Translate this page into:
Prone or lateral patient positioning in KocherLangenbeck approach in acetabular fractures fixation: A systematic review and meta-analysis
*Corresponding author: Ghalib Ahmed, Department of Orthopedic Surgery, Hamad Medical Corporation, Doha, Qatar. gahmed@hamad.qa
-
Received: ,
Accepted: ,
How to cite this article: Hantouly AT, Salman LA, Toubasi AT, Alzobi O, Alborno Y, Kayali H, et al. Prone or lateral patient positioning in KocherLangenbeck approach in acetabular fractures fixation: A systematic review and meta-analysis. J Musculoskelet Surg Res, 2023;7:225-34.
Abstract
The Kocher-Langenbeck (K-L) approach is the approach of choice to treat fractures involving the posterior acetabulum. It provides direct exposure to the acetabulum, adequate reduction, and access to treat associated hip fractures. However, there is no consensus on the positioning of the patient; prone or lateral. This review aimed to investigate the effect of patient positioning on the outcomes of the K-L approach in acetabular fracture fixation. Cochrane, Web of Science, Google Scholar, and PubMed were searched from inception until February 22, 2022. Inclusion criteria encompassed studies that investigated acetabular fracture fixation utilizing the K-L approach in relation to patient positioning (Prone and/or Lateral). Only English manuscripts that reported at least one of the outcomes of interest were included in the study. Studies that utilized both positions without specifying the outcomes in relation to the patient position were excluded from the study. The Newcastle–Ottawa Scale and the Joanna Briggs Institute tool were utilized to assess the quality of the included studies. This study included 521 patients from six articles. Of those patients, 46.1% were operated on in the lateral position and 53.9% in the prone position. The mean operative time of lateral and prone positions was 160.9 min (95% confidence intervals [CI]: 135.11–186.64) and 212.5 min (95% CI: 167.08–257.94), respectively. The mean blood loss in the lateral position was 502.mL (95% CI: 471.61–532.47) compared to 482.5 mL (95% CI: 396.77–568.28) in the prone position. The pooled complications in the lateral position were 29% (95% CI: 19–39%) compared to 37% (95% CI: 6–75%) in the prone position. The outcomes did not significantly differ when comparing lateral and prone patient positioning for posterior acetabular fracture fixation through the K-L approach. Further prospective randomized controlled studies are recommended to reach the best evidence.
Keywords
Acetabulum
Internal fixation
Kocher-Langenbeck
Lateral
Prone
INTRODUCTION
Acetabular fractures, which are caused by high-energy trauma like falls from height and motor vehicle collisions, result in severe and debilitating injuries.[1] Such injuries are associated with osseocartilaginous and musculoligamentous disruptions that affect the congruity of the hip joint.[2] The long-term results of treating such injuries depend on the fracture type, concomitant dislocation, femoral head injury, chondral injury, and, most importantly, reduction quality.[3] Therefore, the aim of treating such injuries is to achieve an anatomical reduction of the hip joint to prevent the potentially debilitating consequences of stiffness, persistent pain, and subsequent arthritis.[2] The gold standard for managing displaced acetabular fractures, particularly those affecting the weight-bearing region, is open reduction and internal fixation (ORIF). However, as there is no single approach to provide adequate exposure to both acetabular columns and pelvic interiors, the surgical approach depends on the fracture pattern that is classified according to Judet Letournel’s classification.[4] Kocher-Langenbeck (K-L) approach is the approach of choice to treat fractures involving the posterior acetabular element as it provides direct exposure to the acetabulum, adequate reduction, and access to treat associated hip fractures.[5] This approach and its modifications and variations are well described in the literature, but with no consensus on the positioning of the patient; prone or lateral. Thus, this study aimed to investigate the impact of patient positioning on the outcomes of the K-L approach in acetabular fracture fixation.
MATERIALS AND METHODS
Search strategy
A systematic search was conducted following the Preferred Reporting Items of Systematic Reviews and Meta-analysis recommendation on Cochrane, Web of Science, Google Scholar, and PubMed databases.[6] The databases were searched from inception till February 22, 2022, to obtain all the articles investigating the impact of patient positioning on the outcomes of the K-L approach in acetabular fracture fixation. Moreover, to ensure the inclusion of all eligible studies, a manual search for eligible studies was done through the review articles and by searching the references of the eligible articles.
