Translate this page into:
Magnetically controlled growing rods' use for early-onset scoliosis management: A single-center experience
2 Department of Surgery, Division of Orthopedic Surgery, King Abdulaziz Medical City-Riyadh, Ministry of National Guard - Health Affairs; King Abdullah International Medical Research Center; Department of Orthopedic, King Abdullah Specialist Children Hospital, Ministry of National Guard - Health Affairs, Riyadh, Saudi Arabia
Corresponding Author:
Samir Alsayegh
King Abdullah Specialist Children Hospital, Ministry of National Guard - Health Affairs, Alrimayah, Riyadh 14611
Saudi Arabia
drsamiralsayegh@gmail.com
| How to cite this article: Annaim MM, Alhandi AA, Alsheddi AA, Alsayegh S, Aleissa SI. Magnetically controlled growing rods' use for early-onset scoliosis management: A single-center experience. J Musculoskelet Surg Res 2020;4:199-204 |
Abstract
Objectives: The challenge in treating early-onset scoliosis (EOS) lies behind the nature of the disease and the technical difficulties. Magnetically controlled growing rods (MCGR) provide a noninvasive option of distraction in EOS. This study reports a single-center experience with the system, assessing hardware-related complications, radiological improvement of curves, and need for revision surgeries. Methods: This was a retrospective study of patients who underwent MCGR placement in a single center with a minimum of 2-year follow-up. Patient demographic data, etiology, and pre/postoperative sagittal and coronal plane images were reviewed. Results: Ten patients were analyzed. The mean age at surgery was 5.1 years. The average preoperative coronal curves were 22.9° in upper thoracic, 71.9° in thoracic, and 47.9° in lumbar, and the mean sagittal curves were 20.9 ± 26.6 in thoracic and 41.3 ± 28.1 in lumbar. The mean follow-up was 3.8 years. The average of progression in all planes was monitored in follow-ups, 15.1° (upper thoracic coronal), 41.0° (thoracic coronal), 24.7° (lumbar coronal), 30.8° (thoracic sagittal), and 18° (lumbar sagittal). The mean percentage of improvement was 47% in the main curve. Seven patients had complications, including, three rod malfunction, four screw pullout that was prominent in two patients. Three patients had revisions due to suspected infection and failure of expansion. Conclusions: In this study, MCGR showed promising results where it enabled growth and showed acceptable improvement in the coronal plane with considerably fewer operations and complications. However, all patients had an alteration in the sagittal plane.
Introduction
Scoliosis is a three-dimensional deformity that has anatomical lateral, anteroposterior, and rotational components. Early-onset scoliosis (EOS) accounts for 80% of all cases; males and females are equally affected with a female predominance in sever-to-moderate curves.[1] EOS is a description of curves that are more than 10° in pediatric patients younger than 10 years of age.[2],[3],[4],[5] The aim of treatment in EOS is to prevent the progression, allow growth, and achieve stability. Therefore, the treatment depends on the type, age, degree of curvature, and the presence of Risser sign.[6],[7] Spinal implants were used in the last decade and became the preferred treatment method. Growth friendly spinal implants have been the gold standard surgical treatment in EOS as they provided internal bracing, delayed spinal fusion, and allowed growth.[6],[8] It was purposely developed to overcome the limitations of EOS's traditional management modalities.[8] Traditional growing rods (TGR), vertical expandable prosthetic titanium ribs, and magnetically controlled growing rods (MCGR) are all currently used as distraction-based implants.[2] The TGR procedure will require patients to undergo distraction surgeries every 6 months under general anesthesia to lengthen the rods, sometimes reaching 15–18 operations until the final fusion at puberty.[6],[8] This objectively high number of surgical interventions carries a surgical and anesthetic risk, and not to mention possible wound complications. General anesthesia risk on developing brains has been addressed in the literature, and warnings have been raised by the Food and Drug Administration; For children <4 years of age, recommendation against receiving general anesthesia or for children to have repeated procedures and those that would last for >3 h.[9],[10] Furthermore, socioeconomic and psychological burdens on both the affected children and their parents cannot be understated.[8] MCGR are, as the name indicates, controlled magnetically with an external device; they are placed initially in the same method as the traditional growing system. However, they provide a noninvasive option of distraction that can be done in an outpatient setting.[6],[8] Distraction can be done in fewer intervals and with conscious neurological monitoring during lengthening.[8] This new system was able to correct the deformities and enable the growth of children with fewer complications, pain, cost, and time compared to the traditional system.[6],[7],[8] The magnetic system is currently recommended by the National Institute for Health and Care Excellence guidelines due to its effectiveness and benefit to childhood scoliosis treatment when compared to the traditional rod systems, although the system is not free from drawbacks, as increased radiation exposure during distraction is cited in the literature.[7] This study reports a single-center experience with the MCGR system, including assessing hardware-related complications, radiological improvement of curves, and need for revision surgeries.
