Translate this page into:
Musculoskeletal hydatid disease of extremities: A topical mini-review of recent articles
Corresponding Author:
Ganesh S Dharmshaktu
Department of Orthopaedics, Government Medical College, Haldwani - 263 139, Uttarakhand
India
drganeshortho@gmail.com
| How to cite this article: Dharmshaktu GS, Adhikari N, Mourya P. Musculoskeletal hydatid disease of extremities: A topical mini-review of recent articles. J Musculoskelet Surg Res 2020;4:182-186 |
Abstract
Hydatid disease is an uncommon but important parasitic infection that presents itself with various clinical problems. It is reported from both endemic and nonendemic regions. Its common presentation may be either an asymptomatic mass or site-specific symptoms that pose a diagnostic or treatment challenge. More articles are added in the medical literature about this disorder every passing year but mostly limited to sporadic case reports or small series. Consensus on the diagnostic approach and management guidelines is nonexistent owing to the rarity of the condition. An attempt has been made in this article to highlight relevant information from published articles in the last 5 years (the year 2015 onward) on the subject. This article is aimed to serve as a brief overview of the recent updates for general clinicians and orthopedists alike.
Introduction
The musculoskeletal affliction of hydatid disease (HD), a zoonosis, is an uncommon entity with only 1%–2% of cases of all hydatid infestations.[1] It is also referred to as cystic echinococcosis (CE) or hydatidosis in the literature. The causative agents of HD are two tapeworm species, either larva of Echinococcus granulosus, that is usually a unilocular form, and Echinococcus multilocularis, that is usually an alveolar form. The former is more common, while the latter produces a more serious disease with respect to clinical presentation. Extremity involvement is less common in cases with musculoskeletal involvement, with approximately 60% of cases being reported to involve large nonextremity bones such as spine, pelvis, and only 28% with long bone involvement followed by ribs and scapula.[2] This disease displays overall low prevalence as most series spanning long period also describe cases that are only a handful. A 17-year-study described 15 cases of primary musculoskeletal HD, without associated involvement of other sites and were diagnosed only on histology following the surgery.[3] Bone CE is the rarest form and has no expert consensus on treatment along with gross heterogeneity in diagnostic approaches, leading to morbidity and complications in many cases. Complications noted in a recent systematic review of published literature, involving 32 cases with skeletal CE, were nerve compression (47%) followed by infection and pathological fracture in 31% of cases each.[4]
A brief overview of recent updates is presented here following a literature review of representative cases. The literature search in the PubMed (www.ncbi.nlm.gov/pmc) for the search query “Musculoskeletal” and “Hydatid disease,” “Hydatid disease,” and “Bone” with filter for articles in the last 5 years resulted in 116 articles (during the period of May 4–7, 2020). PubMed central articles were included to gain open-access reading and assessment of individual articles. Articles with nonextremity involvement such as pelvis, near major joints, spine, intra-abdominal organs, and head-and-neck region were excluded. In cases with multiple reports of similar sites and presentations, only the more recent one was included. The bone involvement in the metaphyseal area and not involving joints was included in one case. The authors also believe that not all published articles can be claimed to be cited due to want of space and relevance.
