Translate this page into:
Does magnetic resonance imaging impact pre-operative plans in adolescent idiopathic scoliosis patients? A retrospective study
-
Received: ,
Accepted: ,
How to cite this article: Al Assiri SS, Al Eissa SI, Konbaz FM, Al Helal FH, Abaalkhail MS, AlSalman MJ, et al. Does magnetic resonance imaging impact pre-operative plan in adolescent idiopathic scoliosis patients? A retrospective study. J Musculoskelet Surg Res 2022;6:167-71.
Abstract
Objectives:
Adolescent idiopathic scoliosis (AIS) has been rigorously discussed in academia for the better part of a century, primarily due to its nuanced and complex management. To date, there are no universal criteria for its management. The use of pre-operative magnetic resonance imaging (MRI) in all patients with AIS is still debatable. We aimed to determine the necessity of using pre-operative routine MRI assessment in all patients treated for AIS.
Methods:
A retrospective and descriptive medical chart review study was done. We examined AIS patients diagnosed between 10 and 18 years of age who underwent surgical treatment between 2016 and 2020. A full medical history and a complete spine clinical examination were performed on all patients.
Results:
Of 267 consecutive patients with verified AIS who underwent surgical correction, 176 were included in the analysis. All patients had normal pre-operative physical and neurological examinations. There were 138 (78%) female and 38 (22%) male patients. MRI findings of neural axis abnormalities were observed in eight of 176 patients (4.54%).
Conclusion:
In our study, the incidence of abnormalities in the neural axis was low and no additional neurosurgical procedures were performed. This could be due to our strict inclusion criteria. However, we cannot establish a recommendation regarding the routine use of pre-operative MRI. A meta-analysis of the currently available data may provide a better assessment in terms of cost-effectiveness and pave the way for the implementation of guidelines for screening protocols.
Keywords
Adolescent
Idiopathic scoliosis
Incidence
Magnetic resonance imaging
Syringomyelia
INTRODUCTION
Adolescent idiopathic scoliosis (AIS) has been rigorously discussed in academia for the better part of a century, primarily due to its nuanced and complex management. To date, there are no universal criteria for its interventions.[1] AIS is defined as rotation with lateral deflection of the vertebral bodies, presenting most commonly in adolescent females.[2] The term “idiopathic” holds tremendous importance here, as we cannot pinpoint a specific cause (e.g., congenital deformities, various genetic syndromes, and neuromuscular conditions). The condition’s idiopathic nature makes the physical examination, clinical history, and — most importantly — the radiological diagnosis modality of choice particularly important.[3] Many ongoing debates are regarding the risk factors and neural axis abnormalities associated with AIS. Neurological abnormalities associated with AIS have been documented since the early 1940s.[4] Intra-spinal diseases such as tethering of the cord (cauda equina fibrous adhesion), Arnold–Chiari malformation, and syringomyelia are among the more frequent neural axis abnormalities.[1,5] Prominent recent papers estimate that anywhere from 2 to 26% of AIS patients have associated neural axis abnormalities.[3,6,7] Neurological abnormalities are asymptomatic for the most part and are subclinical, as pointed out by Dewan et al.[8] Nevertheless, these abnormalities are clinically pertinent to the surgical correction of scoliosis. The use of standard pre-operative magnetic resonance imaging (MRI) to investigate these anomalies in AIS patients is still debatable.[1,5-9] Many authors recommended the routine use of MRI for pre-operative assessment.[5,9] Two papers reported similar prospective surveillance methods and a similar prevalence range (3.8% and 9.9%, respectively).[5,9] Therefore, the authors hypothesized that the use of pre-operative MRI to diagnose neural axis anomalies in AIS patients could be critical. Conversely, other authors, like Dewan et al.,[8] found no significant rates of complications and thus do not recommend MRI preoperatively.
Furthermore, risk factors have also seen their fair share of debate. At present, abnormal neurological examination prompts the use of MRI. However, other risk factors have been historically debated with regard to whether they warrant MRI. For example, age, gender, curve type, and direction are still intensely discussed. In their massive prospective cohort study of 2206 individuals, Diab et al.[1] concluded that juvenile-onset and hyperkyphosis were significantly associated with neural axis abnormalities. However, many other studies could not confirm the same results and often found other factors, such as male gender and curve direction, to be of importance.[1,5,9] For example, Nakahara et al.[5] estimated that (13.3%) males had neural axis abnormalities; in contrast, (2.8%) female patients had abnormalities detected by MRI. One of the few studies that revealed no strong links between neural axis anomalies and AIS was published by Dewan et al.[8] While most existing studies have estimated a range of incidence for AIS and neural axis abnormalities, none have explicitly confirmed the incidence of neural axial anomalies in our region. The goal of our study was to determine the incidence of neural axis anomalies in MRI in AIS patients receiving deformity correction surgery at our institution, as well as to describe the risk variables that necessitate MRI screening.