Materials and Methods
A retrospective cohort of ten pediatric patients who underwent MCGR placement as a treatment of EOS was included in the study. All included patients were skeletally immature with flexible curves and required no additional magnetic resonance imaging. The surgeries were done by two board-certified orthopedic spine surgeons in a single tertiary center. All patients followed the same protocol of clinic rod distraction, which was at 3-month intervals. Each visit, the rods were distracted by 2–3 mm depending on the targeted growth and patients' radiographic status. Patients who had <2 years of follow-up were excluded from the study.
Data from 2011 to 2018 were reviewed, and a total of ten patients who underwent MCGR placement surgery met the inclusion criteria. Patient demographics, etiology, and preoperative, postoperative, and last clinic visit of sagittal and coronal plane radiographs and spinal growth measurements were collected. Patients' follow-up data such as the number of distractions, hardware length reached, postoperative complications, and the need for revision surgeries were all collected and reported. All images used for measurements were standing radiographs and were reviewed by a senior author (SS).
After acquiring the proper institutional review board approval, patients' data were collected from the hospital's database. Quantitative variables from patients' data were described using mean, standard deviation, and frequency. The analysis was done using Microsoft Excel (Microsoft corporation, Redmond, WA, USA) and the Statistical Package for the Social Sciences (SPSS) version 23 (SPSS Inc., Chicago, IL, USA). Student's t-test was used to compare pre- and postoperative Cobb angle improvement with a confidence interval of 95%, and P ≤ 0.05 was considered statistically significant.
Results
The ten patients included in the study were seven females and three males. The mean age at diagnosis was 50 ± 25.9 months. Two patients had idiopathic scoliosis, three had syndromic, four had neuromuscular, and one had congenital scoliosis. All patients were treated primarily with MCGR except one who had a conversion from TGR. All patients had dual growing rods; the instrumentation was done using proximal and distal screws except for two patients, in which proximal hooks were used. One patient had one rod removed after 2 years due to suspected infection. Two patients have completed the treatment course of MCGR placement, and the final fusion surgery was performed. The mean age at the initial surgery was 5.1 ± 2.1 years, the mean height preoperatively was 99.4 ± 17.4 cm, and the mean weight was 81.3 ± 14.7 kg.
Pre- and postoperative angle results in the coronal and sagittal planes are detailed in [Table - 1], [Table - 2], [Table - 3]. On the coronal plane, the mean percentage of improvement was 47% in the main curve at the last visit [Table - 1]. Immediate postoperative angles were significantly improved for the upper thoracic and lumbar sections of the curve P ≤ 0.01, whereas for the last follow-up, curve improvement was only statistically significant for the thoracic and lumbar sections of the curve P < 0.01 [Table - 2]. The sagittal plane results showed a statistically significant improvement only in the thoracic spine on the last follow-up P = 0.01 [Table - 2].



The mean follow-up was 15.3 ± 5.4 visits over 3.8 ± 1.8 years; the mean lengthening per visit was 2.4 ± 1.0 mm in the right (RT) rod and 2.4 ± 0.8 mm lengthening in the left (LT) rod [Table - 3].
Patient number 1 had poor follow-up where her first clinic visit was 1 year after MCGR placement. At the time, her thoracic kyphosis worsened to 66° (from 47° preoperatively). She eventually reached 22° in the last follow-up visit, which is in the acceptable range for kyphosis. Patient number 2 [Figure - 1] had her growth spurt in the period of the final fusion surgery arrangement, which led to marginal improvement in her kyphosis from −11° to −3° and further straightening of her lumbar spine from −1° to −6°. Patient number 3 [Figure - 2] also showed straightening of her spine with lumbar lordosis measured at 71° preoperatively to 3° at her last visit. A similar trend was seen with patient number 9 [Figure - 3] with thoracic kyphosis straightening from 20° to 1° only at the final visit [Table - 4].