The search used the following keywords: Lateral OR Prone AND Acetabulum AND Fracture AND “posterior approach” OR Kocher-Langenbeck OR K-L. Two authors independently performed a blinded screening of titles and abstracts, followed by a comprehensive evaluation of the full texts of eligible articles by the same two authors, and any discrepancy was discussed with a senior author to reach an agreement.
Eligibility criteria
Studies that investigated acetabular fracture fixation utilizing the K-L approach in relation to patient positioning were included if they met the inclusion criteria below.
All studies investigating acetabular fracture fixation using the K-L approach include prospective studies, retrospective studies, cohorts, case–control, and case series
Reporting at least one of the outcomes of interest
Accessible articles that were published in English
No restrictions for study design or follow-up period.
Exclusion criteria
Studies that did not mention patient positioning were excluded from the study. We also excluded studies that utilized both positions (prone and lateral) without specifying the outcomes in relation to patient positioning. Cadaveric studies, technical studies, abstracts, case reports, inaccessible full-text, and abstracts were also excluded from the study.
Data extraction process and data items
The data of the included studies were extracted by two authors independently. The collected data were compared to reach an agreement in case of any discrepancy.
The following data items were collected: Study year, author’s name, country of origin, participants number, sex, age, intraoperative blood loss, operative time, quality of reduction, admission-to-operation time, and complications (Major complications, including infection, neurologic injury, progression to post-traumatic arthritis, femoral head avascular necrosis, thromboembolism, dislocation, non-union, and need for further surgeries. Minor complications included heterotopic ossification, prolonged wound healing, hematoma, and seroma).
Data synthesis
The primary outcomes were operative time. The secondary outcomes were quality of reduction, blood loss, and complication rate.
Risk of bias in individual studies
Two authors used the Newcastle–Ottawa Scale (NOS) independently to evaluate the quality of the cohort studies. NOS has three main domains: selection, comparability, and outcome. The maximum scores for these domains are four, two, and three, respectively.[7] To evaluate the risk of bias in the case series articles, two authors utilized the Joanna Briggs Institute (JBI) tool independently. JBI is a checklist of ten questions that assess the study’s quality, considering its design, conduct, and analysis.[8] Any disagreement between the two authors assessing the included studies’ quality was resolved by consulting a senior author.
Statistical analysis
Mean and standard deviation (SD) were analyzed for continuous outcomes, and whenever median and interquartile were encountered, they were converted to mean and SD using the Wan et al. method.[9] The effect size was weighted mean difference (WMD) and its related 95% CI for continuous outcomes, whereas it was relative risk (RR) and its related 95% CI for binary outcomes. The effect size of the rates of the events was the prevalence with its related 95% CI. The studies were pooled using the random effect model if I2 was >50%, whereas they were pooled using the fixed effect model when I2 was <50%. The heterogeneity of the included studies was assessed using Cochrane Q statistic and I2. The analysis was done using Meta XL, version 5.3 (EpiGear International, Queensland, Australia).
RESULTS
Search results
After searching, a total of 263 articles were retrieved. Of these, 33 duplicate articles were identified and eliminated manually and electronically. The remaining 230 articles were screened using the titles and abstracts, leading to the exclusion of 200 articles as they did not meet the eligibility criteria. A full-text screening was performed for the remaining 30 articles, and another 24 articles were excluded for not reporting the outcomes of interest, failure to specify the outcomes in relation to patient positioning, and inaccessibility. Three cohorts and three case series were included in this study. The selection process of the studies is described in [Figure 1].

- Search strategy flowchart.