Bones
Although males are more commonly involved in older literatures, Tekin et al. reported female preponderance in their series of 22 cases (15 females) and reported the thigh along with the paravertebral region as the most common sites.[5] In one case, a huge buttock swelling was later identified with underlying iliac bone destruction owing to localized HD involvement. The size of the swelling resembled a neoplastic lesion, and the case highlights the importance of putting HD as a differential in a case of lump.[6] Fracture nonunion, as a rare complication of a case of subtrochanteric fracture with a final diagnosis of HD, was reported and managed with a cephalomedullary nail.[7] Another interesting case of a 5-year-old nonunion femur fracture with discharging sinus who was even given anti-tubercular therapy with little improvement was found to result from HD. Sample following sequestrectomy and saucerization of the nonunion site led to a final diagnosis of HD.[8] A femoral condyle lesion with minimally displaced fracture managed with internal fixation is reported in one case.[9] Things get complicated when the entire humerus is involved and requires radical surgery and implantation.[10] Oncological resection of the entire humerus and replacement with customized noncemented prosthesis was done, and abductors and other soft tissues were attached into the prosthesis. Ulna involvement has also been reported.[11] The bony involvement with peri-prosthetic infection, loosening, and a fracture below a total-knee arthroplasty implant due to CE below the tibial stem was recently reported and managed with staged interventions.[12] In a recent series, long bone involvement was found in three out of a total of eight cases with skeletal CE from the endemic region of Kazakhstan. Humerus, femur, and tibia were involved in extremity bones, while the rest were pelvis and spine cases.[13] Scaphoid bone involvement with HD was recently reported in a case with proximal pole cyst initially diagnosed as a simple bone cyst. Curettage and bone allograft were done with no recurrence noted in follow-up.[14]
Muscles/soft Tissues
Thigh region with abundant muscle tissues is commonly affected in HD, but small lumps may also undergo delayed identification and diagnosis.[15] Careful clinical suspicion is important in these region. Adductor magnus muscle involvement is reported in one case.[16] Medial elbow soft-tissue growth and biceps brachii muscle involvement are reported in two separate cases as upper extremity soft-tissue affliction.[17],[18] Pectoralis major involvement as infraclavicular anterior chest growing mass has also been reported.[19] Rarely, the muscle involvement may be part of multifocal involvement as in one case with trapezius muscle involvement, which had concomitant triple site involvement of right lung and liver.[20]
Vastus lateralis muscle involvement in isolation has also been reported.[21] Enlarging mass of CE may have complications such as rupture, compression of adjacent structures, or rarely infection. A case of incidental finding of infected cyst noticed during surgery of a thigh mass has been reported.[22] A forearm mass below flexor digitorum superficialis and adherent to flexor digitorum profundus and the median nerve was reported and was excised with care to prevent its rupture or iatrogenic nerve injury.[23] The dissection, in selected cases, may be avoided if the cyst is in a difficult location or adjacent to a neurovascular structure like in one case of tibialis posterior cyst that was drained and injected with scolicidal agents for being too close to the posterior tibial pedicles and excision was deferred.[24]
