Translate this page into:
Surgical solution and clinical outcome for an initially undertreated vaughan-jackson syndrome
2 Spanish Hospital of Mexico, Orthopaedic Surgery Department, Mexico City, Mexico
Corresponding Author:
Efraín Farias-Cisneros
ABC Medical Center - Campus Santa Fe. Av. Carlos Graef Fernandez 154. Torre Central, Office 104-105, Santa Fe. Cuajimalpa 05300, CDMX
Mexico
dr.efrain.farias@gmail.com
| How to cite this article: Farias-Cisneros E, Palafox-Carral I. Surgical solution and clinical outcome for an initially undertreated vaughan-jackson syndrome. J Musculoskelet Surg Res 2020;4:223-227 |
Abstract
Vaughan-Jackson syndrome was described as a progressive rupture of the hand's extensor tendons due to tendon attrition at the wrist. It is frequently associated with osteoarthritis and rheumatoid arthritis. We present a 75-year-old male patient with a painless limitation of the extension of the little finger of the left hand. Initially, he presented a palmar displacement of the left carpus while lifting a heavy object. Vaughan-Jackson syndrome was diagnosed. At first, an end-to-side repair of the affected tendons was performed. Four months later, the patient returned with spontaneous extension lag of the left little and ring fingers. A second surgery was performed with the transfer and reconstruction of extensor tendons with a favorable outcome. Vaughan-Jackson syndrome causes functional impairment and detriment to the quality of life; thus, it is imperative to make an accurate and early diagnosis. Surgical treatment must be done in a timely and appropriate manner. We aim to report the outcome of a patient with an initially undertreated Vaughan-Jackson syndrome, highlighting the necessity of comprehensive treatment of the underlying pathophysiology, to obtain a desirable outcome.
Introduction
Vaughan-Jackson syndrome was first documented in 1948,[1] as a rupture of the extensor tendons of the ring and little fingers secondary to attrition at the level of the distal radioulnar joint (DRUJ) secondary to arthritis.[2] Its worldwide prevalence is unknown, and current knowledge is limited to the case reports. The presence of ulnar head dysplasia and osteophytes leads to a DRUJ capsule perforation, which erodes the fingers' extensor tendons, generally affecting the 4th and 5th extensor compartments and causing a rupture secondary to progressive erosion, more frequently seen in the dominant hand.[3],[4],[5] It begins with the rupture of the extensor digiti quinti proprius tendon (EDQ) and then continues with the rupture of the extensor digitorum communis quintus tendon (EDC-5), then the extensor digitorum communis tendon of the ring finger (EDC-4) and progressively continues with the rupture of the adjacent extensor tendons in an ulnar-radial direction, causing significant functional limitation, for which the definitive treatment is surgery.[1],[2],[3]
This rare and seldom documented syndrome is poorly recognized and understood.[4],[6] The pathophysiology of this disease is not completely understood, but it involves: (a) direct attrition due to prominent bone margins in the DRUJ and ulnar head, (b) chronic inflammatory changes, and (c) hypovascularity at the rupture site.[3],[5],[7] The ulnar translation related to patients with this syndrome is seen in those with traumatic injury to the radiocarpal ligaments, specifically the radioscaphocapitate, and in those with rheumatoid arthritis (RA),[8] nevertheless, in osteoarthritis (OA) patients who develop this syndrome, positive ulnar variance, volar transition of the carpus, and dorsal osteophyte formation have been proposed as associated factors.[5],[9]
This syndrome compromises the quality of life and functionality of the patient since it is a condition that progresses rapidly toward decay and occurs more frequently in the dominant hand, making it imperative to make a correct and early diagnosis.[6] The reason for a timely diagnosis is to prevent further attrition rupture of adjacent tendons.