Characteristics of the included studies
The total number of participants included in this study was 521 patients retrieved from six studies. Two hundred and forty patients (46.1%) underwent ORIF in a lateral position, while 280 patients (53.9%) were positioned in a prone position. The mean age for the patients who underwent ORIF in the lateral and prone positions was 39.8 ± 10.5 and 40.1 ± 13.9, respectively. Regarding sex, 67.5% of the patients who underwent their procedure in the lateral position were male (162/240), whereas 75.8% (213/281) who underwent ORIF in the prone position were male. Moreover, 35.5% (162/375) of the total number of males were operated in the lateral position, while the rest were operated in a prone position [Table 1].
| Study | Magu et al. 2014[3] | Kumar et al. 2021[5] | Shaath et al., 2020[10] | Negrin et al., 2010[11] | Salameh et al., 2020[1] | Collinge et al., 2011[12] | ||
|---|---|---|---|---|---|---|---|---|
| Country | India | India | USA | Austria | Qatar | USA | ||
| Study design | Case series | Case series | Case series | Cohort | Cohort | Cohort | ||
| Number of participants in lateral position (male) |
26 (20) |
80 (48) |
- | 54 (30) |
47 (42) |
33 (22) |
||
| Number of participants in the prone position (male) |
- | - | 172 (129) |
50 (38) |
26 (22) |
33 (24) |
||
| Age (Lateral vs. Prone) |
41.28±7.16 (25–60) |
43.64±13.24 | 43.4 (15–90) | 40.6±11.8 vs. 44±16.7 | 36.3 vs. 34.8 | 36.7 vs. 38.1 | ||
| Fracture classification in prone position | - | - | Posterior wall 73 Posterior wall and column 10 Transverse - Posterior wall 88 T-Type - Posterior wall 1 |
- | Posterior wall 8 Posterior column 0 Posterior wall and column 2 Transverse 1 Transverse - Posterior wall 11 T-Type 4 ACPHT 0 |
Pure transverse 3 Transverse -Posterior wall 22 T-type 8 |
||
| Fracture classification in lateral position | - | Posterior wall 27 Posterior column 16 Posterior wall and column 9 T-Type 9 Transverse 7 Transverse - post wall 7 ACPHT 5 |
- | - | Posterior wall 24 Posterior column 1 Posterior wall and column 7 Transverse 1 Transverse - Posterior wall 11 T-Type 2 ACPHT 1 |
Pure transverse 5 Transverse post wall 18 T-type 10 |
||
| Operative time (Lateral vs. Prone) |
105 (100–120) | 116.38±22.46 | 200.7 (87–518) | 156±47 vs. 157±48 | 184.2±57.5 vs. 241.4±106.7 | 263 (160–472) vs. 258 (156–450) | ||
| Intraoperative blood loss m/L (Lateral vs. Prone) |
- | 503.13±162.91 | 443.2 (175–2100) |
449±337 vs. 410-+310 | 551±299 vs. 584±365 | 532 (300–1500) vs. 644 (200-3000) | ||
| Quality of reduction in lateral position | Anatomic 84.6% Imperfect 15.4% Poor 0% |
Anatomic 60% Imperfect 27.5% Poor 12.5% |
- | Anatomic 57% Imperfect 26% Poor 17% |
Anatomic 68.1% Imperfect 21.3% Poor 10.6% |
Anatomic 41% Imperfect 41% Poor 18% |
||
| Quality of reduction in prone position | - | - | - | Anatomic 72% Imperfect 18% Poor 10% |
Anatomic 44% Imperfect 40% Poor 16% |
Anatomic 60% Imperfect 35% Poor 5% |
||
| Admission-to-surgery time in days (Lateral vs. Prone) |
- | 7.8±2.8 days | - | 4±5 vs. 7±5 | 7.3 (0–34) vs. 7.1 (2–18) | - | ||
| Complications (lateral) |
AVN 3, Morel-Lavallee 1, HO 2, Sciatic nerve injury 1, 1 underwent THA (AVN case included) 0 Deep infection, PE, recurrent dislocation, revision surgery |
Arthritis 11 Myositis ossificans 6 AVN 5 Sciatic nerve palsy 2 Infection 1 |
- | Post-traumatic arthrosis 13, AVN of femoral head 1, Sciatic nerve injury 5, 3 underwent THA, 0 revisions 0 DVT, PE malposition of the implant, hematoma, seroma, non-union, or implant dysfunction |
Sciatic nerve injury 4, infection 3, HO 8 | 3 (2 infections and 1 sciatic nerve injury that recovered completely) | ||
| Complications (Prone) |
- | - | Infection 6, HO 9, recurrent dislocation 1, 1 loss of fixation, 1 arthritis, prolonged wound healing 1, PE 3, death 1, 0 Sciatic nerve injury, 1 removal of the implant due to infection (included in the 6 infection cases), 4 underwent THA. | Post-traumatic arthrosis 10, AVN of head 4, Sciatic nerve injury 4, 5 underwent THA, 6 revisions (2 cases of secondary loss of reduction and four cases of wound infection) 0 DVT, PE, malposition of the implant, hematoma, seroma, non-union, or implant dysfunction |
Sciatic nerve injury 8, infection 5, HO 9 | 2 (2 infections) | ||
ACPHT: Anterior column posterior hemistransverse, THA: Total hip arthroplasty, HO: Heterotopic ossification, PE: Pulmonary embolism, DVT: Deep venous thrombosis, AVN: Avascular necrosis
Quality assessment
Quality assessment is demonstrated in [Tables 2 and 3].