The cystic and multilobular appearance of HD within muscle tissue in the imaging may at times be confused with some lesion of vascular origin such as hemangioma. One case of pectoralis minor involvement with imaging diagnosis of cystic lymphangioma and final histopathological diagnosis of HD was reported recently.[25] Calf muscle involvement with painless lump is another uncommon localization of HD.[26] Gluteal muscle lump is frequently reported in the literature underlining the importance of its anticipation and knowledge, especially in the endemic regions.[27] Sole of the foot with a clinical diagnosis of foot callus was planned for minor excision which intraoperatively revealed daughter cysts resembling HD.[28] Biceps femoris muscle involvement with painful growing mass along with associated liver cyst was reported recently. Cystectomy of muscle mass was done while the smaller liver cyst was left and treated with pharamacotherapy.[29]
Investigations and Treatment
The judicious use of fine-needle aspiration cytology and cell block method as an important method at unusual locations was underlined in one case of osseous HD mimicking fibrous dysplasia.[30] Immuno-diagnosis (immunoelectrophoresis and immunoblotting) and serology can be instrumental in the diagnosis of HD despite current pitfalls and challenges.[31] The performance data and best reliable serological test are still uncertain, despite many newer tests added in the kitty, highlights research need in this area. Low sensitivity, cross reactivity to other antigens, and lack of standardization across laboratories may be other reasons that demand remedial measures. Development and validation of newer antigen-based tests or the use of recombinant antigen with promising potential should be explored in future for better diagnostic kits.[31]
An extensive oncological approach, as used to treat a locally malignant tumor, is preferred surgical intervention. Complete removal of cysts is critical to prevent a recurrence. Aggressive wide resection and anti-helminthic therapy is the mainstay of the treatment. The complications include hematoma, superficial or deep infection, and, in rare cases, repeat surgical exploration.[32] Puncture, aspiration, injection, and re-aspiration technique was used with good outcome in a series from Sudan.[33] This method can be used in limited resources settings as a treatment option. Recurrence is a dreaded complication, and a case report of recurrence in the form of painful erythematous lesion of the thigh, after 13 years of surgical treatment, was reported at the same site.[34]
Radiotherapy (RT) as an adjunct to conventional treatment has been tried in one retrospective series of 40 cases (16 opted for RT and 24 for surgery) over 11 years, which concluded that relapses and antibody titers were lower and patient satisfaction was higher in RT group, but the need for better trials in future was advocated.[35] Experts believe that studies on RT, though encouraging, have many shortcomings to this date, and successfully planned and executed clinical trials with long-term follow-up data can only provide sufficient evidence in this regard.[36]