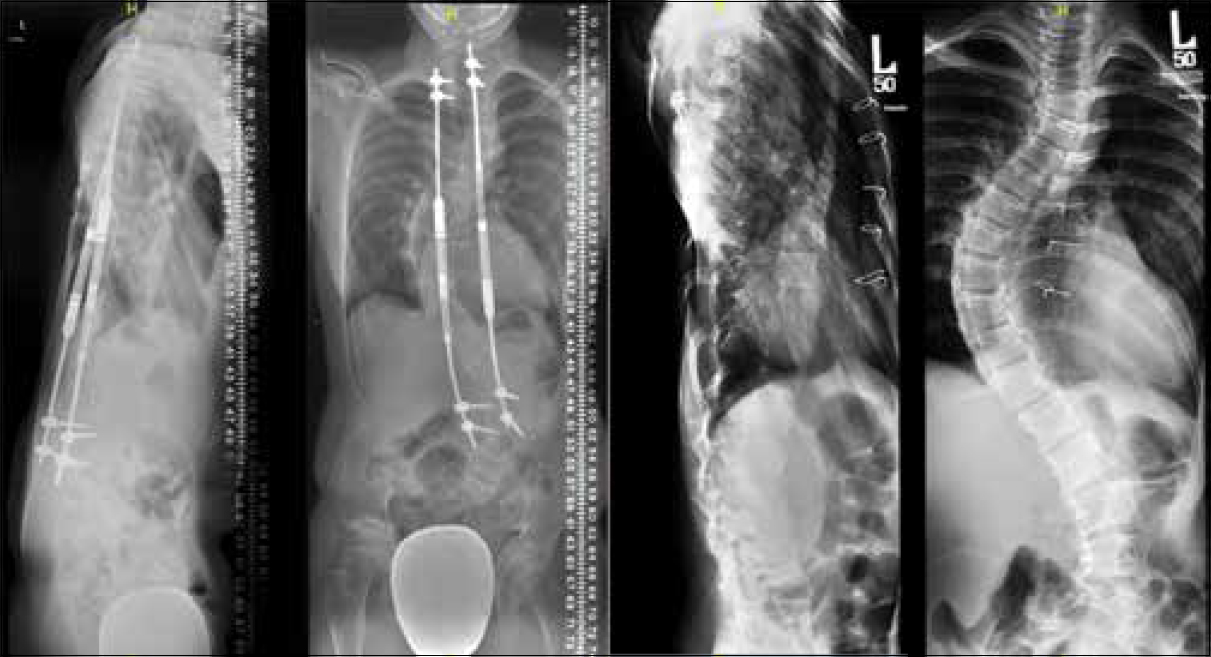 |
| Figure 1: Patient No. 2 had her growth spurt in the period of the final fusion surgery arrangement, which lead to marginal improvement in her kyphosis from -11° to 3° and further straightening of her lumbar spine from -1° to -6° |
 |
| Figure 2: Patient No.3 also showed straightening of her spine with lumbar lordosis measured at 71 preoperatively to 3° at her last visit |
 |
| Figure 3: A similar trend seen with patient No.9 with thoracic kyphosis straightening from 20° to 1° only at the final visit |

Seven patients had complications, including, three rod malfunction, four screw pullout that was prominent in two patients. Three patients had revisions due to suspected infection and failure of expansion. Four patients had screw pullout, two patients complained of hardware prominence, and three patients had revision surgeries due to suspected infection and failure of expansion.
The mean height in the last follow-up was 121.4 ± 18.2 cm. The spinal growth over the years of treatment is demonstrated in [Table - 5]. The first patient had a growth spurt with poor follow-up, and her curve worsened after the 1st year postoperatively. Three patients reached maturity during follow-up, and two had their final fusion surgery. Changes in the sagittal plane for the two patients that underwent their fusion surgery are shown in [Table - 6] (kyphosis and lordosis).