| Study | Selection | Comparability | Outcome |
|---|---|---|---|
| Salameh et al., 2020 | **** | ** | *** |
| Collinge et al., 2011 | **** | ** | * |
| Negrin et al., 2010 | **** | * | *** |
NOS has three main domains: selection, comparability, and outcome. The maximum scores for these domains are four, two, and three, respectively. Each start represents 1 point
| Study question | Kumar et al., 2021 | Shaath et al., 2020 | Magu et al., 2014 |
|---|---|---|---|
| Were there clear criteria for inclusion in the case series? | Yes | No | Yes |
| Was the condition measured in a standard, reliable way for all participants included in the case series? | Yes | Yes | Yes |
| Were valid methods used for the identification of the condition for all participants included in the case series? | Yes | Yes | Yes |
| Did the case series have consecutive inclusion of participants? | UC | Yes | Yes |
| Did the case series have complete inclusion of participants? | UC | Yes | Yes |
| Was there clear reporting of the demographics of the participants in the study? | Yes | Yes | Yes |
| Was there clear reporting of clinical information of the participants? | Yes | No | No |
| Were the outcomes or follow-up results of cases clearly reported? | Yes | Yes | Yes |
| Was there clear reporting of the presenting site (s)/clinic (s) demographic information? | Yes | Yes | Yes |
| Was statistical analysis appropriate? | Yes | Yes | UC |
JBI: Joanna Briggs Institute
Outcomes of the procedure in lateral position
The model that evaluated the operative time in fixation of acetabular fractures in the lateral position included four studies. The overall operative time was 160.9 min (Figure 2; 95% CI: 135.1–186.6); the heterogeneity of this model was significant (P = 0.00, I2 = 99%). Moreover, four studies assessed the intraoperative blood loss during acetabular fracture fixation in the lateral position. Pooling these studies showed that the overall mean blood loss was 502 mL (Supplementary Figure 1; 95% CI: 471.6–532.5); the model also showed insignificant heterogeneity (P = 0.53, I2 = 0%). The models that evaluated the quality of reduction rates in the lateral position included five studies. The model that pooled anatomic reduction rates as per Matta classification showed that the rate was 62% (Supplementary Figure 2; 95% CI: 51–73%); the model showed significant heterogeneity (P = 0.01, I2 = 69%). Furthermore, the model that pooled the imperfect reduction rate as per Matta classification revealed that the rate was 27% (Supplementary Figure 2; 95% CI: 20–34%) with insignificant heterogeneity (P = 0.19, I2 = 34%). In addition, the model that pooled poor reduction rates as per Matta classification showed that the rate was 11% (Supplementary Figure 2; 95% CI: 6–19%); the model had insignificant heterogeneity (P = 0.05, I2 = 58%). Pooling the studies that assessed the complication rate of fixation in the lateral position included five studies. The overall complication rate was 29.6% (Figure 3; 95% CI: 19–39%); the model showed significant heterogeneity (P = 0.02, I2 = 66%). In addition, 76.6% of the overall complication rate was considered major complications.