As many HD cases may mimic tumors in clinical features, they require relevant radiology and histological opinion for diagnosis. In a small series of five cases resembling tumors, three cases involving the pelvis and one each in femur and thigh were managed and finally diagnosed as HD. Treatment ranged from simple debridement, bone cementing with or without implant fixation, hip arthrodesis, hemipelvic replantation with femoral prosthesis, and distal femur endoprosthetic replacement.[37] Many times, endoprosthesis and allograft prosthetic composites, though, promising options, are not viable due to availability, technical demand, limited resources, and cost factors. Massive allograft use may be an alternative in such circumstances as described in two cases with extensive femoral destruction managed with this technique and showing successful follow-up at 5 and 9 years.[38] If the operation risks and outcomes do not guarantee a well-functioning limb, amputation may be a sound option. In an exhaustive review about osseous CE, the authors concluded that therapies should be aimed at disease control and complication prevention and not solely on curative surgeries.[39]
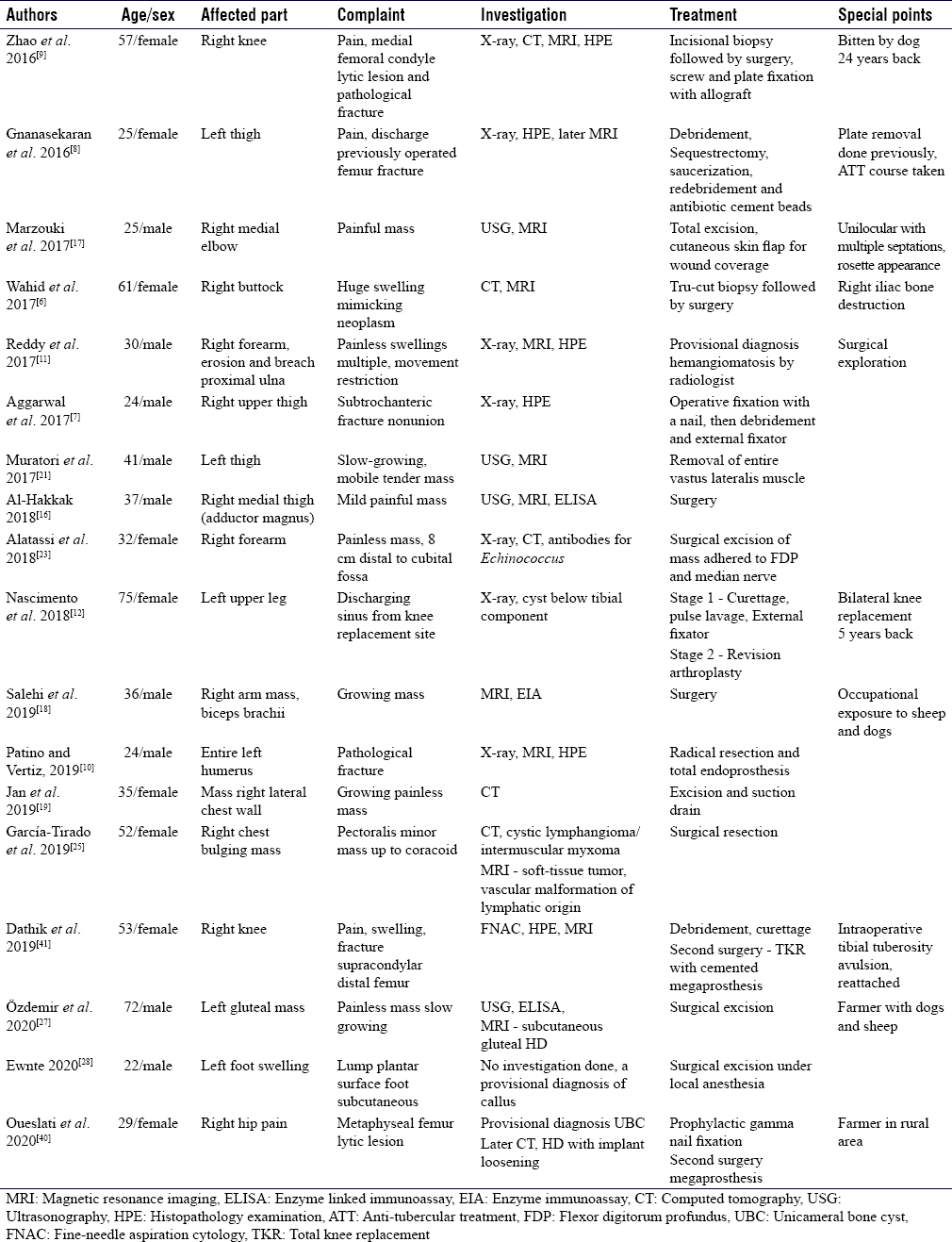
A case of proximal femur lytic lesion, initially managed with prophylactic cepahlomedullary nailing, was followed by recurrence of pain and tumefaction. Lysis of trochanteric region and subsequent implant loosening was again managed with repeat surgery. Biopsy and wide excision followed by the use of megaprosthesis were done leading to a good outcome.[40] Another case of a pathological fracture of distal femur was managed by cemented megaprosthesis 1 month after debridement and curettage of the lesion.[41] Tumor megaprosthesis can be instrumental in select cases with diffuse involvement. A few recent representative cases with relevant details are described in a tabulated form for an easy read [Table - 1].
Conclusion
Many cases of HD are added into the existing literature affecting unusual locations and with unusual presentations. This article is a brief review of recent articles and does not however claim to include all published articles. Visible or palpable mass with or without clinical complaints is the usual feature in the extremities. Clinical suspicion and judicious imaging can result in an appropriate diagnosis and surgical removal in most cases with an excellent outcome in most cases.
Recommendations
The serological and immunological diagnostic technology requires major research impetus for fruitful products such as diagnostic kits for HD. The clinical practice guidelines regarding investigations and management of HD also require evidence-based approach.
Ethical consideration
This is a review article and does not involve patients or patient's information.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
GSD conceived the study and searched the literature, and NA and PM did advanced literature search and prepared the initial draft. GSD critically revised the content and wrote the final draft of the article. All authors critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Resnik D, Niwayama G. Diagnosis of bone and Joint Disorders. 2nd ed. Philadelphia, PA (USA): WB Saunders; 1988. p. 2732-9. [Google Scholar] |
| 2. | Wilner D. Radiology of Bone Tumors and Allied Disorders. 4th ed. Philadelphia, PA (USA): WB Saunders; 1982. p. 114-79. [Google Scholar] |
| 3. | Arazi M, Erikoglu M, Odev K, Memik R, Ozdemir M. Primary echinococcus infestation of the bone and muscles. Clin Orthop Relat Res 2005;432:234-41. [Google Scholar] |