MATERIALS AND METHODS
A retrospective and descriptive medical chart review were performed with 257 consecutive AIS patients between 10 and 18 years of age who underwent surgical treatment between 2016 and 2020. Patients diagnosed with muscular dystrophy or connective tissue disorders, congenital scoliosis, syndromic scoliosis, and atypical curves (such as left thoracic curves or kyphoscoliosis) were excluded in addition to patients who did not do MRI or surgery. In total, 176 patients were included in the study. All patients underwent a comprehensive medical history and back examination, which included a forward bend test and upper and lower motor neuron testing, as well as deep tendon and abdominal reflex evaluation.
Clinical and demographic data were retrieved from medical files, including age at diagnosis, age at surgery, gender, body mass index (BMI), and type of complication before and after 30 days of surgery. Furthermore, any data regarding neurosurgery intervention were done before scoliosis correction was retrieved. Plain radiographs of the spine were performed, including standing posterior-anterior and lateral images. Images in Digital Imaging and Communications in Medicine format were retrieved from the Picture Archiving and Communications System and uploaded to the online imaging software KeOps (SMAIO, Lyon, France). The Cobb method was used to determine the magnitudes of the curves.[10] Measurement involved curve type according to the Lenke classification system.[11] Cobb’s angle of ≤45° was considered as mild scoliosis, between 46° and 80° denoted more moderate scoliosis and more than 81° indicated severe scoliosis. Using a 1.5 Tesla MR Scanner (Sonata; Siemens, Erlangen, Germany), all patients had a whole-spine MRI with T1- and T2-weighted sagittal and axial scans. The cord appearance, the position of the conus medullaris, and the presence or absence of syringomyelia, cord tethering, and diastematomyelia were all reported. A single musculoskeletal radiologist analyzed MRI scans and Cobb angles to minimize intra-observer variation.
Statistical measures
Means and standard deviations, as well as frequencies and percentages, are used to present data. When comparing categorical variables, the Chi-square test was employed, whereas when comparing continuous variables, the t-test was utilized. Statistical significance was defined as P < 0.05. To determine the degree and direction of the association between variables, the Pearson correlation coefficient test was utilized. The data were analyzed using R software (Vienna, Austria), which can be found at https://www.R-project.org/ .
RESULTS
The study looked at a total of 176 AIS patients who had surgery to correct their scoliosis. Physical and neurological examinations were normal in all patients before surgery. There were 138 (78%) female and 38 (22%) male patients. The mean age at diagnosis was 14.35 years and the overall mean age of surgery was 16.91 years. The average BMI was 20.9 kg/m2. The average Cobb angle was 62.61°, indicating that most of the patients had moderate spine curvature. According to Lenke classification,[11] 31 patients were Lenke Type 1, 19 were Type 2, 44 were Type 3, 23 were Type 4, 51 were Type 5, and eight were Type 6. MRI findings of neural axis abnormalities were observed in eight of 176 patients (4.54%). Four patients had syringomyelia and one patient had diastematomyelia.
One patient had lumbar spine stenosis and posterolateral disc L4-L5 and L5-S1. Two patients had tethered cords. All patients consulted with the neurosurgical department, and they required regular outpatient follow-up, without any additional surgical management.
Furthermore, all patients underwent intra-operative neuromonitoring that included both motor and somatosensory evoked potentials (MEP/SSEP), with no abnormalities in MEP/SSEP. None of our patients had immediate intra- or postoperative neurological complications. During the follow-up period, no changes were detected in the numbers or dimensions of syrinxes in postoperative MRI. No additional anomalies of the medulla spinalis or a change in spur were noticed in the patient with diastematomyelia. No systemic complications or late neurological deficits developed during follow-up.
A Chi-square test of independence was performed to examine the relationship between curve magnitude (mild, moderate, and severe) and patients with normal MRI findings; no statistically significant difference was found (P = 0.934) with 95% confidence that the mean lies between (1.8564 and 2.0414) [Figure 1]. Furthermore, there was no statistically significant difference between patient gender and MRI findings (P = 0.522). The degree and direction of the link between BMI (ratio variable) and MRI (nominal variable) data were assessed using the Pearson correlation coefficient test. The value of R2, the coefficient of determination, was 0.0011, indicating that BMI did not have a strong correlation with MRI findings [Figure 2].