- Lateral position operative time.
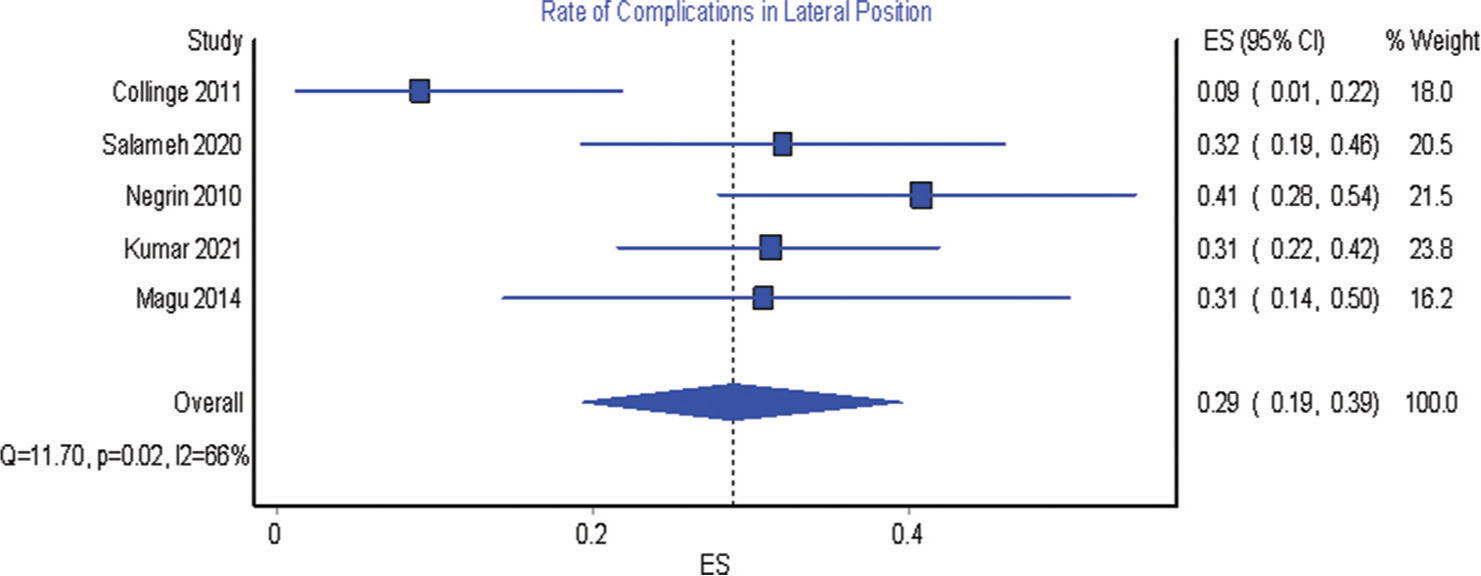
- Rate of complications in lateral position.
Outcomes of the procedure in prone position
The model that assessed the operative time of acetabular fracture fixation in a prone position included four studies. The overall mean operative time was 212.5 min (Figure 4; 95% CI: 167.1–257.9); the model showed significant heterogeneity (P = 0.00, I2 = 95%). Furthermore, four studies evaluated intraoperative blood loss in the prone position. The overall mean blood loss was 482.5 mL (Supplementary Figure 3; 95% CI: 396.8–568.3); the model showed insignificant heterogeneity. The models that assessed the reduction-quality-rate of fixation in the prone position included three studies. The model that pooled the anatomic reduction rate as per Matta classification showed that the rate was 61% (Supplementary Figure 4; 95% CI: 46–75%); the model showed insignificant heterogeneity (P = 0.09, I2 = 58%). The model that evaluated the overall rate of imperfect reduction as per Matta classification showed that the rate was 31% (Supplementary Figure 4; 95% CI: 16–47%); the model also had insignificant heterogeneity (P = 0.05, I2 = 67%). In addition, the model that pooled the rates of poor reduction as per Matta classification showed that the rate was 11% (Supplementary Figure 4; 95% CI: 5–17%) with insignificant heterogeneity (P = 0.53, I2 = 0%). Four studies assessed the complication rate in the prone position. Pooling these studies revealed that the overall complication rate was 37% (Figure 5; 95% CI: 6–75%) with significant heterogeneity (P = 0.00, I2 = 96%).