Surgical treatment consists of the reconstruction and/or transfer of tendons,[10],[11] tendon protection and stabilization,[12] in addition to the resection of the ulnar head and osteophytes in most cases, and if necessary, synovectomy.[9],[13] These anatomical corrections will prevent its progression and restore function.[3] We hereby present a report of a Vaughan-Jackson syndrome case, related to primary DRUJ OA. We aim to show that despite this was an initially undertreated case, the study shows that patients may have a favorable clinical result, after ensuring comprehensive treatment, we also aim to compare it with the previous literature available restricted to case presentations and case series.
Case Report
A 75-year-old male presents with a painless limitation of the extension of the little finger of the left hand for the past 6 weeks [Figure - 1]. Prior to the start of symptoms, he had a mechanism of palmar translation of the left wrist while lifting a heavy object. He mentions having played golf for 20 years, with repeated mild degree left wrist injuries. He has no other significant medical history. The physical examination revealed dorsal prominence of the ulnar head, inability to extend the little finger, and weak extension of the ring finger against resistance, with a palpable mass in the extensor zone 6, suggestive of EDQ rupture. The forearm and wrist presented full range of motion.
 |
| Figure 1: The initial clinical picture of the patient's right hand showing a flexion attitude of the small finger while performing a tenodesis test |
Serum markers and clinical criteria for RA were assessed, the presence of RA was ruled out. Radiographs of the wrist revealed severe DRUJ arthrosis with ulnar head dysplasia and abundant osteophytes [Figure - 2]. Magnetic resonance imaging showed rupture and retraction of the EDQ and EDC-5 of the left hand. Therefore, a Vaughan-Jackson syndrome of the left hand was diagnosed.
 |
| Figure 2: Anteroposterior and oblique views of the right wrist. The findings include ulnar head dysplasia; osteophytes at the ulnar styloid and sigmoid notch are observed |
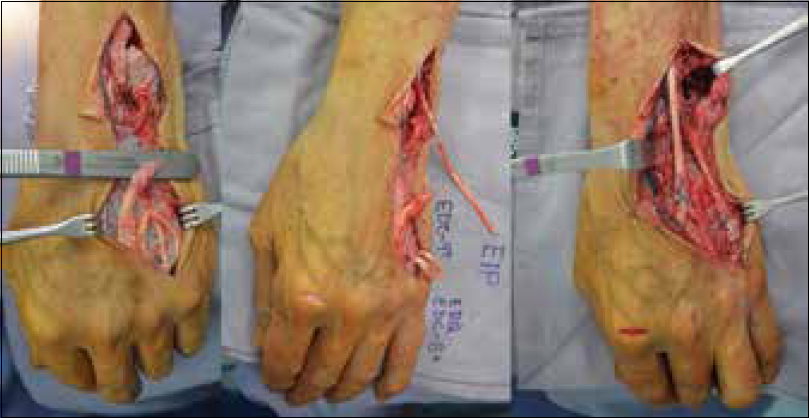
The treatment suggested to the patient consisted of a transfer of extensor indicis proprius tendon (EIP) to the EDQ tendon and excision of the ulnar head, which the patient rejected for cultural reasons. An alternative surgery was accepted consisting of EDQ end-to-end and EDC-5 end-to-side repair with the remaining intact EDC tendons. During the procedure, a complete tear of the EDC-4 was seen, which was missed clinically due to the preservation of the ring finger function. The repair performed was end-to-end EDQ repair, and end-to-side EDC-5 and EDC-4 to the remaining intact EDC. The DRUJ dorsal osteophytes were excised, and a dorsal retinacular flap as interposed between the dorsal capsule and the repaired tendons [Figure - 3].
 |
| Figure 3: Intraoperative pictures showing the affection of the EDQ, and EDC-5 and EDC-4 tendons. The distal radioulnar joint dorsal osteophytes were excised, and a dorsal retinacular flap was interposed between the dorsal capsule and the repaired tendons |
After the surgery, the extensor apparatus function is adequate with full extension of the little finger and progressive improvement in flexion of the ring and little fingers. The only complaint was the inability to make a full fist due to the dorsal stiffness of the little finger [Figure - 4].
 |
| Figure 4: Postoperative clinical pictures after the first surgery. The patient had a functional outcome of the hand, with almost full recovery of the preoperative extension lag |
Four months later, the patient developed spontaneous deterioration in the fingers' function with inability to extend the ring and little fingers. He presented again at the office two months after the newly presented symptoms. The physical examination revealed an absent extension of the ring and little fingers of the left hand.