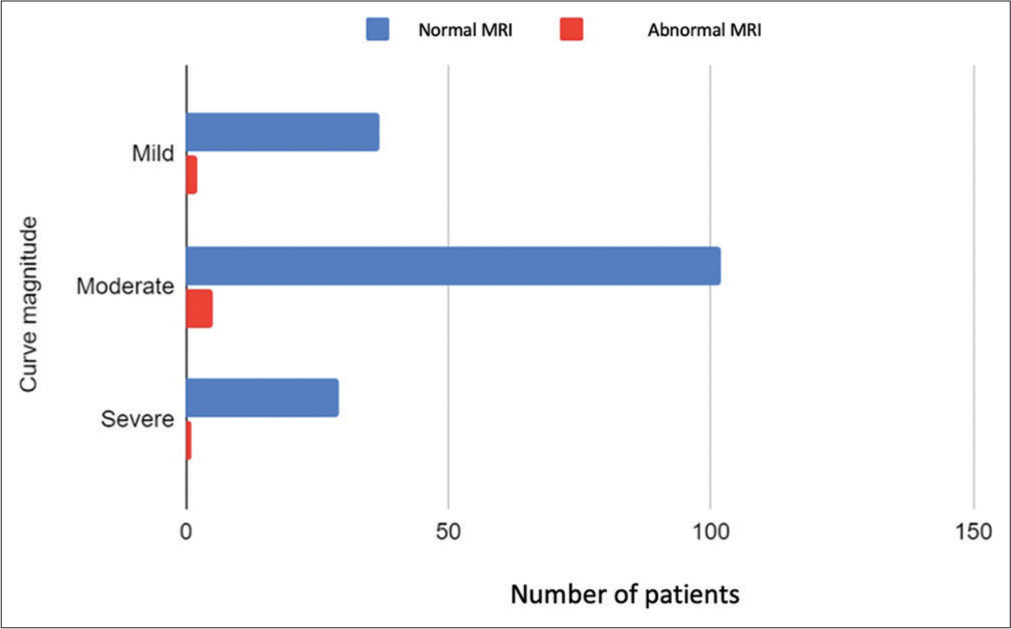
- The relationship between curve magnitude and magnetic resonance imaging.
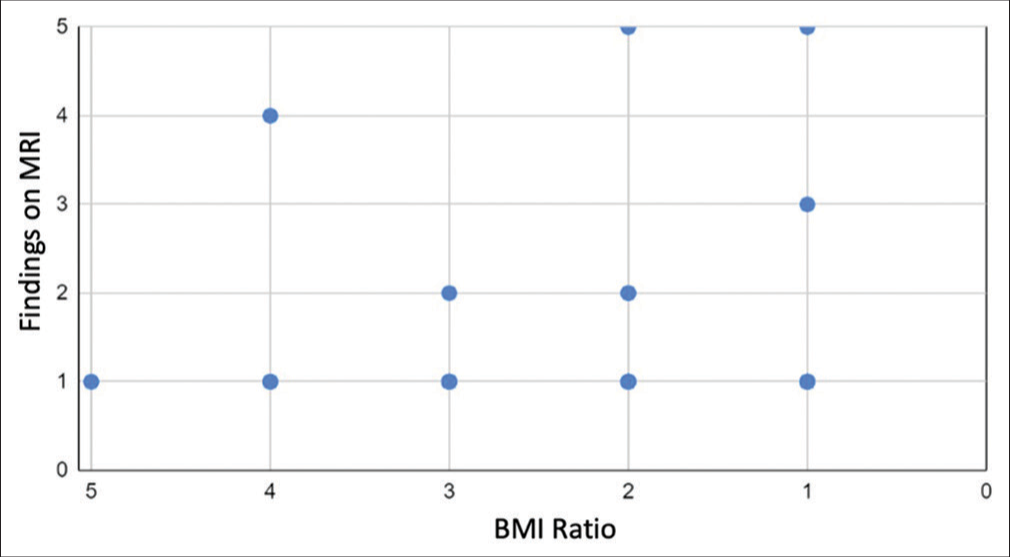
- The relationship between patient body mass index and magnetic resonance imaging findings.