| 4. | Cattaneo L, Manciulli T, Cretu CM, Giordani MT, Angheben A, Bartoloni A, et al. Cystic echinococcosis of the bone: A European multicenter study. Am J Trop Med Hygiene 2019;100:617-21. [Google Scholar] |
| 5. | Tekin R, Avci A, Tekin RC, Gem M, Cevik R. Hydatid cysts in muscles: Clinical manifestations, diagnosis, and management of this atypical presentation. Rev Soc Bras Med Trop 2015;48:594-8. [Google Scholar] |
| 6. | Wahid MA, Ahmed SJ, Gowher HA, Butoo AJ, Ahmed SA, Nabi MG. Musculoskeletal hydatid masquerading as malignancy: A diagnostic dilemma. Afr J Med Health Sci 2017;16:75-6. [Google Scholar] |
| 7. | Aggarwal D, Girotra V, Wadhwa N, Chadha M. Hydatid disease: A rare cause of fracture nonunion. J Family Med Prim Care 2017;6:164-6. [Google Scholar] |
| 8. | Gnanasekaran KK, Prabhu AJ, George S. Osseous hydatidosis of femur in a patient with fracture non-union: An uncommon entity. J Clin Diagn Res 2016;10:ED06-8. [Google Scholar] |
| 9. | Zhao Y, Zinlu Y, Jingbo W, Zhu D, Yu T. Primary hydatid disease in the femoral condyle: A case report. Int J Clin Exp Med 2016;9:14781-6. [Google Scholar] |
| 10. | Patino JM, Vertiz AJ. Hydatidosis of the complete humerus. Treated with radical resection and endoprosthesis. Case report. Int J Surg Case Rep 2019;65:296-300. [Google Scholar] |
| 11. | Reddy IV, Kumar AH, Samorekar B, Babu BA, Mettu AK. Complicated hydatid cyst of ulna – A rare case report. J Clin Diagn Res 2017;11:RD01-3. [Google Scholar] |
| 12. | Nascimento G, Silva C, Marques R, Silva C, Oliveira JF, Santos J, et al. Periprosthetic pathological fracture following tibial echinococcosis: A case report. Int J Surg Case Rep 2018;51:231-6. [Google Scholar] |
| 13. | Manciulli T, Mustapayeva A, Juszkiewicz K, Sokolenko E, Maulenov Z, Vola A, et al. Cystic echinococcosis of the bone in Kazakhstan. Case Rep Infect Dis 2018;2018:9682508. [Google Scholar] |
| 14. | Serbest S, Tiftikci U, Uludag A. Unusual localization of a primary hydatid cyst: Scaphoid bone: A case report. Medicine (Baltimore) 2016;95:e3290. [Google Scholar] |
| 15. | Landolsi M, Kouki S, Abdennadher A. Hydatid cyst of the thigh: A challenging diagnosis. BMJ Case Rep 2017;2017:bcr2017222113. [Google Scholar] |
| 16. | Al-Hakkak SM. Adductor magnus muscle primary hydatid cyst rare unusual site: A case report. Int J Surg Case Rep 2018;51:379-84. [Google Scholar] |
| 17. | Marzouki A, Naam A, Abdulrazak S, Soumare B, Lahrach K, Butayeb F. Musculoskeletal Echinococcus infection as a rare first presentation of hydatid disease: Case report. Patient Saf Surg 2017;11:21. [Google Scholar] |
| 18. | Salehi H, Boroujeni KS, Yaghoubi S. Report of a hydatid cyst case with biceps brachii involvement. Adv Biomed Res 2019;8:23. [Google Scholar] |
| 19. | Jan Z, Zeb S, Shoaib A, Ullah K, Muslim M, Anjum H, et al. Hydatid cyst involving right pectoralis major muscle: A case report. Int J Surg Case Rep 2019;58:54-6. [Google Scholar] |
| 20. | Aljasem H, Almess M, Bakgagi M. Multi-sited hydatid cystic disease with muscular involvement in a young female: A case report from Syria. Int J Surg Case Rep 2017;35:73-6. [Google Scholar] |
| 21. | Muratori F, de Gori M, D'Arienzo A, Bettini L, Roselli G, Campanacci DA, et al. Hydatid cyst in the vastus lateralis muscle: A case report. Clin Cases Miner Bone Metab 2017;14:262-4. [Google Scholar] |
| 22. | Tahir AM, Bahjat AS, Mohammed AA. Primary infected hydatid cyst of the thigh in a young lady; case report with literature review. Ann Med Surg (Lond) 2019;47:32-5. [Google Scholar] |