A new surgery was performed consisting of a reconstruction of EDC-4, EDC-5, and EDQ tendons with tenodesis of EDC-3 to EDC-4 and transfer of EIP to EDC-5 and EDQ left hand [Figure - 5] and the excision of the ulnar head [Figure - 6]a and [Figure - 6]b.
 |
| Figure 5: After exposing the severed tendons, the repair was done using a transfer from extensor indicis proprius tendon to EDQ-EDC-5 and a termino-lateral tenodesis of EDC-4 to EDC-3 |
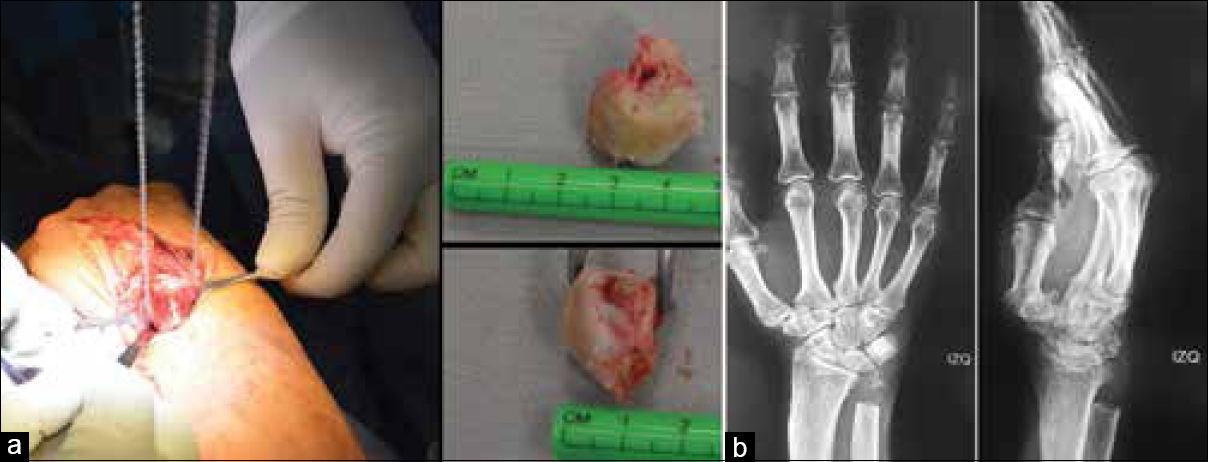 |
| Figure 6: (a) Ulnar head excision was performed with a Gigli saw. The excised ulnar head showed an almost complete loss of cartilage. (b) Radiographic anteroposterior and lateral views after the resection |
After the surgery, the patient had forearm pronation/supination of 70/85°, respectively. Wrist extension/flexion of 70/75, and radial/ulnar deviation of 20/35. He complained of mild ulnar side wrist pain with radiation to the elbow, with an Analog Visual Scale of 2/10. He had a full extension of the metacarpophalangeal (MP), and interphalangeal (IP) joints of the little and ring fingers, and full flexion of the ring finger [Figure - 7], with only partial limitation in flexion of the little finger with a tip-to-palm distance 6 mm lag, due to a loss of flexion at the MP joint of 5° and loss of flexion of 5 more at the proximal IP joint, the distal IP joint had full range of motion. The final patient's follow-up was 12 months after the surgery [Video 1].
 |
| Figure 7: Final clinical pictures showing a full extension of the four ulnar fingers of the right hand, and 5 mm extensor lag of the little finger |
Discussion
Patients with Vaughan-Jackson syndrome have a variable presentation. In the half of the patients, the rupture can present suddenly without previous symptoms like pain or swelling, conflictingly, it may present with a history of DRUJ pain, on the other half. Therefore, the presence or absence of pain, does not rule out or confirm the tendinous involvement.[2],[10],[12] Regardless of the previous nonspecific symptoms, the impairment always starts with weakness and/or inability to extend the little finger due to the EDQ rupture, this being characteristic and suggestive of the syndrome.[1],[3],[9] In our patient, the pain was absent while the chief complaint was the fingers extension deficit, initially the little finger and then the ring finger.