DISCUSSION
With the increased use of MRI, the prevalence of neural axis disorders has increased. Patients with AIS have been documented to have neuraxial anomalies such as Chiari malformation and syringomyelia. Correction of scoliosis in people with neural axis anomalies may cause neurological complications.[1,8,12]
According to the different studies, the incidence of neural axis anomalies in AIS patients ranges from 2 to 26%.[3,6,7] According to Dewan et al.,[8] 114 (14%) of 811 scoliosis patients showed aberrant neural axis, with no significant link with a left-sided thoracic curve, double thoracic curve, male gender, or scoliosis diagnosis before the age of 10. Ameri et al.[9] reported that 9.9% of 271 patients had neural axis abnormalities and that they were directly related to the male gender and early-onset idiopathic scoliosis disease. Nakahara et al.[5] found that 3.8% of 472 patients had neural axis abnormalities and that these correlated with several factors, such as early-onset scoliosis (<11 years of age), male gender, abnormal neurological findings, and size of the curve. Furthermore, Rajasekaran et al.[13] observed that neural axis anomalies were highly related to a double curve, clinical neurological abnormalities, and scoliosis occurrence at an early age in 16% of 94 patients. They found no correlation between curve size or atypical curves and neural axial abnormalities. However, the previous studies have indicated different risk factors for neural axis abnormalities in patients with AIS. This disparity could be related to differences in study design and patient demographics, as well as a lack of consistent language usage. For example, the terms “syringomyelia,” “hydromyelia,” “dilated central canal,” and the hybrid term “syringohydromyelia” are all used interchangeably to describe fluid-filled cavities in the spinal cord.[14] More and more intraspinal changes are being diagnosed as the MRI use has been increasing over the past decade, but they are considered a normal spinal variation. For example, an idiopathic syrinx is usually asymptomatic and stable in size and some would consider it a normal variation with the absence of underlying pathology.[12] Moreover, finding a central canal with a 1–3 mm diameter should not be considered pathologic in patients with no underlying pathology.[15] Fruergaard et al. presented a large cohort study of patients with AIS who had MRI examinations to overcome this overestimation of the incidence of neural axis abnormalities.[12] They found neural axis abnormalities in 8.9% of patients, but after applying more conservative definitions of neural axis abnormality, they found a prevalence of only 2.9%.
The need for routine pre-operative MRI of the spine to evaluate AIS patients is still being debated. Despite this, there are no established screening guidelines. Many institutions rely on specific findings from the history, physical examination, or plain radiograph to determine whether additional imaging is required. In some hospitals, all patients undergoing surgery have a routine pre-operative MRI of the entire spine. Neural axis abnormalities could be identified in neurologically asymptomatic patients and they are clinically pertinent to the surgical management of scoliosis.[12] The frequency of syringomyelia or Chiari malformations in MRI with a normal neurological examination is not completely understood. In individuals with syringomyelia; however, neurological problems have been reported after surgical scoliosis correction without decompression.[3] Therefore, some authors hypothesize that the routine use of pre-operative whole-spine MRI to determine neural axis abnormalities in patients with AIS can be critical.[5,9] However, some surgeons suggest that pre-operative whole-spine MRI and decompression are not indicated in the absence of neurological abnormalities.[16,17] Notably, no post-operative neurological deficits were seen in the present study, and no neurosurgical interventions were needed. There were no pre-operative MRI findings that mandated changing the surgical plan. Therefore, the question at hand is whether a routine pre-operative MRI is necessary. Some authors[12,16] have questioned the value of routine MRI for patients with apparent AIS, claiming that the incidence of neural axis abnormalities is low and that surgically correcting scoliosis without addressing the neural axial abnormality has no significant increase in surgical complication rate when individuals appear without neurologic symptoms. Wang et al.[16] observed that it was safe to leave some neural axis disorders, such as syringomyelia, untreated while addressing the scoliosis deformity. Moreover, the largest report in the literature – the study by Diab et al.[1] highly against a routine pre-operative MRI; the researchers found no significant differences in outcome when comparing patients with normal versus abnormal MRI findings. Fruergaard et al.[12] discovered no increased neurologic sequelae in AIS patients receiving surgical correction, implying that MRI is not required frequently. According to the different studies, patients with unusual symptoms or neurological impairments should have an MRI.[5,7,9] Conversely, other authors suggested routine pre-operative MRI concerning neural axis abnormalities to prevent neurological complications following correction surgery.[18] Lee et al.[7] recommended routine MRI for all patients having surgical correction for AIS, claiming that early diagnosis of these abnormalities would minimize neurological sequelae with appropriate neurosurgical interventions before final surgical management.
Because of its retrospective nature and limited sample size, the present study has several limitations. In addition, because the study was conducted retrospectively, the precision of some clinical data may be limited. However, despite these limitations, due to our precise inclusion criteria, we were able to get a realistic incidence of neural axis anomalies in individuals with AIS in the Saudi community. Finally, because it encompassed consecutive AIS patients having whole-spine pre-operative MRI at a single institute, our study offers a better level of patient population homogeneity than earlier investigations.