Discussion
The challenge in the treatment of EOS mainly lies behind the nature of the disease and the technical difficulties. The treatment must target the deformity itself, maintain a balanced spine, and allow growth at the same time. Not to forget that the deformity is tridimensional, and the currently available treatment methods only target one or two dimensions at most. In this study, patients showed good improvement in their coronal plane of the major curve, with a mean of 47.4% improvement. Akbarnia et al. found in a comparative study between MCGR and TGR use that the coronal improvement in the last follow-up was 32% with MCGR and 31% in TGR.[11] Similarly, Thompson et al. reviewed 19 patients over a mean of 22-month period, and the coronal improvement was 29.6% at the final follow-up.[12] The primary placement of MCGR and secondary placement results of clinical improvement have been studied by Wimmer et al., and they found that the coronal improvement was 51.3% and 16%, respectively.[13] Furthermore, Keskinen et al. studied the difference between primary and conversion procedures; they found that the patients who had MCGR as their primary treatment have shown improvement by 38%, whereas the conversion group showed only 14.8% at 1-year follow-up.[14] MCGR instrumentation showed its effectiveness in the coronal deformity correction. However, in the sagittal plane, the patients tend to shift into a more straightened spine. This observation was seen in this study's population, as well. The problem has been described by Cheung et al., where the usage of MCGR tends to straighten the spine, and the benefit of contouring can be relatively useful to a certain degree.[15] Patients in the current study showed some improvement in the thoracic and lumbar sagittal curves. However, this improvement has shifted to a straight curve in some of the patients. Knowing that normal thoracic kyphosis ranges from 20° to 50° and the lumbar lordosis ranges from 31° to 79°,[16] the sample showed mixed results in the sagittal plane [Table - 4] and [Table - 6]. As seen in our population, patient numbers 2, 3, and 9 showed good coronal curve improvements unlike in the sagittal plane. Such observation shows that patients do improve very well in the coronal plane while lagging behind in the sagittal plane. This phenomenon can be explained since the expansion occurs at the posterior column mainly, leading to the unintended straightening of the curve sagittally. Lebon et al. reported steady improvement in both the coronal and sagittal planes, and the final follow-up curves were 48° in both thoracic kyphosis and lumbar lordosis.[17] Skov et al. have also reported similar good improvement in the mean sagittal plane; however, they had some outliers, with a range of 6°–65° in thoracic kyphosis and 19°–59° in lumbar lordosis at last follow-up.[18] Keskinen et al. compared the sagittal balance in patients with conversion surgery to primary MCGR placement in EOS. They found that patients who had conversion surgery had significantly worse results than those who underwent a primary MCGR procedure.[14]
In this study, 70% of the patients had complications and 30% had revision surgeries. Moreover, 50% of the complications were due to hardware malfunction and screw pullout. These complications had been described in many case series; Figueiredo et al. found in a systematic review that the total complication rate in dual rod procedure is 30.9%. Nevertheless, the complications do not hold much of the burden when compared to TGR, since patients will need additional surgery down from multiple ones that have been avoided.[19] Proximal junctional kyphosis (PJK) has been observed by some authors such as Hickey et al., who reported it at 50% of their population.[6] Lebon et al. had it only in one out of thirty patients.[17] In our article, the analysis of PJK was not performed.
Patient compliance was a major issue in this population and was reflected in the results. However, the current study remains the first study recording the experience in using MCGR in the Middle East. Further research efforts should address population education and include more strict selection criteria. In addition, the small sample size, heterogeneity in the etiologies, and poor patients' compliance, as well as the functional outcome scores with the psychological outcomes, were not reported in the current study and are acknowledged by the authors as limitations.
Conclusions
MCGR showed promising results where it enabled growth and showed acceptable improvement in the coronal plane with considerably fewer operations. The study reported the possible complications that come with MCGR. However, most patients had an alteration in the sagittal plane, where it shifted into a more straightened spine. Moreover, patient compliance proved to be monumental for success.
Recommendation
A multicenter study with a larger sample size and proper parent education with more strict selection criteria, addressing rod malfunction, sagittal balance, and spinal growth is needed to better assess MCGR as the gold standard treatment in EOS.
Ethical approval
The ethical approval was obtained from the Institutional Review Board of King Abdullah International Medical Research Center, KAIMRC, Riyadh on 30th October 2017, with reference number IRBC-1475/17.
Acknowledgment
We would like to thank Walaa Abdullah Barnawi for her contributions to data collection.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contribution
MMA designed and conducted the study, while AAH with MMA wrote the draft, and SIA with SA critically revised and approved the content. AAS collected, interpreted, and analyzed the data. All authors have critically reviewed and approved the final draft and are responsible for the manuscript's content and similarity index.
