROM that had insignificant functional implications. This discrepancy may be attributable to the late presentation, the necessity of open reduction with subsequent scarring, and longer immobilization period encountered in our case. The incomplete forearm rotation in our case may partially be attributed to transarticular radioulnar fixation.
Conclusion
This study reemphasizes the vitality of radiologic evaluation of pediatric Monteggia fractures in acute settings. Our surgical strategy in this clinical setting yielded satisfactory short-term radioclinical outcomes. Reproducing the fracture mechanism augmented our interpretation of imaging and intraoperative abnormalities. In late-presenting pediatric Monteggia, a concomitant MHCF may complicate management difficulties.
Recommendations
Junior emergency department physicians are urged to consult senior orthopedic surgeons and radiologists to avoid misreading of pediatric elbow radiographs in the acute setting.
Acknowledgment
The authors thank Dr. Samer Arafa for providing the graphic animations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors contributions
TAE and SS conceived and designed the study, conducted research, provided research materials, and collected and organized data. TAE, SS and ASA analyzed and interpreted data. TAE wrote initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft, have checked the article for plagiarism, and are responsible for the content and similarity index of the manuscript.
| 1. | Goyal T, Arora SS, Banerjee S, Kandwal P. Neglected Monteggia fracture dislocations in children: A systematic review. J Pediatr Orthop B 2015;24:191-9. [Google Scholar] |
| 2. | Arazi M, Oǧün TC, Kapicioǧlu MI. The Monteggia lesion and ipsilateral supracondylar humerus and distal radius fractures. J Orthop Trauma 1999;13:60-3. [Google Scholar] |
| 3. | Arora S, Sabat D, Verma A, Sural S, Dhal A. An unusual Monteggia equivalent: A case report with literature review. J Hand Microsurg 2011;3:82-5. [Google Scholar] |
| 4. | Cobanoglu M, Şavk ŞO, Cullu E, Duygun F. Ipsilateral supracondylar humerus fracture and Monteggia lesion with a 5-year follow-up: A rare injury in a young girl. BMJ Case Rep 2015;2015. pii: bcr2014206313. [Google Scholar] |
| 5. | Powell RS, Bowe JA. Ipsilateral supracondylar humerus fracture and Monteggia lesion: A case report. J Orthop Trauma 2002;16:737-40. [Google Scholar] |
| 6. | Rouhani AR, Navali AM, Sadegpoor AR, Soleimanpoor J, Ansari M. Monteggia lesion and ipsilateral humeral supracondylar and distal radial fractures in a young girl. Saudi Med J 2007;28:1127-8. [Google Scholar] |
| 7. | Sharma H, Wilson N. T-condylar distal humeral fracture associated with irreducible anterior radial head dislocation in an 11-year-old child: A case report. J Trauma 2007;63:202-4. [Google Scholar] |
| 8. | Dattani R, Patnaik S, Kantak A, Lal M. Distal humerus lateral condyle fracture and Monteggia lesion in a 3-year old child: A case report. Acta Orthop Belg 2008;74:542-5. [Google Scholar] |
| 9. | Güven M, Eren A, Kadioǧlu B, Yavuz U, Kilinçoǧlu V, Ozkan K, et al. The results of treatment in pediatric Monteggia equivalent lesions. Acta Orthop Traumatol Turc 2008;42:90-6. [Google Scholar] |
| 10. | Deshpande S, O'Doherty D. Type I Monteggia fracture dislocation associated with ipsilateral distal radial epiphyseal injury. J Orthop Trauma 2001;15:373-5. [Google Scholar] |
| 11. | Rodgers WB, Smith BG. A type IV Monteggia injury with a distal diaphyseal radius fracture in a child. J Orthop Trauma 1993;7:84-6. [Google Scholar] |
| 12. | Williams HL, Madhusudhan TR, Sinha A. Type III Monteggia injury with ipsilateral type II Salter Harris injury of the distal radius and ulna in a child: A case report. BMC Res Notes 2014;7:156. [Google Scholar] |
| 13. | Maeda H, Yoshida K, Doi R, Omori O. Combined Monteggia and Galeazzi fractures in a child: A case report and review of the literature. J Orthop Trauma 2003;17:128-31. [Google Scholar] |
| 14. | Kamudin N, Firdouse M, Han CS, M Yusof A. Variants of Monteggia type injury: Case reports. Malays Orthop J 2015;9:23-7. [Google Scholar] |
| 15. | Kim YS, Lee HM, Kim JP, Lim CR. Unusual presentation of a type 1 Monteggia equivalent lesion: Simultaneous medial humeral condyle fracture with ipsilateral anterior dislocation of the radial head and acute plastic bowing of the ulna. J Pediatr Orthop B 2014;23:383-8. [Google Scholar] |
| 16. | Cusick MC, Bonnaig NS, Azar FM, Mauck BM, Smith RA, Throckmorton TW, et al. Accuracy and reliability of the mayo elbow performance score. J Hand Surg Am 2014;39:1146-50. [Google Scholar] |
| 17. | Shillington M, Collins B, Walsh HP. Medial humeral condyle fracture with an ipsilateral dislocated radial head. Ann R Coll Surg Engl 2009;91:W12-4. [Google Scholar] |
| 18. | EL-Sobky TA, Haleem JF, Sakr HM, Aly AS. A neglected markedly displaced medial epicondyle fracture with simultaneous ulnar nerve palsy in an adolescent. Clin Orthop Surg 2017;9:542-6. [Google Scholar] |
| 19. | Panthi S, Khatri K, Kharel K, Vaishya R, Agarwal AK, Vijay V, et al. Radiological and functional outcome of medial epicondyle fracture treated surgically in children and adolescents: A Retrospective study. Cureus 2017;9:e953. [Google Scholar] |
| 20. | Lädermann A, Ceroni D, Lefèvre Y, De Rosa V, De Coulon G, Kaelin A, et al. Surgical treatment of missed Monteggia lesions in children. J Child Orthop 2007;1:237-42. [Google Scholar] |
| 21. | Exner GU. Missed chronic anterior Monteggia lesion. Closed reduction by gradual lengthening and angulation of the ulna. J Bone Joint Surg Br 2001;83:547-50. [Google Scholar] |
| 22. | Kawoosa AA, Dhar SA, Butt MF, Wani SA, Mir MR, Dar TA, et al. Stable relocation of the radial head without annular ligament reconstruction using the ilizarov technique to treat neglected Monteggia fracture: Two case reports. J Med Case Rep 2010;4:344. [Google Scholar] |
Fulltext Views
2,309
PDF downloads
785