CONCLUSION
We cannot make a recommendation for standard pre-operative whole-spine MRI because the incidence of neural axis anomalies was modest in our study and no further neurosurgery procedures were undertaken. However, advance recognition of such problems in asymptomatic individuals can enable surgeons to use more thorough surgical correction techniques to avoid any neurological consequences by allowing for proper neurosurgical interventions before corrective surgery. To provide solid recommendations, extensive multi-center studies are required, as well as meta-analyses of the present data.
ACKNOWLEDGMENT
The author and coauthors would like to thank Dr. Sahar Aldekhyel and Dr. Tareq Alotaibi for their kind assistance in formatting and organizing the data.
AUTHORS’ CONTRIBUTIONS
SA, SA, and RJ conceived the presented idea. FK and RJ developed the theory and performed the computations. SA and FH verified the analytical methods. FH, MA, and AM collected the data and supervised the findings of this work. MS reviewed all the musculoskeletal images. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
This study was reviewed and approved in September 2017 by the Institutional Review Board (IRB) registration number: (RC17/205/R) at King Abdullah International Medical Research Centre, Riyadh, Saudi Arabia.
DECLARATION OF PATIENT CONSENT
Patients consent not required as there are no patients in this study.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICTS OF INTEREST
There are no conflicts of interest.
References
- Use and outcome of MRI in the surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2011;36:667-71.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of adolescent idiopathic scoliosis. J Child Orthop. 2013;7:3-9.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging effectiveness in adolescent idiopathic scoliosis. Spine Deform. 2021;9:67-73.
- [CrossRef] [PubMed] [Google Scholar]
- Intramedullary lesions of the spinal cord: Study of sixty-eight consecutive cases. Arch Neurpsych. 1944;52:383-99.
- [CrossRef] [Google Scholar]
- Magnetic resonance imaging evaluation of patients with idiopathic scoliosis: A prospective study of four hundred seventy-two outpatients. Spine (Phila Pa 1976). 2011;36:E482-5.
- [CrossRef] [PubMed] [Google Scholar]
- Indications for magnetic resonance imaging in presumed adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2004;86:2187-95.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative magnetic resonance imaging evaluation in patients with adolescent idiopathic scoliosis. Asian Spine J. 2017;11:37-43.
- [CrossRef] [PubMed] [Google Scholar]
- Is the routine use of magnetic resonance imaging indicated in patients with scoliosis? J Spine Surg. 2018;4:575-82.
- [CrossRef] [PubMed] [Google Scholar]
- The role of routine preoperative magnetic resonance imaging in idiopathic scoliosis: A ten years review. Asian Spine J. 2015;9:511-6.
- [CrossRef] [PubMed] [Google Scholar]
- Outline for the study of scoliosis. Am Acad Orthop Surg Instr Course Lect. 1948;5:261-75.
- [Google Scholar]
- Classifications in brief: The lenke classification for adolescent idiopathic scoliosis. Clin Orthop Relat Res. 2018;476:2271-6.
- [CrossRef] [PubMed] [Google Scholar]
- Neural axis abnormalities in patients with adolescent idiopathic scoliosis: Is routine magnetic resonance imaging indicated irrespective of curve severity? Neurospine. 2019;16:339-46.
- [CrossRef] [PubMed] [Google Scholar]
- Intraspinal anomalies in scoliosis: An MRI analysis of 177 consecutive scoliosis patients. Indian J Orthop. 2010;44:57-63.
- [CrossRef] [PubMed] [Google Scholar]
- Syringomyelia: A practical, clinical concept for classification. Acta Neurochir (Wien). 2014;156:2127-38.
- [CrossRef] [PubMed] [Google Scholar]
- Cord cystic cavities: Syringomyelia and prominent central canal. Semin Ultrasound CT MR. 2017;38:98-104.
- [CrossRef] [PubMed] [Google Scholar]
- One-stage correction surgery of scoliosis associated with syringomyelia: Is it safe to leave untreated syrinx without neurological symptom? J Spinal Disord Tech. 2015;28:E260-4.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatment of scoliosis associated with syringomyelia with no or minor neurologic symptom. Eur Spine J. 2015;24:1555-9.
- [CrossRef] [PubMed] [Google Scholar]
- MRI utilization and rates of abnormal pretreatment MRI findings in early-onset scoliosis: Review of a global cohort. Spine Deform. 2020;8:1099-107.
- [CrossRef] [PubMed] [Google Scholar]