| 23. | Alatassi R, Koaban S, Alshayie M, Almogbil I. Solitary hydatid cyst in the forearm: A case report. Int J Surg Case Rep 2018;51:419-24. [Google Scholar] |
| 24. | Ouakrim R, Amziane Z, Younes O, Eloukili I, Kharmaz M, Lamrani MO, et al. Locally recurrent subcutaneous and muscular hydatid cysts of the leg: An unusual case report. Pan Afr Med J 2015;21:282. [Google Scholar] |
| 25. | García-Tirado J, Allué-Cabañuz M, Muñoz-González N, Viso-Soriano MJ, Marquina-Ibáñez I. Cystic lesion of pectoralis minor muscle: Learning from mistakes. Autops Case Rep 2019;9:e20180780. [Google Scholar] |
| 26. | Mohammed AA, Arif SH. Hydatid cyst of the calf presenting as painless mass: A case report. Int J Surg Case Rep 2019;60:273-5. [Google Scholar] |
| 27. | Özdemir M, Kavak RP, Kavak N, Akdur NC. Primary gluteal subcutaneous hydatid cyst. IDCases 2020;19:e00719. [Google Scholar] |
| 28. | Ewnte B. Hydatid cyst of the foot: A case report. J Med Case Rep 2020;14:6. [Google Scholar] |
| 29. | Seyedsadeghi M, Arabzadeh A, Habibzadeh A. A case of hydatid cyst in biceps femoris. Int J Surg Case Rep 2020;66:107-9. [Google Scholar] |
| 30. | Hui M, Tandon A, Prayaga AK, Patnaik S. Isolated musculoskeletal hydatid disease: Diagnosis on fine needle aspiration and cell block. J Parasit Dis 2015;39:332-5. [Google Scholar] |
| 31. | Sarkari B, Rezaei Z. Immunodiagnosis of human hydatid disease: Where do we stand? World J Methodol 2015;5:185-95. [Google Scholar] |
| 32. | Erol B, Onay T, Çalışkan E, Okay E. Oncological approach with antihelminthic chemotherapy and wide resection in the treatment of musculoskeletal hydatidosis. A review of 10 cases with mean follow-up of 64 months. Acta Orthop Belg 2015;81:530-7. [Google Scholar] |
| 33. | Foad AF, Satir AA. Skeletal manifestation of hydatid cystic disease in Sudan. J Taibah Univ Med Sci 2018;13:564-71. [Google Scholar] |
| 34. | Barkati S, Butler-Laporte G, Ndao M, Ajise OK, Semret M, Yansouni CP, et al. A recurrent hydatid cyst of the thigh diagnosed 13 years after initial presentation. IDCases 2018;11:12-5. [Google Scholar] |
| 35. | Xie Z, Chen L, Xiue Q, Bao Y, Luo X, Yi C, et al. Surgery or radiotherapy for the treatment of bone hydatid disease: A retrospective case series. Int J Infectious Dis 2015;33:114-9. [Google Scholar] |
| 36. | Neumayr A. Radiotherapy of osseous echinococcosis: Where is the evidence? Int J Infect Dis 2015;33:75-8. [Google Scholar] |
| 37. | Toǧral G, Arıkan ŞM, Ekiz T, Kekeç AF, Ekşioǧlu MF. Musculoskeletal hydatid cysts resembling tumors: A report of five cases. Orthop Surg 2016;8:246-52. [Google Scholar] |
| 38. | Muscolo DL, Zaidenberg EE, Farfalli GL, Aponte-Tinao LA, Ayerza MA. Use of massive allografts to manage hydatid bone disease of the femur. Orthopedics 2015;38:e943-6. [Google Scholar] |
| 39. | Monge-Maillo B, Tojeiro SC, López-Vélez R. Management of osseous cystic echinococcosis. Expert Rev Anti Infect Ther 2017;15:1075-82. [Google Scholar] |
| 40. | Oueslati A, Amri K, Chefi MA, Mallat Y, Znagui T, Nouisri L. Hydatid disease of proximal femur treated using a mega prosthesis: A case report. Int J Surg Case Rep 2020;68:67-73. [Google Scholar] |
| 41. | Dathik S, Chopra RK, Talwar J, Pheroz M, Prasad R. Primary hydatidosis of distal femur masquerading malignancy – A rare case. J Clin Orthop Trauma 2019;10:213-20. [Google Scholar] |
Fulltext Views
1,825
PDF downloads
300