| 1. | Solomon L, Warwick D, Nayagam S, editors. Apley's system of orthopaedics and fractures. CRC press Taylor & Francis 338 Euston Road, London NW1 3BH; 2010. [Google Scholar] |
| 2. | Yang S, Andras LM, Redding GJ, Skaggs DL. Early-onset scoliosis: A review of history, current treatment, and future directions. Pediatrics. 2016;137:e20150709. Doi: 10.1542/peds.2015-0709. [Google Scholar] |
| 3. | Menger RP, Kalakoti P, Pugely AJ, Nanda A, Sin A. Adolescent idiopathic scoliosis: Risk factors for complications and the effect of hospital volume on outcomes. Neurosurg Focus 2017;43:E3. [Google Scholar] |
| 4. | Beauchamp EC, Anderson RCE, Vitale MG. Modern surgical management of early onset and adolescent idiopathic scoliosis. Neurosurgery 2019;84:291-304. [Google Scholar] |
| 5. | Cunin V. Early-onset scoliosis: Current treatment. Orthop Traumatol Surg Res 2015;101:S109-18. [Google Scholar] |
| 6. | Hickey BA, Towriss C, Baxter G, Yasso S, James S, Jones A, et al. Early experience of MAGEC magnetic growing rods in the treatment of early onset scoliosis. Eur Spine J 2014;23 Suppl 1:S61-5. [Google Scholar] |
| 7. | Jenks M, Craig J, Higgins J, Willits I, Barata T, Wood H, et al. The MAGEC system for spinal lengthening in children with scoliosis: A NICE Medical Technology Guidance. Appl Health Econ Health Policy 2014;12:587-99. [Google Scholar] |
| 8. | Cheung KM, Cheung JP, Samartzis D, Mak KC, Wong YW, Cheung WY, et al. Magnetically controlled growing rods for severe spinal curvature in young children: A prospective case series. Lancet 2012;379:1967-74. [Google Scholar] |
| 9. | Wilder RT, Flick RP, Sprung J, Katusic SK, Barbaresi WJ, Mickelson C, et al. Early exposure to anesthesia and learning disabilities in a population-based birth cohort. Anesthesiology 2009;110:796-804. [Google Scholar] |
| 10. | Andropoulos DB, Greene MF. Anesthesia and developing brains-implications of the FDA Warning. N Engl J Med 2017;376:905-7. [Google Scholar] |
| 11. | Akbarnia BA, Pawelek JB, Cheung KM, Demirkiran G, Elsebaie H, Emans JB, et al. Traditional growing rods versus magnetically controlled growing rods for the surgical treatment of early-onset scoliosis: A case-matched 2-year study. Spine Deform 2014;2:493-7. [Google Scholar] |
| 12. | Thompson W, Thakar C, Rolton DJ, Wilson-MacDonald J, Nnadi C. The use of magnetically-controlled growing rods to treat children with early-onset scoliosis: Early radiological results in 19 children. Bone Joint J 2016;98-B:1240-7. [Google Scholar] |
| 13. | Wimmer CS, Pfandlsteiner T, Siam AE. Preliminary results of treatment of early onset scoliosis using magnetic growing rods. Ann Orthop Rheumatol 2017;5:1077. [Google Scholar] |
| 14. | Keskinen H, Helenius I, Nnadi C, Cheung K, Ferguson J, Mundis G, et al. Preliminary comparison of primary and conversion surgery with magnetically controlled growing rods in children with early onset scoliosis. Eur Spine J 2016;25:3294-300. [Google Scholar] |
| 15. | Cheung JP, Cahill P, Yaszay B, Akbarnia BA, Cheung KM. Special article: Update on the magnetically controlled growing rod: Tips and pitfalls. J Orthop Surg (Hong Kong) 2015;23:383-90. [Google Scholar] |
| 16. | Roussouly P, Nnadi C. Sagittal plane deformity: An overview of interpretation and management. Eur Spine J 2010;19:1824-36. [Google Scholar] |
| 17. | Lebon J, Batailler C, Wargny M, Choufani E, Violas P, Fron D, et al. Magnetically controlled growing rod in early onset scoliosis: A 30-case multicenter study. Eur Spine J 2017;26:1567-76. [Google Scholar] |
| 18. | Skov ST, Wijdicks SPJ, Bünger C, Castelein RM, Li H, Kruyt MC. Treatment of early-onset scoliosis with a hybrid of a concave magnetic driver (magnetic controlled growth rod) and a contralateral passive sliding rod construct with apical control: Preliminary report on 17 cases. Spine J 2018;18:122-9. [Google Scholar] |
| 19. | Figueiredo N, Kananeh SF, Siqueira HH, Figueiredo RC, Al Sebai MW. The use of magnetically controlled growing rod device for pediatric scoliosis. Neurosciences 2016;21:17-25. [Google Scholar] |
Fulltext Views
2,292
PDF downloads
1,049