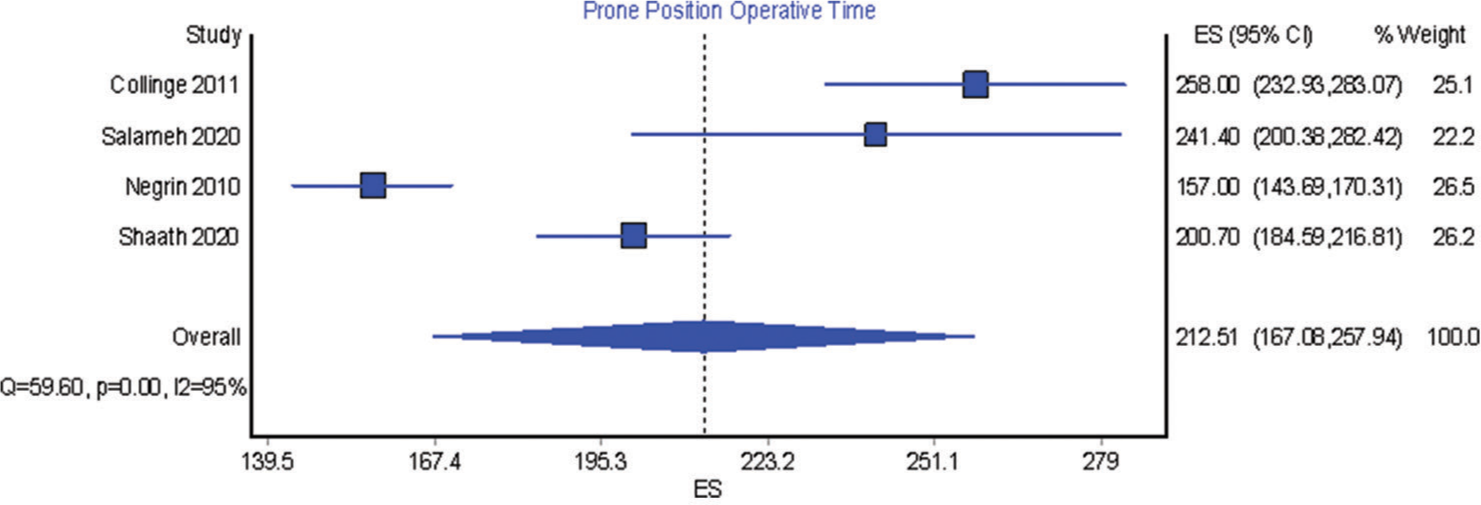
- Prone position operative time.

- Rate of complications in the prone position.
Comparison of the outcomes between lateral and prone positions
The model that compared the lateral and prone positions in regard to the intraoperative blood loss and operative time included three studies. The model that compared the operative time showed no significant difference between the two positions (Figure 6; WMD = −13.6; 95% CI: −45.2–18.0); the model had significant heterogeneity (P = 0.06, I2 = 65%). In addition, the model that compared the intraoperative blood loss showed that there was no significant difference between the two positions (Supplementary Figure 5; WMD = −3.1; 95% CI: −95.7–89.6); the model had insignificant heterogeneity (P = 0.54, I2 = 0%). Furthermore, the model that compared the two positions in regard to quality reduction included three studies. The model that compared anatomic Matta reduction showed an insignificant difference between the two positions (Supplementary Figure 6; RR = 0.93; 95% CI: 0.6–1.4) with insignificant heterogeneity (P = 0.05, I2=68%). Moreover, the model that compared the imperfect Matta reduction rate showed an insignificant difference between the two positions (Supplementary Figure 6; RR = 0.95; 95% CI: 0.5–1.8) with significant heterogeneity (P = 0.09, I2 = 59%). Furthermore, the model that compared poor Matta reduction rate showed an insignificant difference between the two positions (Supplementary Figure 6; RR = 1.42; 95% CI: 0.7–2.9); the model had insignificant heterogeneity (P = 0.31, I2 = 14%). In addition, the model that pooled the studies that reported complication rates included three studies. The model showed no significant difference between the two positions (Figure 7; RR = 0.57; 95% CI: 0.3–1); the model had insignificant heterogeneity (P = 0.07, I2 = 62%).