It is well-documented that a progressive deterioration occurs, with initial involvement of the EDQ that later advances toward adjacent tendons in an ulnar-radial direction presenting multiple tendon ruptures in up to 76% of the patients.[13] The tendons progressively move toward the OA site, exposing themselves to greater attrition, which eventually causes subsequent rupture.[11],[13]
Although the etiology is not fully understood, it is evident that the affection of the DRUJ, as well as the presence of osteophytes and ulnar head dysplasia, are crucial in the progression of the syndrome,[9],[10] features also present in our patient. Furthermore, it is classically related to OA and RA tenosynovitis and joint erosion,[4],[6] and although rare, it may be associated with Kienböck disease,[2] Madelung's deformity,[14] carpal boss,[15] microcrystal-related arthropathies such as gout or pseudogout,[16],[17] extravasation of intravenous infusions,[18] and carpal bone fractures.[12] This syndrome compromises the quality of life and functionality of the patient since it progresses rapidly toward deterioration and occurs more frequently in the dominant hand, making it imperative to make a precise and early diagnosis.[19] It predominantly affects older patients,[10],[13],[20] like in this case. However, it can appear in younger patients with avascular necrosis of the lunate or long standing or severe RA.[2],[4]
The repetitive use of the wrist with exercise, work or daily-related activities, and/or forced motion of the wrist or hands is associated with this syndrome.[12],[15] Our patient's long-standing history of golf practice may be related to the underlying OA of the DRUJ, furthermore, he had repetitive wrist injuries that may have contributed to DRUJ arthrosis.[7] The pathophysiology involves direct attrition due to prominent bone margins in the DRUJ and ulnar head; chronic inflammatory changes, and hypovascularity at the rupture site.[4],[5],[21]
Comprehensive surgical treatment consists of the reconstruction and/or transfer of tendons,[9],[11] tendon protection and stabilization,[22] in addition to the resection of the ulnar head and osteophytes in most cases, and if necessary, synovectomy.[13],[23]
The surgical procedure with excision of the ulnar head and tendon transfers chiefly eliminates the cause of the erosion of the tendons and restores the function of the fingers.[4],[11],[24],[25] It has been reported previously that the treatment could be performed without the ulnar head resection, based on the arthritic state of the head, like it was also initially performed in our case.[26] Furthermore, the above-mentioned report has only 2 months of follow-up, and the author still suggests the excision of the ulnar head.[26] In our case, after tendons re-rupture, the ulnar head resection was performed during the second surgery; therefore, the ulnar head excision should be included as part of a comprehensive treatment since it has had excellent results and has been shown to be decisively beneficial if performed on time.[24],[25] Other alternatives should be considered to address the DRUJ pathology, including prosthetic replacement.[4],[27]
A tendon transfer is still the first line of treatment option in tendon rupture, even more so in chronic cases.[11],[25] Alternatives to address the tendon deficit include end-to-end repair and tendon graft reconstruction. End-to-end repair may be an option in acute settings where fibrotic changes have not yet appeared, but tendons may not be viable in chronic lesions due to chronic inflammatory changes. Therefore, end-to-end repair is likely to fail, which was the case in our patient. Grafting appears to have good results, but donor tendons must be available. The harvest must be performed, often in another anatomical region, and in some cases, a long graft must be harvested, while transferred tendons preserve its innate function. Thus, transfer is frequently a better option, especially in the hand, where redundant function tendons are available.[11],[25]
The main limitation of the study is its observational nature, a case presentation has a low level of evidence. This work shows that not all cases go well since the beginning. Since we treat patients and not cases, patient values and opinions are considered; therefore, we respected one of the three pillars of evidence-based medicine. Finally, even though Vaughan-Jackson syndrome is not uncommon, the research available has been restricted to case presentations and case series. One of the strengths of this article is that it highlights the transition of the “classic” Vaughan-Jackson syndrome related to RA that has been decreasing thanks to new disease-modifier therapies, to the “current” more frequent etiology of Vaughan-Jackson syndrome, that is related to primary OA and has seen a worldwide increase due to aging population.
Conclusion
Although rare, Vaughan-Jackson syndrome represents a major cause of closed rupture of the hand's extensor tendons. In addition to conferring limited or abolished extension of the fingers, this condition if untreated progresses toward further impairment, limiting the forearm and wrist function. Therefore, the syndrome's natural history progressively compromises the quality of life and function of the patient.
Recommendations
It is imperative to have a high degree of suspicion to make an accurate and early diagnosis. Since deterioration is inevitable and imminent, we recommend that the surgical treatment should address all the causes intervening in the pathophysiology of the syndrome and may be performed as soon as the diagnosis is made, to improve the functional outcome.
Ethical consideration
The research for this case presentation was conducted in accordance with the 1964 Helsinki Declaration, by its observational nature does not require approval by the Institutional Ethics Committee. The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
EFC and IPC contributed with the concept, design, definition of intellectual content, literature search and manuscript editing. IPC contributed with manuscript preparation. EFC contributed with data acquisition and manuscript review. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Vaughan-Jackson OJ. Rupture of extensor tendons by attrition at the inferior radio-ulnar joint; report of two cases. J Bone Joint Surg Br 1948;30B:528-30. [Google Scholar] |
| 2. | Mazhar T, Rambani R. Vaughan-Jackson-like syndrome as an unusual presentation of Kienböck´s disease: A case report. J Med Case Rep 2011;5:325. [Google Scholar] |
| 3. | Mannerfelt L, Norman O. Attrition ruptures of flexor tendons in rheumatoid arthritis caused by bony spurs in the carpal tunnel. A clinical and radiological study. J Bone Joint Surg Br 1969;51:270-7. [Google Scholar] |
| 4. | Lee SK, Hausman MR. Management of the distal radioulnar joint in rheumatoid arthritis. Hand Clin 2005;21:577-89. [Google Scholar] |
| 5. | Yamazaki H, Uchiyama S, Hata Y, Murakami N, Kato H. Extensor tendon rupture associated with osteoarthritis of the distal radioulnar joint. J Hand Surg Eur Vol 2008;33:469-74. [Google Scholar] |
| 6. | Ohshio I, Ogino T, Minami A, Kato H, Miyake A. Extensor tendon rupture due to osteoarthritis of the distal radio-ulnar joint. J Hand Surg Br 1991;16:450-3. [Google Scholar] |
| 7. | Woo SH, Lee YK, Kim JM, Cheon HJ, Chung WH. Hand and Wrist Injuries in Golfers and Their Treatment. Hand Clin 2017;33:81-96. [Google Scholar] |
| 8. | Pirela-Cruz MA, Firoozbakhsh K, Moneim MS. Ulnar translation of the carpus in rheumatoid arthritis: An analysis of five determination methods. J Hand Surg Am 1993;18:299-306. [Google Scholar] |
| 9. | Cruz-Sánchez M, Pidemunt-Moli G, Cebamanos-Celma J. Rotura espontánea del aparato extensor secundaria a artrosis de la articulación radiocubital distal. Rev Iberoam Cir Mano 2015;43:82-7. [Google Scholar] |
| 10. | Carr AJ, Burge PD. Rupture of extensor tendons due to osteoarthritis of the distal radio-ulnar joint. J Hand Surg Br 1992;17:694-6. [Google Scholar] |