- Comparison between lateral and prone in operative time (weighted mean difference = lateral-prone).

- Comparison between lateral and prone in the rate of complications.
DISCUSSION
This study aimed to investigate the impact of patient positioning on the outcomes of ORIF of acetabular fractures using the K-L approach. The main findings of this systematic review and meta-analysis showed no significant statistical difference between prone and lateral positions in terms of operative time, intraoperative blood loss, rate of Matta reduction (anatomic, imperfect, and poor), and complication rate.
The K-L approach is commonly utilized for the acetabulum and hip joint. It provides direct visualization and aids in the reduction and fixation of acetabular fractures with posterior and transverse elements.[13-17] Two primary positions, prone and lateral, are described in the literature, and the positioning decision is left to the surgeon’s preference and experience.
While several earlier studies have reported a more favorable operative time in the lateral position,[1,11,12] our current analysis showed an insignificant difference in a direct comparison model. Furthermore, another analysis model of four studies (Salameh et al., Collinge et al., Negrin et al., and Shaath et al.) reported a mean operative time of 212.5 min for the lateral position.[1,10-12] Although the reasons for this occurrences are not explicitly delineated in the literature, this can be partially explained by patient-specific, surgical, and implant-related factors.
Obtaining anatomic reduction is critical in the surgical fixation of acetabular fractures.[15,18] Several complications have been associated with improper reduction, including nerve injury, heterotrophic ossification, malunion and non-union, earlier osteoarthritis, and persistent pain.[19,20] Matta grading system is used frequently to evaluate the quality of fracture reduction in acetabular fractures, and it comprises three grades based on the radiographic residual displacement: anatomic (0–1 mm of residual displacement), imperfect (2–3 mm), or poor (>3 mm).[13] Collinge et al. reported a higher residual fracture displacement in the lateral position cohort, likely due to the impact of gravitational forces placed by the proximal femur on the ischiopubic segment, resulting in poor reduction quality.[12] However, our review has shown no significant difference between both positions regarding Matta anatomic and poor reduction.
Other variables reported in our analysis were consistent with the current literature, demonstrating comparable findings regarding intraoperative blood loss and complication rate across both groups.[1,11,12] Conversely, Negrin et al. reported higher infection and revision rates in patients operated in the prone position; this was linked to the more complex fracture patterns and delayed surgeries encountered in these patients (prone position) cohort.[11]
Limitations
It is important to acknowledge several limitations in this study. First, the limited number of included studies restricts the generalizability of our findings. Second, the lack of adjustment for confounding variables in the included studies introduces the potential for confounding bias. Furthermore, some included studies did not directly compare the outcomes between lateral and prone positions. Moreover, while the included studies reported the overall operative time, they did not provide details on the specific time taken for patient positioning. In addition, a specific analysis of the outcomes based on fracture classification could not be performed. Thus, future large prospective and well-conducted comparative studies are needed. In addition, we found significant heterogeneity across some of the outcomes, which can be explained by the differences between the included studies in fracture classification types and the patient’s demographics. Finally, publication bias was not assessed due to the limited number of studies included in our analysis. However, this is the first systematic review and meta-analysis that analyzes and compares both positions, and the included studies retain the most robust and highest level of evidence currently available in the literature.
CONCLUSION
There was no significant difference in operative time, intraoperative blood loss, rate of Matta reduction (anatomic, imperfect, poor), and complication rate when comparing lateral and prone patient positioning for posterior acetabular fracture fixation through the K-L approach. A further prospective randomized controlled study is recommended to reach the best evidence.