| 11. | O'Sullivan MB, Singh H, Wolf JM. Tendon transfers in the rheumatoid hand for reconstruction. Hand Clin 2016;32:407-16. [Google Scholar] |
| 12. | Barbati A, Geraci A, Borri M, Polidoro F, Di Carlo S, Salini V. Spontaneous rupture of the digital extensor tendons of the hand in unrecognized carpal lunatefracture. Acta Ortop Mex 2017;31:91-4. [Google Scholar] |
| 13. | Gong HS, Lee JO, Baek GH, Kim BS, Kim JY, Lee JS, et al. Extensor tendon rupture in rheumatoid arthritis: A survey of patients between 2005 and 2010 at five Korean hospitals. Hand Surg 2012;17:43-7. [Google Scholar] |
| 14. | Ducloyer P, Leclercq C, Lisfranc R, Saffar P. Spontaneous ruptures of the extensor tendons of the fingers in Madelung's deformity. J Hand Surg Br 1991;16:329-33. [Google Scholar] |
| 15. | Ghatan AC, Carlson EJ, Athanasian EA, Weiland AJ. Attrition or rupture of digital extensor tendons due to carpal boss: Report of 2 cases. J Hand Surg Am 2014;39:919-22. [Google Scholar] |
| 16. | Taniguchi Y, Yoshida M, Tamaki T. Subcutaneous extensor tendon rupture associated with calcium pyrophosphate dihydrate crystal deposition disease of the wrist. J Hand Surg Br 1997;22:386-7. [Google Scholar] |
| 17. | Iwamoto T, Toki H, Ikari K, Yamanaka H, Momohara S. Multiple extensor tendon ruptures caused by tophaceous gout. Mod Rheumatol 2010;20:210-2. [Google Scholar] |
| 18. | Rath S, Bhan S. Oxytocin-induced tenosynovitis and extensor digitorum tendon rupture. J Hand Surg Am 1989;14:847-9. [Google Scholar] |
| 19. | Backdahl M. The caput ulnae syndrome in rheumatoid arthritis. A study of the morphology, abnormal anatomv and clinical picture. Acta Rheumatol Scand Suppl 1963;5:1-75. [Google Scholar] |
| 20. | Tanaka T, Kamada H, Ochiai N. Extensor tendon rupture in ring and little fingers with DRUJ osteoarthritis without perforating the DRUJ capsule. J Orthop Sci 2006;11:221-3. [Google Scholar] |
| 21. | Sivakumar B, Akhavani MA, Winlove CP, Taylor PC, Paleolog EM, Kang N. Synovial hypoxia as a cause of tendon rupture in rheumatoid arthritis. J Hand Surg Am 2008;33:49-58. [Google Scholar] |
| 22. | Rabarin F, Saint Cast Y, Raimbeau G, Césari B, Fouque PA, Jeudy J, et al. “Butterfly flap”: The retinaculum to the rescue of the extensors. Orthop Traumatol Surg Res 2015;101:S207-9. [Google Scholar] |
| 23. | De Smet L. The distal radioulnar joint in rheumatoid arthritis. Acta Orthop Belg 2006;72:381-6. [Google Scholar] |
| 24. | Itsubo T, Uchiyama S, Yamazaki H, Hayashi M, Nakamura K, Kuniyoshi K, et al. Factors affecting extension lag after tendon reconstruction for finger extensor tendon rupture due to distal radioulnar lesion. J Orthop Sci 2016;21:19-23. [Google Scholar] |
| 25. | Moore JR, Weiland AJ, Valdata L. Tendon ruptures in the rheumatoid hand: Analysis of treatment and functional results in 60 patients. J Hand Surg Am 1987;12:9-14. [Google Scholar] |
| 26. | Lozano Moreno FJ. Rupture of extensor tendons due to chronic post-traumatic distal radio-ulnar dislocation. Case report. Acta Ortop Mex 2007;21:96-8. [Google Scholar] |
| 27. | Galvis EJ, Pessa J, Scheker LR. Total joint arthroplasty of the distal radioulnar joint for rheumatoid arthritis. J Hand Surg Am 2014;39:1699-704. [Google Scholar] |
Fulltext Views
7,487
PDF downloads
1,553