AUTHORS’ CONTRIBUTIONS
AH, LS, and OZ performed the literature search. AH, OZ, and YA collected the data. AH and HK performed a quality assessment. AT performed the statistical analysis. AH, LS, AT, and HK wrote the manuscript. AH and GA supervised the whole work and helped to prepare the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
This article does not contain any studies with human participants performed by any of the authors.
USE OF ARTIFICIAL INTELLIGENCE (AI)- ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
DECLARATION OF PATIENT CONSENT
Patient’s consent is not required as there are no patients in this study.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
Supplementary material available online at
FINANCIAL SUPPORT AND SPONSORSHIP
This study received no specific grant from public, commercial, or not-for-profit funding agencies.
References
- The role of patient positioning on the outcome of acetabular fractures fixation through the Kocher-Langenbeck approach. Eur J Orthop Surg Traumatol. 2021;31:503-9.
- [CrossRef] [PubMed] [Google Scholar]
- Fracture of the acetabulum: A retrospective review of ninety-one patients treated at a single institution. Eur J Orthop Surg Traumatol. 2013;23:155-63.
- [CrossRef] [PubMed] [Google Scholar]
- Long term results after surgical management of posterior wall acetabular fractures. J Orthop Traumatol. 2014;15:173-9.
- [CrossRef] [PubMed] [Google Scholar]
- Acetabulum fractures: Classification and management. Clin Orthop Relat Res. 1980;151:81-106.
- [CrossRef] [Google Scholar]
- Outcome of acetabulum fractures treated with open reduction and internal fixation through Kocher-Langenbeck Approach: A retrospective study. J Clin Orthop Trauma. 2021;23:101599.
- [CrossRef] [PubMed] [Google Scholar]
- Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J Clin Epidemiol. 2009;62:1006-12.
- [CrossRef] [PubMed] [Google Scholar]
- Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603-5.
- [CrossRef] [PubMed] [Google Scholar]
- Systematic reviews of etiology and risk In: Joanna Briggs institute reviewer's manual. Adelaide: The Joanna Briggs Institute; 2017. Ch. 7
- [Google Scholar]
- Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2012;14:135.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical results of acetabular fracture fixation using a focal Kocher-Langenbeck approach without a specialty traction table. J Orthop Trauma. 2020;34:316-20.
- [CrossRef] [PubMed] [Google Scholar]
- Prone or lateral? Use of the Kocher-Langenbeck approach to treat acetabular fractures. J Trauma. 2010;69:137-41.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of radiographic reduction and perioperative complications for transverse acetabular fractures treated by the Kocher-Langenbeck approach: Prone versus lateral position. J Orthop Trauma. 2011;25:538-42.
- [CrossRef] [PubMed] [Google Scholar]
- Acetabular fractures: Anatomic and clinical considerations and current treatment options In: Bucholz RW, Heckman JD, eds. Rockwood and Green's fractures in adults Vol 2. (4th ed). United States: Lippincott-Raven; 1996. p. :1731-866.
- [Google Scholar]
- Surgical management of displaced acetabular fractures: A review. Clin Orthop Relat Res. 1981;151:115-43.
- [CrossRef] [Google Scholar]
- Fractures of the acetabulum: Classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. 1964;46:1615-46.
- [CrossRef] [PubMed] [Google Scholar]
- The Kocher-Langenbeck Approach: State of the Art. JBJS Essent Surg Tech. 2018;8:e18.
- [CrossRef] [PubMed] [Google Scholar]
- KocherLangenbeck approach for posterior wall acetabular fractures. J Orthop Trauma. 2020;34(Suppl 2):S21-2.
- [CrossRef] [PubMed] [Google Scholar]
- Marginal impaction in complex posterior wall acetabular fractures: Role of allograft and mid-term results. Eur J Orthop Surg Traumatol. 2020;30:435-40.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of poor outcome after both column acetabular fractures: A 30-year retrospective cohort study. Patient Saf Surg. 2013;7:9.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes after surgical treatment of acetabular fractures: A review. Patient Saf Surg. 2019;13:16.
- [CrossRef] [PubMed] [Google Scholar]






